You searched for:"Paulo Roberto Antonacci Carvalho"
We found (7) results for your search.-
Original Article
Effects of critical illness on the functional status of children with a history of prematurity
Rev Bras Ter Intensiva. 2022;34(4):469-476
Abstract
Original ArticleEffects of critical illness on the functional status of children with a history of prematurity
Rev Bras Ter Intensiva. 2022;34(4):469-476
DOI 10.5935/0103-507X.20220429-en
Views1See moreABSTRACT
Objective:
To evaluate the effects of critical illness on the functional status of children aged zero to 4 years with or without a history of prematurity after discharge from the pediatric intensive care unit.
Methods:
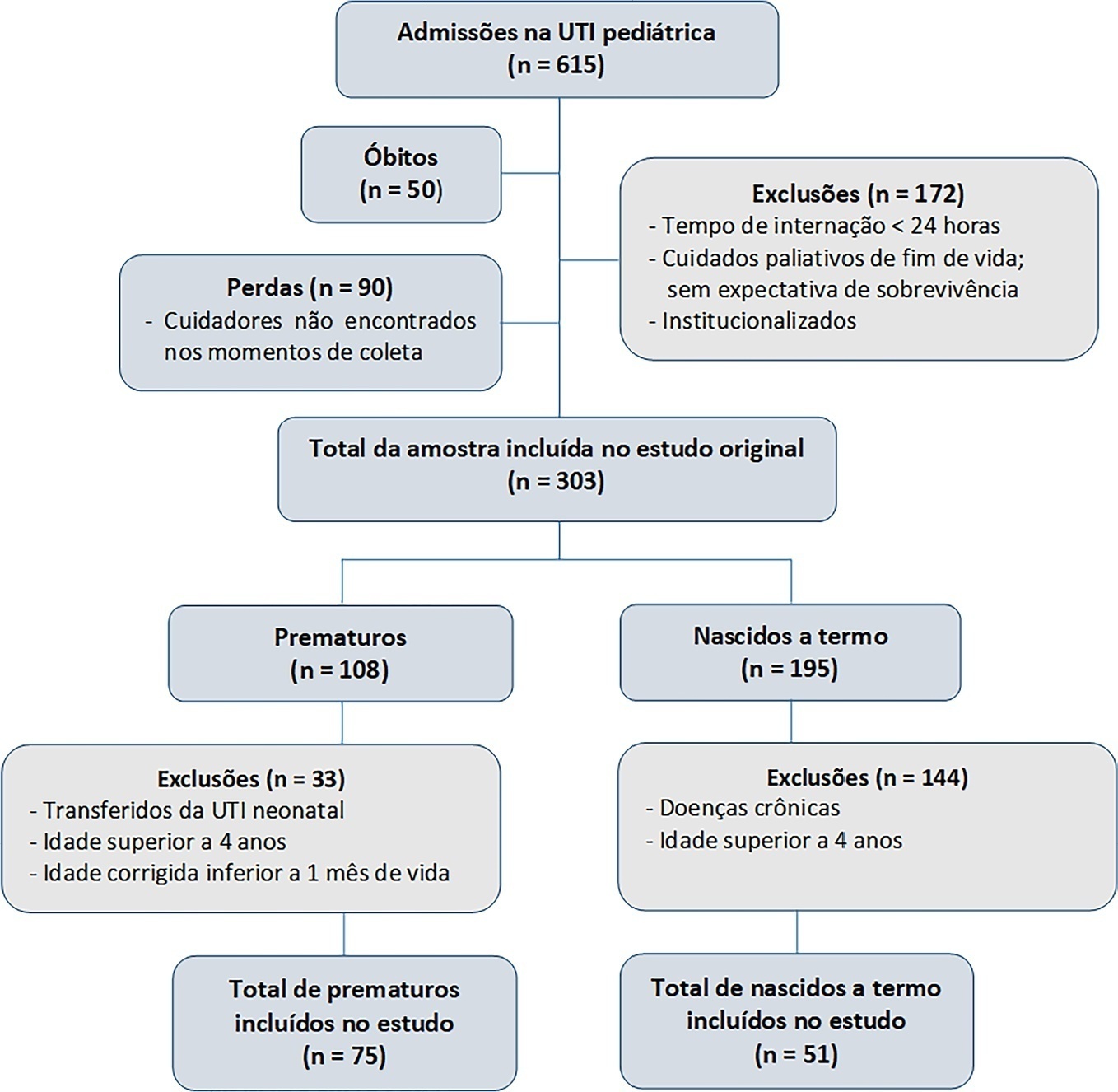
This was a secondary cross-sectional study nested in an observational cohort of survivors from a pediatric intensive care unit. Functional assessment was performed using the Functional Status Scale within 48 hours after discharge from the pediatric intensive care unit.
