Abstract
Rev Bras Ter Intensiva. 2020;32(2):284-294
DOI 10.5935/0103-507X.20200045
To identify the relationship of patient-ventilator asynchrony with the level of sedation and hemogasometric and clinical results.
This was a prospective study of 122 patients admitted to the intensive care unit who underwent > 24 hours of invasive mechanical ventilation with inspiratory effort. In the first 7 days of ventilation, patient-ventilator asynchrony was evaluated daily for 30 minutes. Severe patient-ventilator asynchrony was defined as an asynchrony index > 10%.
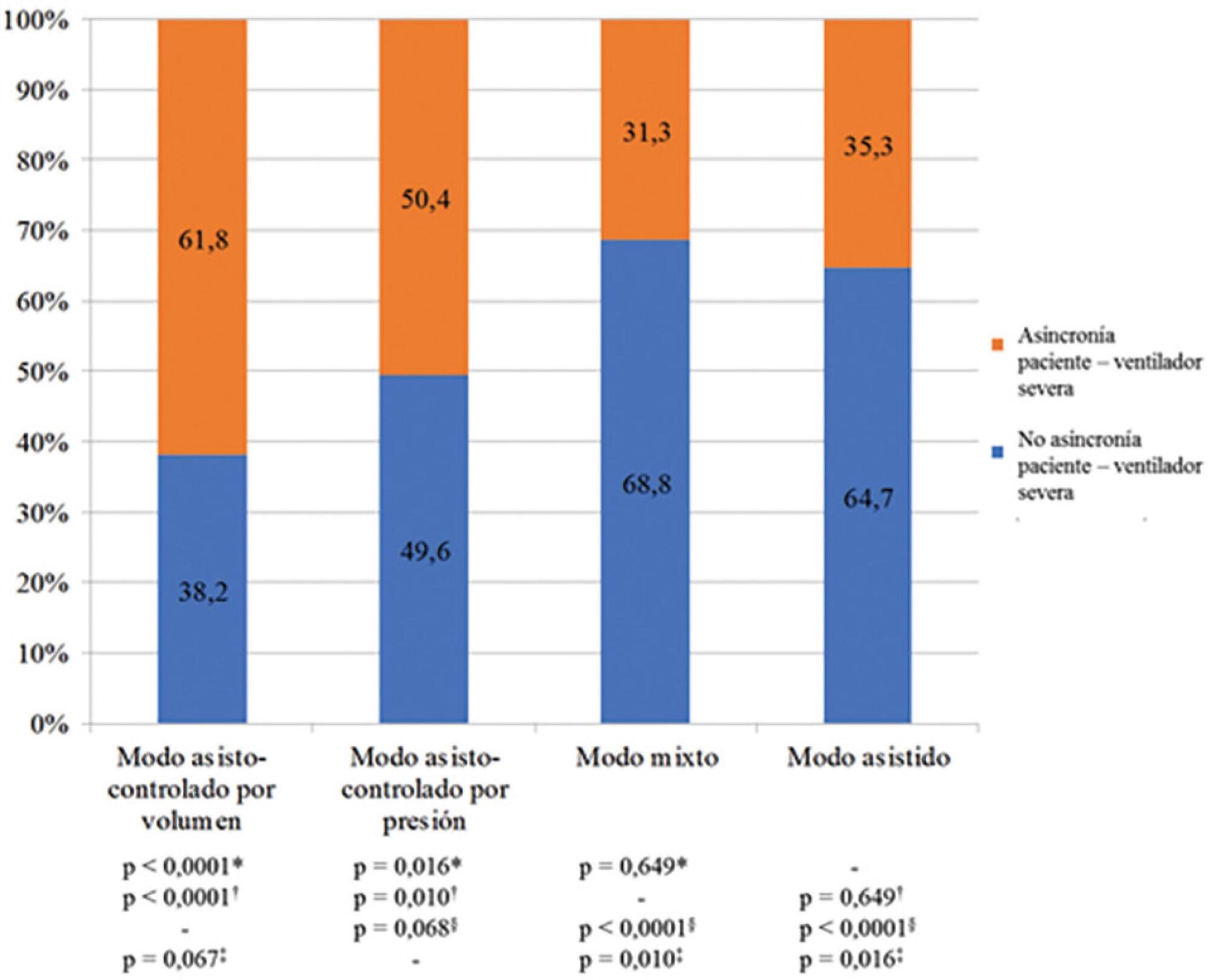
A total of 339,652 respiratory cycles were evaluated in 504 observations. The mean asynchrony index was 37.8% (standard deviation 14.1 - 61.5%). The prevalence of severe patient-ventilator asynchrony was 46.6%. The most frequent patient-ventilator asynchronies were ineffective trigger (13.3%), autotrigger (15.3%), insufficient flow (13.5%), and delayed cycling (13.7%). Severe patient-ventilator asynchrony was related to the level of sedation (ineffective trigger: p = 0.020; insufficient flow: p = 0.016; premature cycling: p = 0.023) and the use of midazolam (p = 0.020). Severe patient-ventilator asynchrony was also associated with hemogasometric changes. The persistence of severe patient-ventilator asynchrony was an independent risk factor for failure of the spontaneous breathing test, ventilation time, ventilator-associated pneumonia, organ dysfunction, mortality in the intensive care unit, and length of stay in the intensive care unit.
