Abstract
Rev Bras Ter Intensiva. 2021;33(3):461-468
DOI 10.5935/0103-507X.20210061
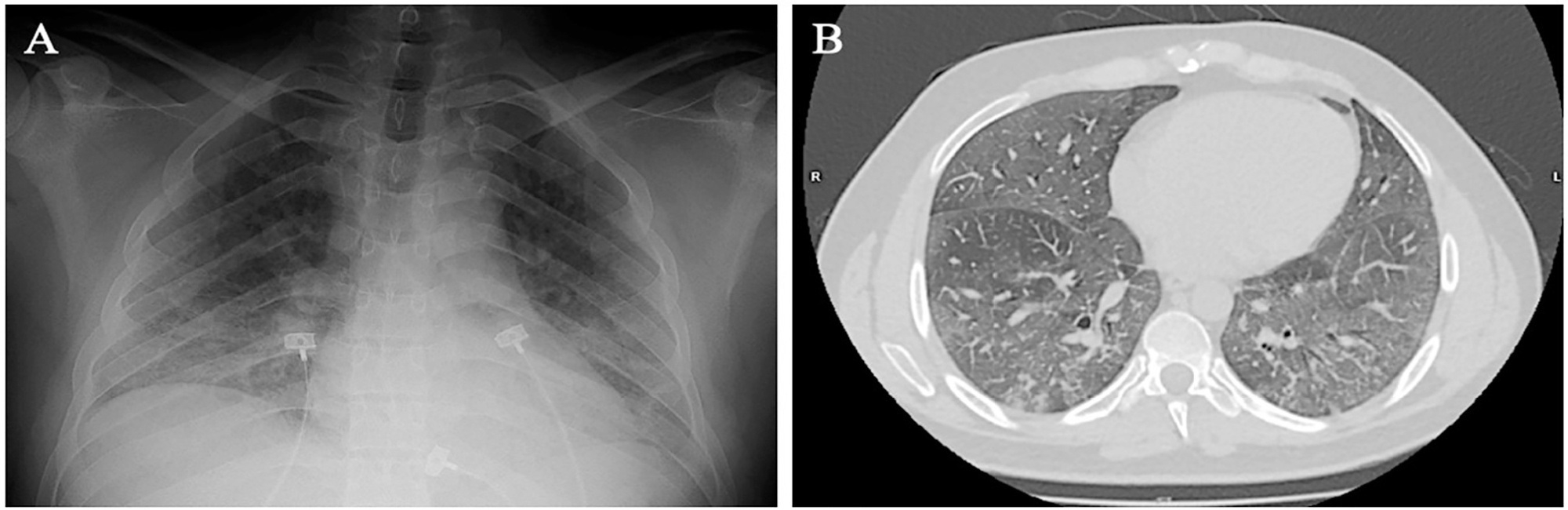
Spontaneous breathing can be deleterious in patients with previously injured lungs, especially in acute respiratory distress syndrome. Moreover, the failure to assume spontaneous breathing during mechanical ventilation and the need to switch back to controlled mechanical ventilation are associated with higher mortality. There is a gap of knowledge regarding which parameters might be useful to predict the risk of patient self-inflicted lung injury and to detect the inability to assume spontaneous breathing. We report a case of patient self-inflicted lung injury, the corresponding basic and advanced monitoring of the respiratory system mechanics and physiological and clinical results related to spontaneous breathing. The patient was a 33-year-old Caucasian man with a medical history of AIDS who developed acute respiratory distress syndrome and needed invasive mechanical ventilation after noninvasive ventilatory support failure. During the controlled ventilation periods, a protective ventilation strategy was adopted, and the patient showed clear clinical and radiographic improvement. However, during each spontaneous breathing period under pressure support ventilation, despite adequate initial parameters and a strictly adjusted ventilatory setting and monitoring, the patient developed progressive hypoxemia and worsening of respiratory system mechanics with a clearly correlated radiographic deterioration (patient self-inflicted lung injury). After failing three spontaneous breathing assumption trials, he died on day 29 due to refractory hypoxemia. Conventional basic and advanced monitoring variables in this case were not sufficient to identify the aptitude to breathe spontaneously or to predict the risk and development of patient self-inflicted lung injury during partial support ventilation.