Results:
A total of 126 patients participated in the study, 75 of whom were premature, and 51 of whom were born at term. Comparing the baseline and functional status at pediatric intensive care unit discharge, both groups showed significant differences (p < 0.001). Preterm patients exhibited greater functional decline at discharge from the pediatric intensive care unit (61%). Among patients born at term, there was a significant correlation between the Pediatric Index of Mortality, duration of sedation, duration of mechanical ventilation and length of hospital stay with the functional outcomes (p = 0.05).
Conclusion:
Most patients showed a functional decline at discharge from the pediatric intensive care unit. Although preterm patients had a greater functional decline at discharge, sedation and mechanical ventilation duration influenced functional status among patients born at term.
-
Case Reports
Accidental strangulation in children by the automatic closing of a car window
Rev Bras Ter Intensiva. 2018;30(1):112-115
Abstract
Case ReportsAccidental strangulation in children by the automatic closing of a car window
Rev Bras Ter Intensiva. 2018;30(1):112-115
DOI 10.5935/0103-507X.20180017
Views1See moreABSTRACT
Among the main causes of death in our country are car accidents, drowning and accidental burns. Strangulation is a potentially fatal injury and an important cause of homicide and suicide among adults and adolescents. In children, its occurrence is usually accidental. However, in recent years, several cases of accidental strangulation in children around the world have been reported. A 2-year-old male patient was strangled in a car window. The patient was admitted to the pediatric intensive care unit with a Glasgow Coma Scale score of 8 and presented with progressive worsening of respiratory dysfunction and torpor. The patient also presented acute respiratory distress syndrome, acute pulmonary edema and shock. He was managed with protective mechanical ventilation, vasoactive drugs and antibiotic therapy. He was discharged from the intensive care unit without neurological or pulmonary sequelae. After 12 days of hospitalization, he was discharged from the hospital, and his state was very good. The incidence of automobile window strangulation is rare but of high morbidity and mortality due to the resulting choking mechanism. Fortunately, newer cars have devices that stop the automatic closing of the windows if resistance is encountered. However, considering the severity of complications strangulated patients experience, the intensive neuro-ventilatory and hemodynamic management of the pathologies involved is important to reduce morbidity and mortality, as is the need to implement new campaigns for the education of parents and caregivers of children, aiming to avoid easily preventable accidents and to optimize safety mechanisms in cars with electric windows.

-
Original Articles
Characteristics and progression of children with acute viral bronchiolitis subjected to mechanical ventilation
Rev Bras Ter Intensiva. 2016;28(1):55-61
Abstract
Original ArticlesCharacteristics and progression of children with acute viral bronchiolitis subjected to mechanical ventilation
Rev Bras Ter Intensiva. 2016;28(1):55-61
DOI 10.5935/0103-507X.20160003
Views0ABSTRACT
Objective:
To analyze the characteristics of children with acute viral bronchiolitis subjected to mechanical ventilation for three consecutive years and to correlate their progression with mechanical ventilation parameters and fluid balance.
Methods:
Longitudinal study of a series of infants (< one year old) subjected to mechanical ventilation for acute viral bronchitis from January 2012 to September 2014 in the pediatric intensive care unit. The children's clinical records were reviewed, and their anthropometric data, mechanical ventilation parameters, fluid balance, clinical progression, and major complications were recorded.
