Abstract
Rev Bras Ter Intensiva. 2019;31(1):86-92
DOI 10.5935/0103-507X.20190009
To examine the association between donor plasma cytokine levels and the development of primary graft dysfunction of organs transplanted from deceased donors.
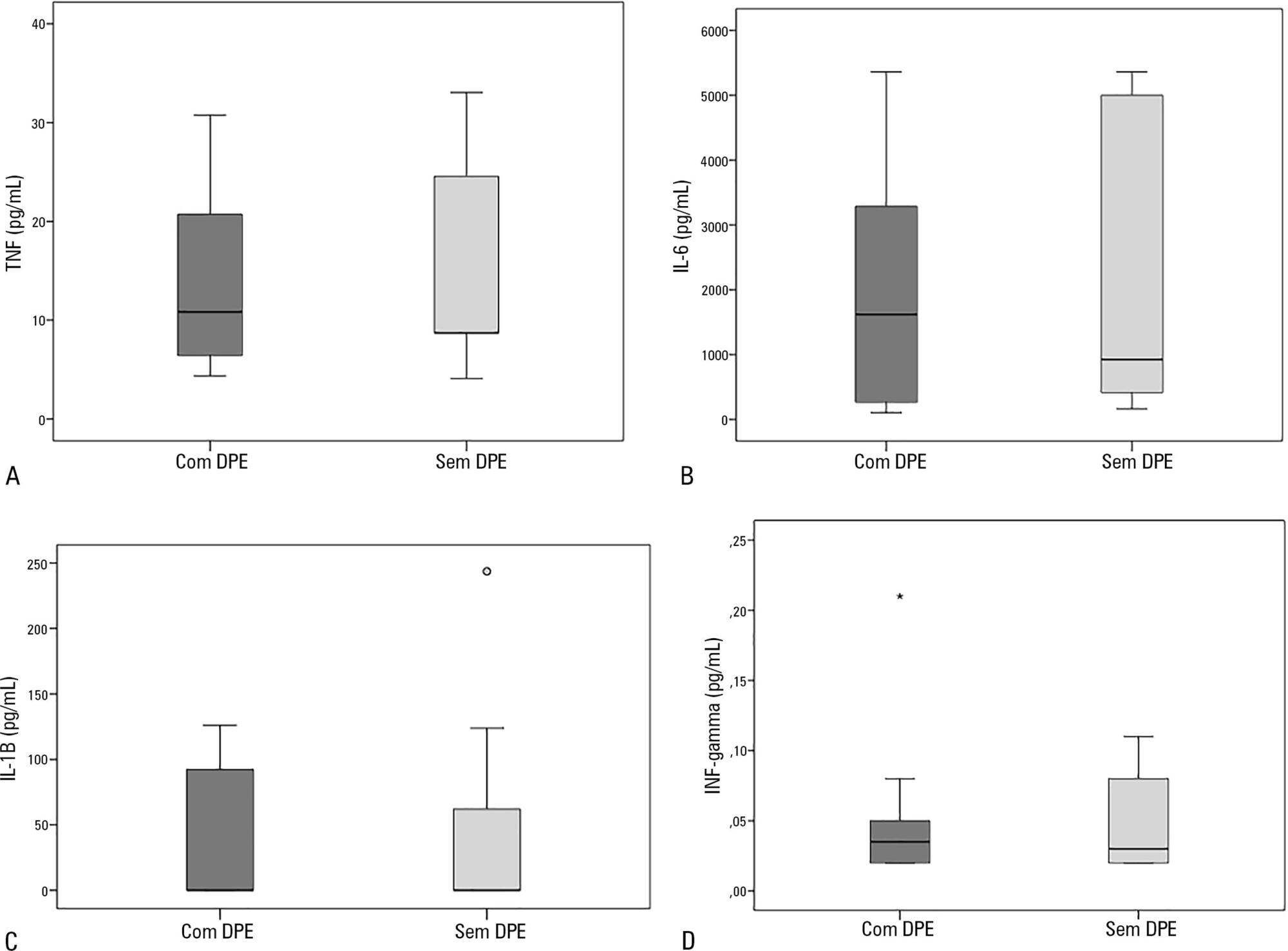
Seventeen deceased donors and the respective 47 transplant recipients were prospectively included in the study. Recipients were divided into two groups: group 1, patients who developed primary graft dysfunction; and group 2, patients who did not develop primary graft dysfunction. Donor plasma levels of TNF, IL-6, IL-1β, and IFN-γ assessed by ELISA were compared between groups.