Abstract
Rev Bras Ter Intensiva. 2020;32(2):284-294
DOI 10.5935/0103-507X.20200045
To identify the relationship of patient-ventilator asynchrony with the level of sedation and hemogasometric and clinical results.
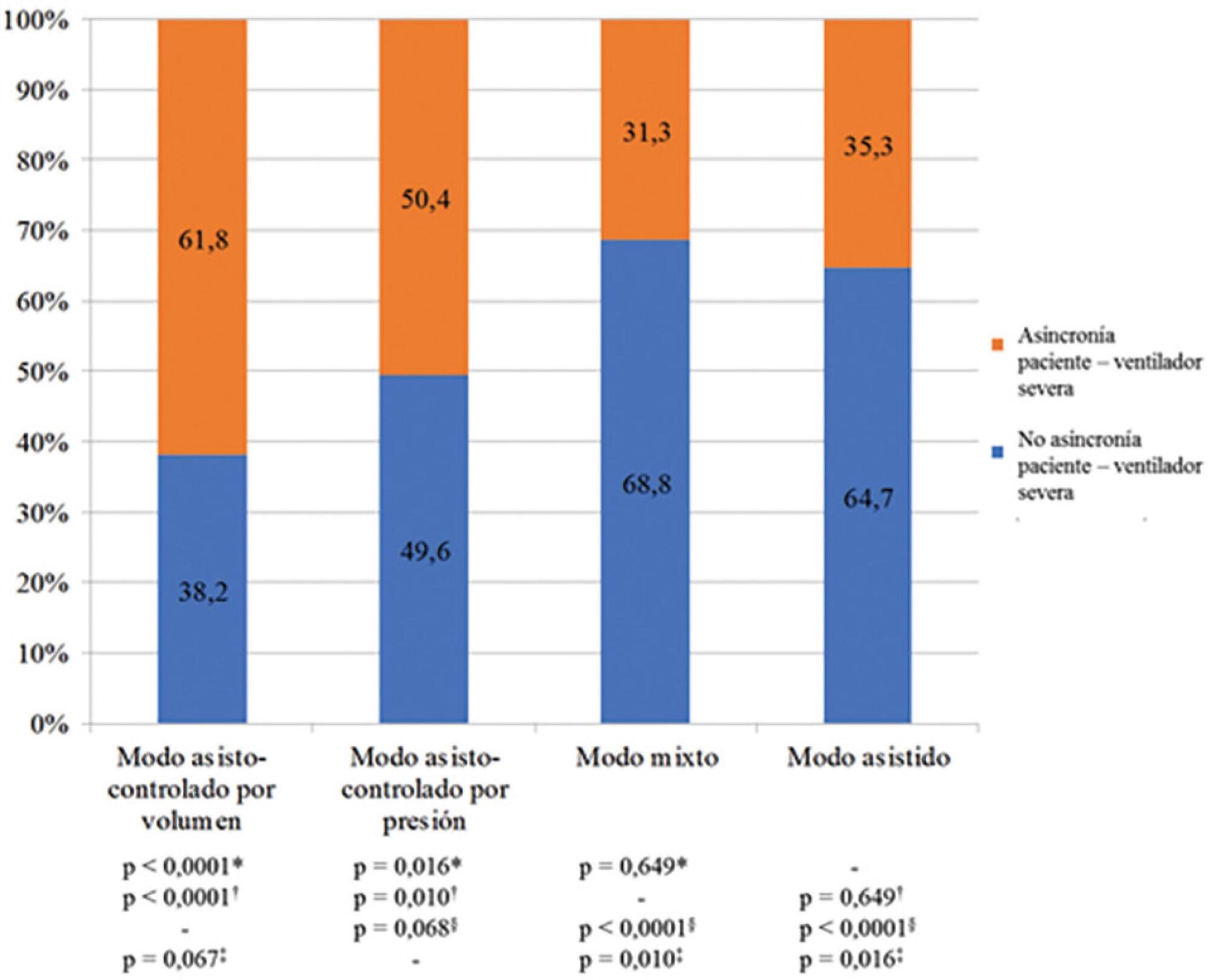
This was a prospective study of 122 patients admitted to the intensive care unit who underwent > 24 hours of invasive mechanical ventilation with inspiratory effort. In the first 7 days of ventilation, patient-ventilator asynchrony was evaluated daily for 30 minutes. Severe patient-ventilator asynchrony was defined as an asynchrony index > 10%.