Results:
Sixty-six infants (3.0 ± 2.0 months old and with an average weight of 4.7 ± 1.4kg) were included, of whom 62% were boys; a virus was identified in 86%. The average duration of mechanical ventilation was 6.5 ± 2.9 days, and the average length of stay in the pediatric intensive care unit was 9.1 ± 3.5 days; the mortality rate was 1.5% (1/66). The peak inspiratory pressure remained at 30cmH2O during the first four days of mechanical ventilation and then decreased before extubation (25 cmH2O; p < 0.05). Pneumothorax occurred in 10% of the sample and extubation failure in 9%, which was due to upper airway obstruction in half of the cases. The cumulative fluid balance on mechanical ventilation day four was 402 ± 254mL, which corresponds to an increase of 9.0 ± 5.9% in body weight. Thirty-seven patients (56%) exhibited a weight gain of 10% or more, which was not significantly associated with the ventilation parameters on mechanical ventilation day four, extubation failure, duration of mechanical ventilation or length of stay in the pediatric intensive care unit.
Conclusion:
The rate of mechanical ventilation for acute viral bronchiolitis remains constant, being associated with low mortality, few adverse effects, and positive cumulative fluid balance during the first days. Better fluid control might reduce the duration of mechanical ventilation.
Keywords:BronchiolitisChildEdemaIntensive care unitsRespiration, artificialRespiratory syncytial virusesSee more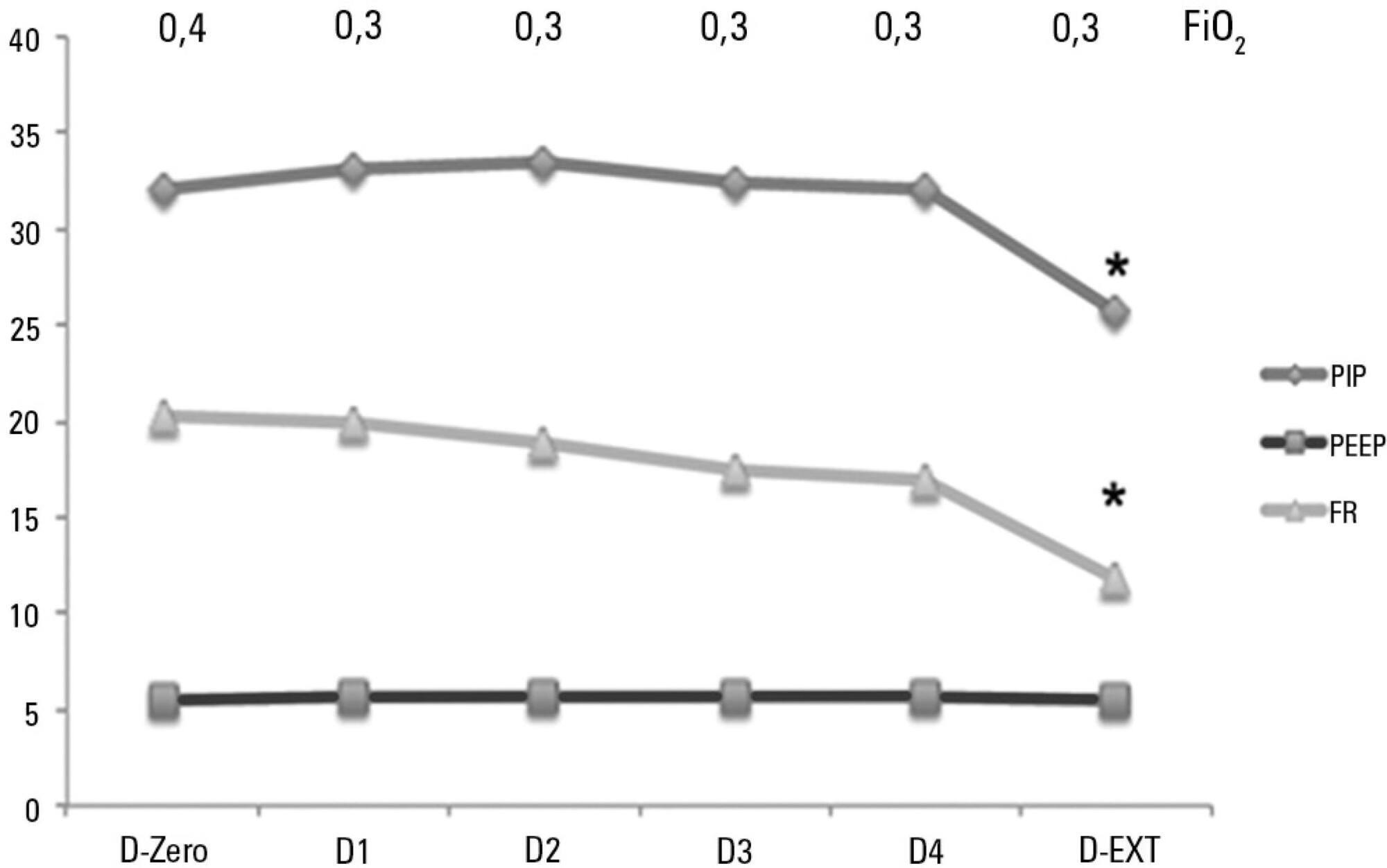
-
Original Articles
Health professionals’ perceptions about the decision-making process in the care of pediatric patients
Rev Bras Ter Intensiva. 2016;28(3):335-340
Abstract
Original ArticlesHealth professionals’ perceptions about the decision-making process in the care of pediatric patients
Rev Bras Ter Intensiva. 2016;28(3):335-340
DOI 10.5935/0103-507X.20160057
Views0ABSTRACT
Objective:
To evaluate the perceptions of physicians, nurses and nursing technicians of their participation in the decision-making process surrounding life support limitation in terminally ill pediatric patients, with comparisons by professional category.
Methods:
A cross-sectional study was conducted in the pediatric intensive care unit of a tertiary public university hospital with the participation of physicians, nurses and nursing technicians. The MacArthur Admission Experience Survey Voice Scale was used to assess and quantify the perceptions of professionals who assisted 17 pediatric patients with life support limitation within 24 hours after the outcome of each patient was determined. All professionals working in the unit (n = 117) who were potentially eligible for the study received a free and informed consent form prior to the occurrence of the cases studied.