Patient-ventilator asynchrony is a frequent disorder in critically ill patients with inspiratory effort. The patient’s interaction with the ventilator should be optimized to improve hemogasometric parameters and clinical results. Further studies are required to confirm these results.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):26-35
DOI 10.5935/0103-507X.20150006
The number of patients who require prolonged mechanical ventilation increased during the last decade, which generated a large population of chronically ill patients. This study established the incidence of prolonged mechanical ventilation in four intensive care units and reported different characteristics, hospital outcomes, and the impact of costs and services of prolonged mechanical ventilation patients (mechanical ventilation dependency ≥ 21 days) compared with non-prolonged mechanical ventilation patients (mechanical ventilation dependency < 21 days).
This study was a multicenter cohort study of all patients who were admitted to four intensive care units. The main outcome measures were length of stay in the intensive care unit, hospital, complications during intensive care unit stay, and intensive care unit and hospital mortality.
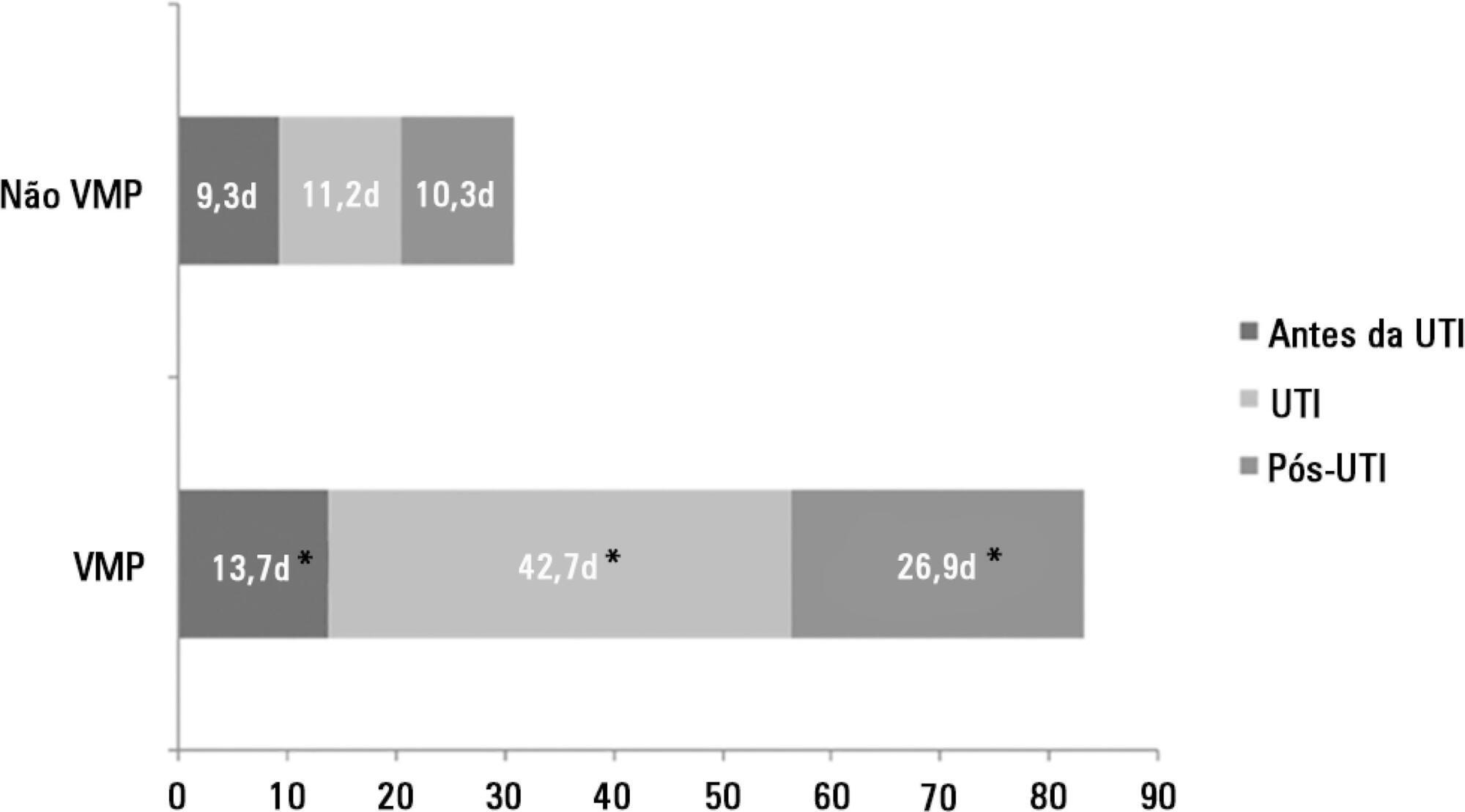