Sixty-nine organs were retrieved, and 48 transplants were performed. Donor plasma cytokine levels did not differ between groups (in pg/mL): TNF, group 1: 10.8 (4.3 - 30.8) versus group 2: 8.7 (4.1 - 33.1), p = 0.63; IL-6, group 1: 1617.8 (106.7 - 5361.7) versus group 2: 922.9 (161.7 - 5361.7), p = 0.56; IL-1β, group 1: 0.1 (0.1 - 126.1) versus group 2: 0.1 (0.1 - 243.6), p = 0.60; and IFN-γ, group 1: 0.03 (0.02 - 0.2) versus group 2: 0.03 (0.02 - 0.1), p = 0.93). Similar findings were obtained when kidney transplants were analyzed separately.
In this sample of transplant recipients, deceased donor plasma cytokines TNF, IL-6, IL-1β, and IFN-γ were not associated with the development of primary graft dysfunction.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):285-293
DOI 10.5935/0103-507X.20160043
To evaluate the knowledge and acceptance of the public and professionals working in intensive care units regarding organ donation after cardiac death.
The three hospitals with the most brain death notifications in Curitiba were selected, and two groups of respondents were established for application of the same questionnaire: the general public (i.e., visitors of patients in intensive care units) and health professionals working in the same intensive care unit. The questionnaire contained questions concerning demographics, intention to donate organs and knowledge of current legislation regarding brain death and donation after cardiac death.
In total, 543 questionnaires were collected, including 442 from family members and 101 from health professionals. There was a predominance of women and Catholics in both groups. More females intended to donate. Health professionals performed better in the knowledge comparison. The intention to donate organs was significantly higher in the health professionals group (p = 0.01). There was no significant difference in the intention to donate in terms of education level or income. There was a greater acceptance of donation after uncontrolled cardiac death among Catholics than among evangelicals (p < 0.001).