Results:
Study participants included 25/40 (62.5%) physicians, 10/17 (58.8%) nurses and 41/60 (68.3%) nursing technicians, representing 65% of the eligible professionals identified. The questionnaire return rate was higher for physicians than technicians (p = 0.0258). A perceived lack of voice was reported in all three professional categories at varying rates that were lower for physicians than for nurses and nursing technicians (p < 0.00001); there was no difference between the latter (p = 0.7016). In the three professional categories studied, three subscale items were reported. For two of the three statements, there were significant differences between physicians and nurses (p = 0.004) and between physicians and nursing technicians (p = 0.001). For one of the statements, there was no difference among the three professional categories.
Conclusion:
Respondents perceived a lack of voice in the decision-making process at varying rates across the three categories of studied professionals who assisted terminally ill pediatric patients with life support limitation, with physicians expressing lowered rates of perceived coercion.
Keywords:CoercionDecision MakingEthics, professionalIntensive care units, pediatricPatient careResuscitation orders/psychologySurveys and questionnairesSee more -
Original Articles
A comparison of gradual sedation levels using the Comfort-B scale and bispectral index in children on mechanical ventilation in the pediatric intensive care unit
Rev Bras Ter Intensiva. 2013;25(4):306-311
Abstract
Original ArticlesA comparison of gradual sedation levels using the Comfort-B scale and bispectral index in children on mechanical ventilation in the pediatric intensive care unit
Rev Bras Ter Intensiva. 2013;25(4):306-311
DOI 10.5935/0103-507X.20130052
Views0Objective:
Compare the scores resulting from the Comfort-B scale with the bispectral index in children in an intensive care unit.
Methods:
Eleven children between the ages of 1 month and 16 years requiring mechanical ventilation and sedation were simultaneously classified based on the bispectral index and the Comfort-B scale. Their behavior was recorded using digital photography, and the record was later evaluated by three independent evaluators. Agreement tests (Bland-Altman and Kappa) were then performed. The correlation between the two methods (Pearson correlation) was tested.