There were 5,287 admissions to the intensive care units during study period. Some of these patients (41.5%) needed ventilatory support (n = 2,197), and 218 of the patients met criteria for prolonged mechanical ventilation (9.9%). Some complications developed during intensive care unit stay, such as muscle weakness, pressure ulcers, bacterial nosocomial sepsis, candidemia, pulmonary embolism, and hyperactive delirium, were associated with a significantly higher risk of prolonged mechanical ventilation. Prolonged mechanical ventilation patients had a significant increase in intensive care unit mortality (absolute difference = 14.2%, p < 0.001) and hospital mortality (absolute difference = 19.1%, p < 0.001). The prolonged mechanical ventilation group spent more days in the hospital after intensive care unit discharge (26.9 ± 29.3 versus 10.3 ± 20.4 days, p < 0.001) with higher costs.
The classification of chronically critically ill patients according to the definition of prolonged mechanical ventilation adopted by our study (mechanical ventilation dependency ≥ 21 days) identified patients with a high risk for complications during intensive care unit stay, longer intensive care unit and hospital stays, high death rates, and higher costs.
Abstract
Rev Bras Ter Intensiva. 2013;25(4):306-311
DOI 10.5935/0103-507X.20130052
Compare the scores resulting from the Comfort-B scale with the bispectral index in children in an intensive care unit.