A total of 339,652 respiratory cycles were evaluated in 504 observations. The mean asynchrony index was 37.8% (standard deviation 14.1 - 61.5%). The prevalence of severe patient-ventilator asynchrony was 46.6%. The most frequent patient-ventilator asynchronies were ineffective trigger (13.3%), autotrigger (15.3%), insufficient flow (13.5%), and delayed cycling (13.7%). Severe patient-ventilator asynchrony was related to the level of sedation (ineffective trigger: p = 0.020; insufficient flow: p = 0.016; premature cycling: p = 0.023) and the use of midazolam (p = 0.020). Severe patient-ventilator asynchrony was also associated with hemogasometric changes. The persistence of severe patient-ventilator asynchrony was an independent risk factor for failure of the spontaneous breathing test, ventilation time, ventilator-associated pneumonia, organ dysfunction, mortality in the intensive care unit, and length of stay in the intensive care unit.
Patient-ventilator asynchrony is a frequent disorder in critically ill patients with inspiratory effort. The patient’s interaction with the ventilator should be optimized to improve hemogasometric parameters and clinical results. Further studies are required to confirm these results.
Abstract
Rev Bras Ter Intensiva. 2020;32(1):81-91
DOI 10.5935/0103-507X.20200013
To identify common practices related to the use and titration of pressure-support ventilation (PC-CSV - pressure control-continuous spontaneous ventilation) in patients under mechanical ventilation and to analyze diagnostic criteria for over-assistance and under-assistance. The secondary objective was to compare the responses provided by physician, physiotherapists and nurses related to diagnostic criteria for over-assistance and under-assistance.
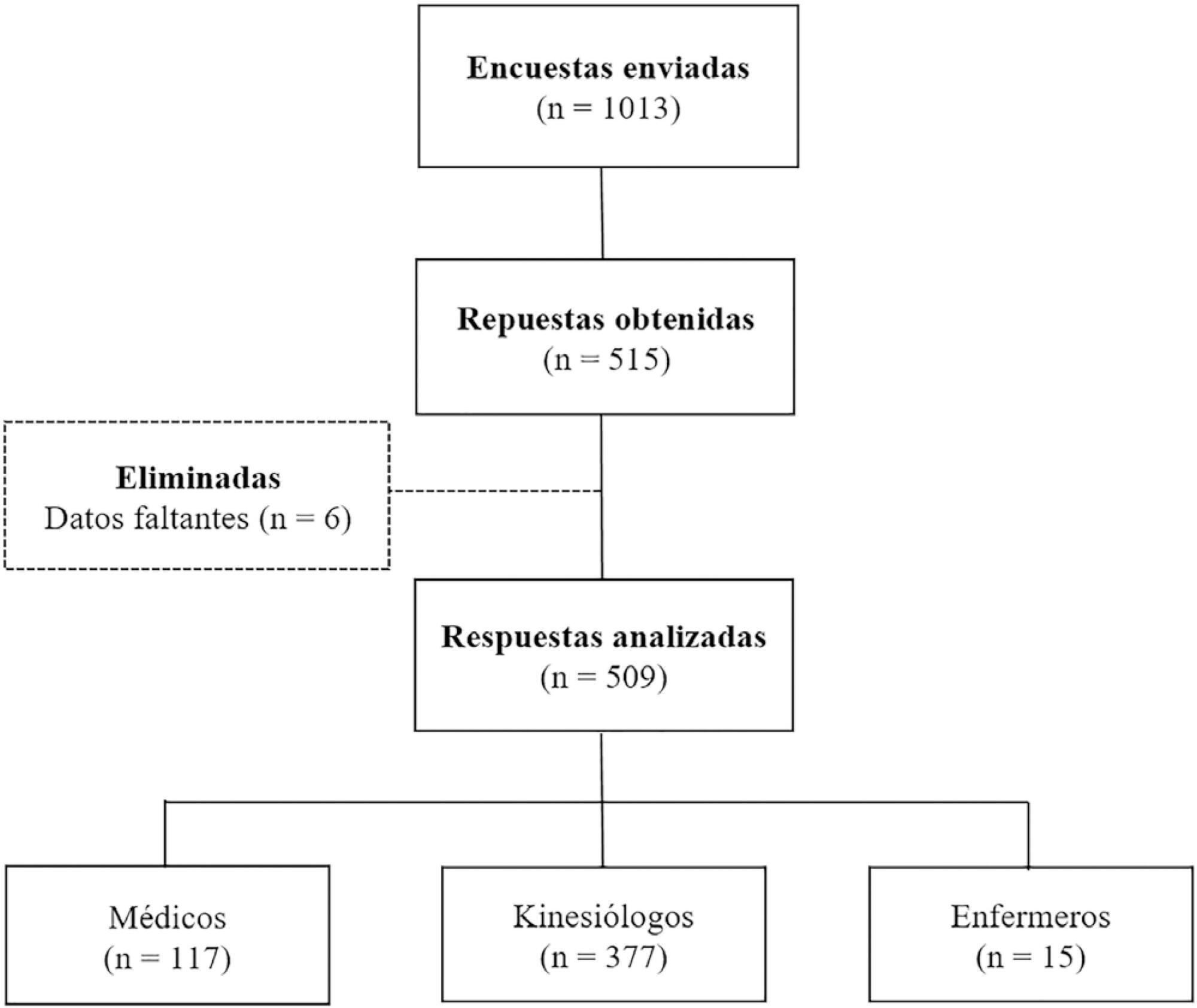
An online survey was conducted using the Survey Monkey tool. Physicians, nurses and physiotherapists from Argentina with access to PC-CSV in their usual clinical practice were included.
A total of 509 surveys were collected from October to December 2018. Of these, 74.1% were completed by physiotherapists. A total of 77.6% reported using PC-CSV to initiate the partial ventilatory support phase, and 43.8% of respondents select inspiratory pressure support level based on tidal volume. The main objective for selecting positive end-expiratory pressure (PEEP) level was to decrease the work of breathing. High tidal volume was the primary variable for detecting over-assistance, while the use of accessory respiratory muscles was the most commonly chosen for under-assistance. Discrepancies were observed between physicians and physiotherapists in relation to the diagnostic criteria for over-assistance.