Most of the general population intended to donate, with greater intentions expressed by females. Education and income did not affect the decision. The type of transplant that used a donation after uncontrolled cardiac death was not well accepted in the study population, indicating the need for more clarification for its use in our setting.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):72-76
DOI 10.5935/0103-507X.20150012
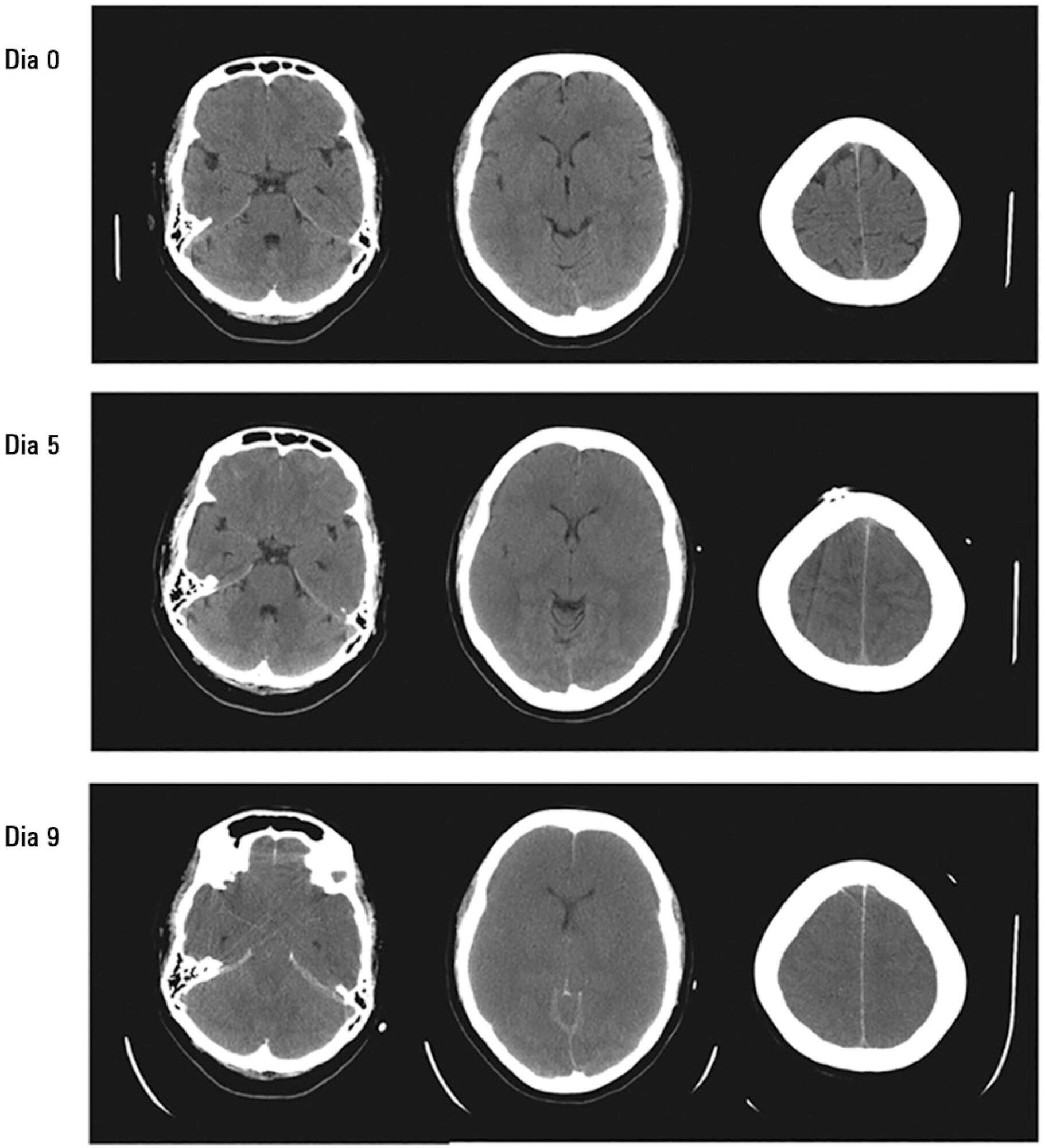
The most important topics in fulminant hepatic failure are cerebral edema and intracranial hypertension. Among all therapeutic options, systemic induced hypothermia to 33 - 34ºC has been reported to reduce the high pressure and increase the time during which patients can tolerate a graft. This review discusses the indications and adverse effects of hypothermia.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):144-148
DOI 10.1590/S0103-507X2008000200005
BACKGROUND AND OBJECTIVES: Failure or delay to diagnose brain death leads to needless occupation of a hospital bed, emotional and financial losses, and unavailability of organs for transplants. The intensive care physician plays an essential role in this diagnosis. This study intended to evaluate intensivists' knowledge concerning brain death. METHODS: Cross-sectional study in 15 intensive care units (ICU) in eight hospitals in the city of Porto Alegre, Brazil. RESULTS: Two hundred forty-six intensivists were interviewed in a consecutive sample between April and December 2005. The prevalence of lack of knowledge regarding the concept was of 17%. Twenty per cent of the interviewees ignored the legal need for complementary confirmatory tests for their diagnosis. Forty-seven per cent considered themselves as having the highest level of assurance to explain the concept to a patient's family members. Twenty-nine per cent erroneously determined the legal time of death for brain dead patients. Pediatric intensivists had less knowledge about the concept, when compared to intensivists for adults (p < 0.001). CONCLUSIONS: Current knowledge of brain death is insufficient in Brazil, among the health care professionals who most often find patients in this situation. Education on the subject is needed to avoid unnecessary expenses, reduce family suffering and increase the offer of organs for transplant.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)