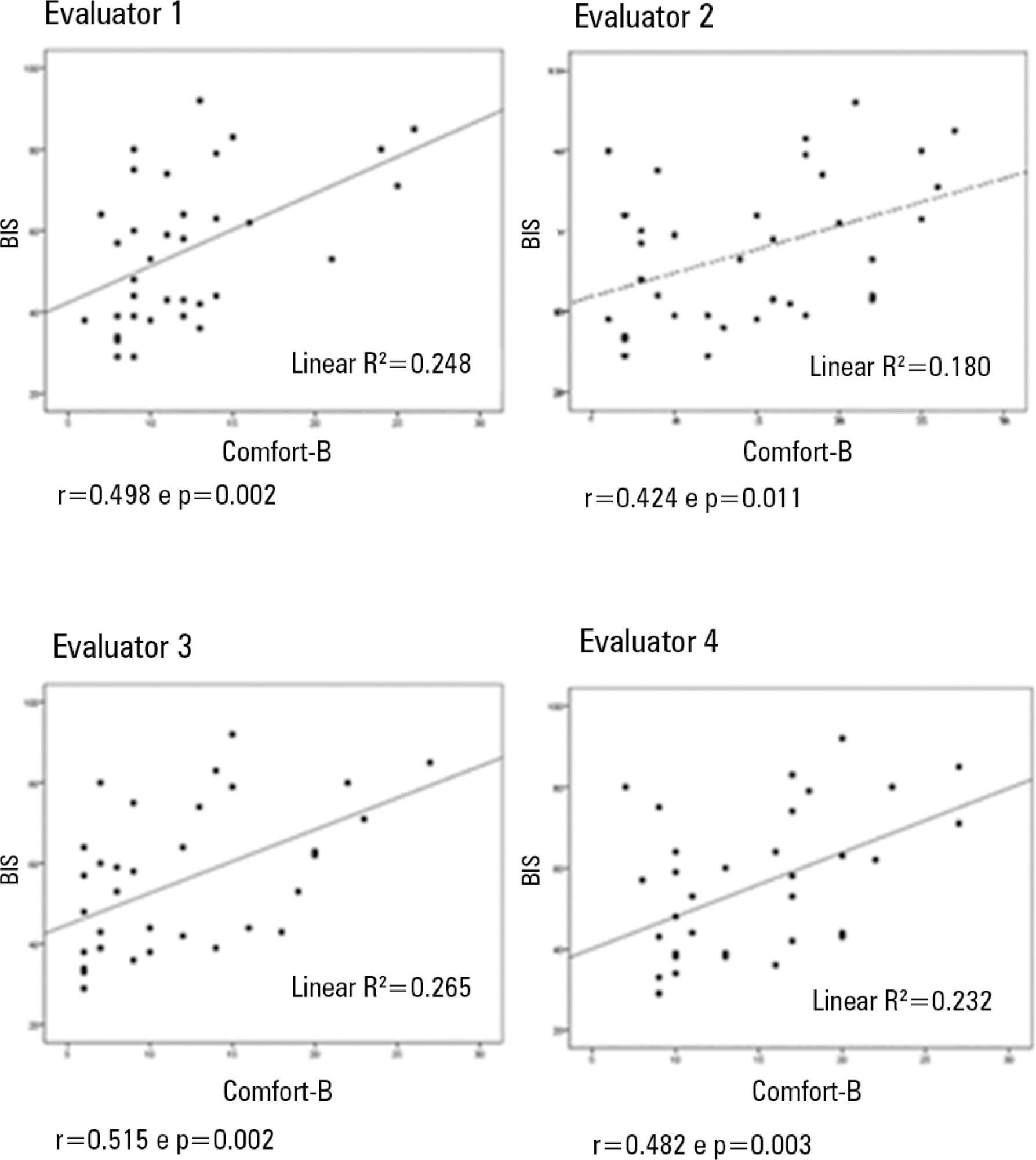
Eleven children between the ages of 1 month and 16 years requiring mechanical ventilation and sedation were simultaneously classified based on the bispectral index and the Comfort-B scale. Their behavior was recorded using digital photography, and the record was later evaluated by three independent evaluators. Agreement tests (Bland-Altman and Kappa) were then performed. The correlation between the two methods (Pearson correlation) was tested.
In total, 35 observations were performed on 11 patients. Based on the Kappa coefficient, the agreement among evaluators ranged from 0.56 to 0.75 (p<0.001). There was a positive and consistent association between the bispectral index and the Comfort-B scale [r=0.424 (p=0.011) to r=0.498 (p=0.002)].
Due to the strong correlation between the independent evaluators and the consistent correlation between the two methods, the results suggest that the Comfort-B scale is reproducible and useful in classifying the level of sedation in children requiring mechanical ventilation.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (33) COVID-19 (45) Critical care (115) Critical illness (54) ICU (25) Infant, newborn (27) Intensive care (72) Intensive care units (254) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (75) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (117) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)