Results:
In total, 35 observations were performed on 11 patients. Based on the Kappa coefficient, the agreement among evaluators ranged from 0.56 to 0.75 (p<0.001). There was a positive and consistent association between the bispectral index and the Comfort-B scale [r=0.424 (p=0.011) to r=0.498 (p=0.002)].
Conclusion:
Due to the strong correlation between the independent evaluators and the consistent correlation between the two methods, the results suggest that the Comfort-B scale is reproducible and useful in classifying the level of sedation in children requiring mechanical ventilation.
Keywords:ChildConscious sedationElectroencephalography/instrumentationIntensive care units, pediatricMonitoring, physiologic/instrumentationRespiration, artificial/methodsSee more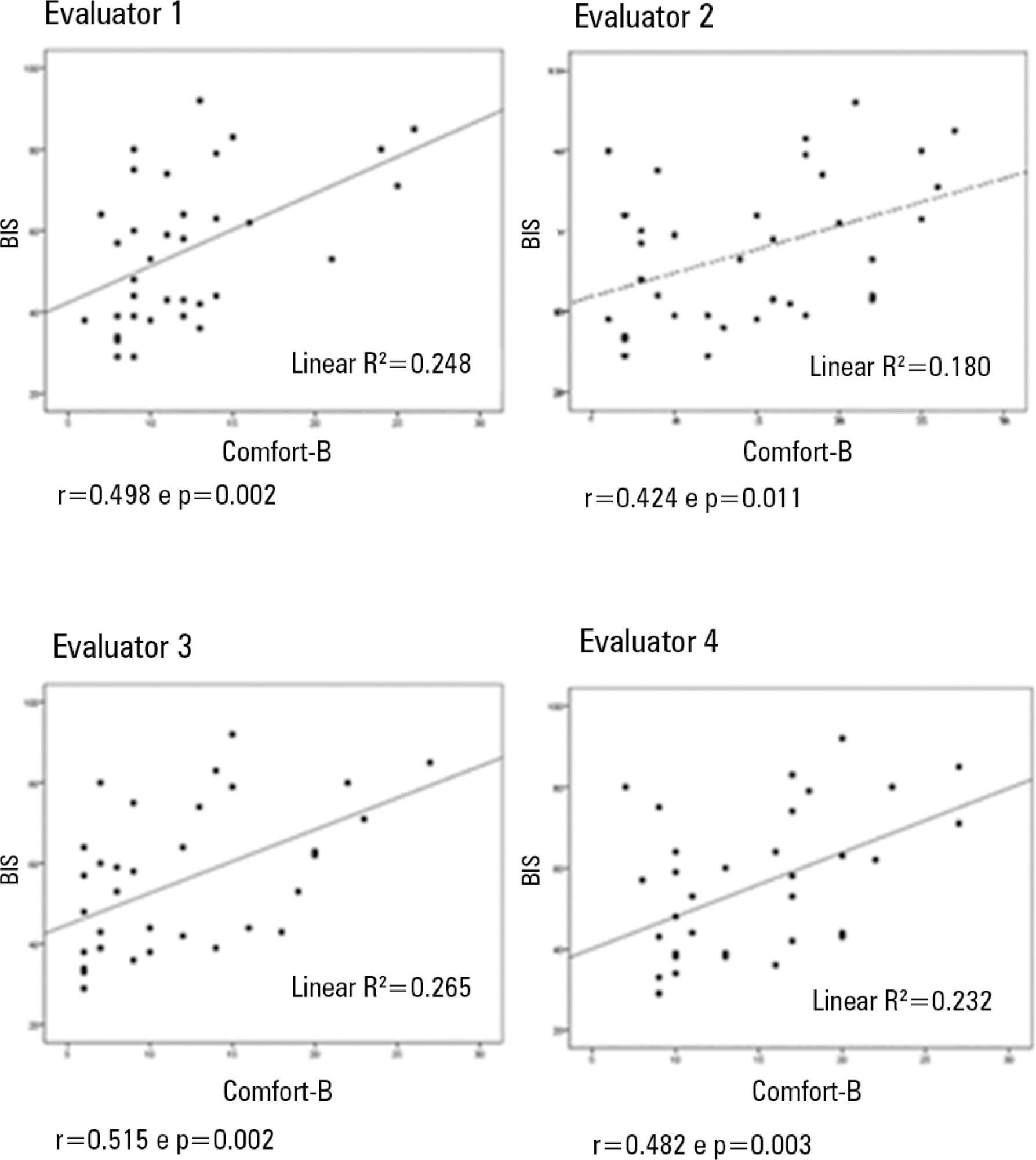
-
Original Articles
Validation of sedation scores in mechanically ventilated children admitted to a tertiary pediatric intensive care unit
Rev Bras Ter Intensiva. 2008;20(4):325-330
Abstract
Original ArticlesValidation of sedation scores in mechanically ventilated children admitted to a tertiary pediatric intensive care unit
Rev Bras Ter Intensiva. 2008;20(4):325-330
DOI 10.1590/S0103-507X2008000400002
Views0OBJECTIVES: Sedation scores are important tools for use in pediatric intensive care units. The Comfort-Behavior scale is a valid method for the assessment of children although it is considered an extensive scale. The motor activity assessment scale is validated for an adult population. We considered it simpler then the one above and suitable for application in children. None of these scores had been translated into Portuguese. Our objective was to apply both scales in Portuguese to a pediatric population under mechanical ventilation. Secondary objectives were to evaluate the sedation level of children on mechanical ventilation in tertiary pediatric intensive care units and to compare the Comfort- Behavior and motor activity assessment scales in this population. METHODS: After translating the scales into Portuguese, both were simultaneously applied to 26 patients by 2 pediatricians. Each scale was applied 116 times in total. RESULTS: The intraclass correlation coefficient was 0.90 (0.85 – 0.93 CI 95%) for the Comfort-Behavior and 0.94 (0.92 – 0.96 CI 95%) for the motor activity assessment scale. When applying the Comfort-Behavior