The most commonly used mode to initiate the partial ventilatory support phase was PC-CSV. The most frequently selected variable to guide the titration of inspiratory pressure support level was tidal volume, and the main objective of PEEP was to decrease the work of breathing. Over-assistance was detected primarily by high tidal volume, while under-assistance by accessory respiratory muscles activation. Discrepancies were observed among professions in relation to the diagnostic criteria for over-assistance, but not for under-assistance.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):245-250
DOI 10.5935/0103-507X.20130042
To analyze the incidence of early-onset nasal injury in infants with very low birth weight and indication for noninvasive ventilation via nasal prongs.
A prospective case series of infants with gestational age <37 weeks, weight <1.500 g and postnatal age <29 days. The patients were evaluated three times daily from the installation of nasal prongs to the 3rd day of use. The patients' clinical conditions and the device's characteristics and its application were analyzed. The initial analysis was descriptive, indicating the prevalence of nasal injury and factors associated with it. Categorical data were analyzed using the chi-squared test or Fisher's exact test, and numerical data were analyzed using the t-test or the Mann-Whitney test.
Eighteen infants were included; 12 (with a gestational age of 29.8±3.1 weeks, birth weight of 1.070±194 g and a Score for Neonatal Acute Physiology - Perinatal Extension (SNAPPE) of 15.4±17.5) developed nasal injuries (injury group), and 6 (with a gestational age of 28.0±1.9 weeks, weight of 1.003±317 g and SNAPPE of 26.2±7.5) showed no nasal injury (uninjured group). The injury group subjects were more often male (75% versus 17%), and their injuries appeared after an average of 18 hours, predominantly during the night (75%).
The incidence of nasal injury in preterm infants who experienced noninvasive ventilation via nasal prongs was high, and a study of associated factors may be planned based on this pilot.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)