scale, the Crombach’s alpha was 0.81 for observer A and 0.92 for observer B. The Spearman coefficient was 0.86 for observer A and 0.91 for observer B. These patients were found to be deeply sedated, showing low values in both scales. CONCLUSIONS: The scales were successfully translated into Portuguese and both were adequate to assess pain and sedation in the pediatric population under mechanical ventilation. Sedation level was high in this sample of applications.
Keywords:AnalgesicsChildChild behaviorIntensive care units, pediatricMonitoring, physiologicPain measurementRespiration, artificialSee more -
Original Articles
Evaluation of intensivists’ knowledge on brain death
Rev Bras Ter Intensiva. 2008;20(2):144-148
Abstract
Original ArticlesEvaluation of intensivists’ knowledge on brain death
Rev Bras Ter Intensiva. 2008;20(2):144-148
DOI 10.1590/S0103-507X2008000200005
Views0See moreBACKGROUND AND OBJECTIVES: Failure or delay to diagnose brain death leads to needless occupation of a hospital bed, emotional and financial losses, and unavailability of organs for transplants. The intensive care physician plays an essential role in this diagnosis. This study intended to evaluate intensivists’ knowledge concerning brain death. METHODS: Cross-sectional study in 15 intensive care units (ICU) in eight hospitals in the city of Porto Alegre, Brazil. RESULTS: Two hundred forty-six intensivists were interviewed in a consecutive sample between April and December 2005. The prevalence of lack of knowledge regarding the concept was of 17%. Twenty per cent of the interviewees ignored the legal need for complementary confirmatory tests for their diagnosis. Forty-seven per cent considered themselves as having the highest level of assurance to explain the concept to a patient’s family members. Twenty-nine per cent erroneously determined the legal time of death for brain dead patients. Pediatric intensivists had less knowledge about the concept, when compared to intensivists for adults (p < 0.001). CONCLUSIONS: Current knowledge of brain death is insufficient in Brazil, among the health care professionals who most often find patients in this situation. Education on the subject is needed to avoid unnecessary expenses, reduce family suffering and increase the offer of organs for transplant.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




