You searched for:"Frank Daniel Martos-Benítez"
We found (2) results for your search.-
Original Article
Outcomes of ventilatory asynchrony in patients with inspiratory effort
Rev Bras Ter Intensiva. 2020;32(2):284-294
Abstract
Original ArticleOutcomes of ventilatory asynchrony in patients with inspiratory effort
Rev Bras Ter Intensiva. 2020;32(2):284-294
DOI 10.5935/0103-507X.20200045
Views0Abstract
Objective:
To identify the relationship of patient-ventilator asynchrony with the level of sedation and hemogasometric and clinical results.
Methods:
This was a prospective study of 122 patients admitted to the intensive care unit who underwent > 24 hours of invasive mechanical ventilation with inspiratory effort. In the first 7 days of ventilation, patient-ventilator asynchrony was evaluated daily for 30 minutes. Severe patient-ventilator asynchrony was defined as an asynchrony index > 10%.
Results:
A total of 339,652 respiratory cycles were evaluated in 504 observations. The mean asynchrony index was 37.8% (standard deviation 14.1 – 61.5%). The prevalence of severe patient-ventilator asynchrony was 46.6%. The most frequent patient-ventilator asynchronies were ineffective trigger (13.3%), autotrigger (15.3%), insufficient flow (13.5%), and delayed cycling (13.7%). Severe patient-ventilator asynchrony was related to the level of sedation (ineffective trigger: p = 0.020; insufficient flow: p = 0.016; premature cycling: p = 0.023) and the use of midazolam (p = 0.020). Severe patient-ventilator asynchrony was also associated with hemogasometric changes. The persistence of severe patient-ventilator asynchrony was an independent risk factor for failure of the spontaneous breathing test, ventilation time, ventilator-associated pneumonia, organ dysfunction, mortality in the intensive care unit, and length of stay in the intensive care unit.
Conclusion:
Patient-ventilator asynchrony is a frequent disorder in critically ill patients with inspiratory effort. The patient’s interaction with the ventilator should be optimized to improve hemogasometric parameters and clinical results. Further studies are required to confirm these results.
Keywords:Intensive care unitsInteractive ventilatory supportMortalityPhysiological monitoringRespiration, artificial/methodsSee more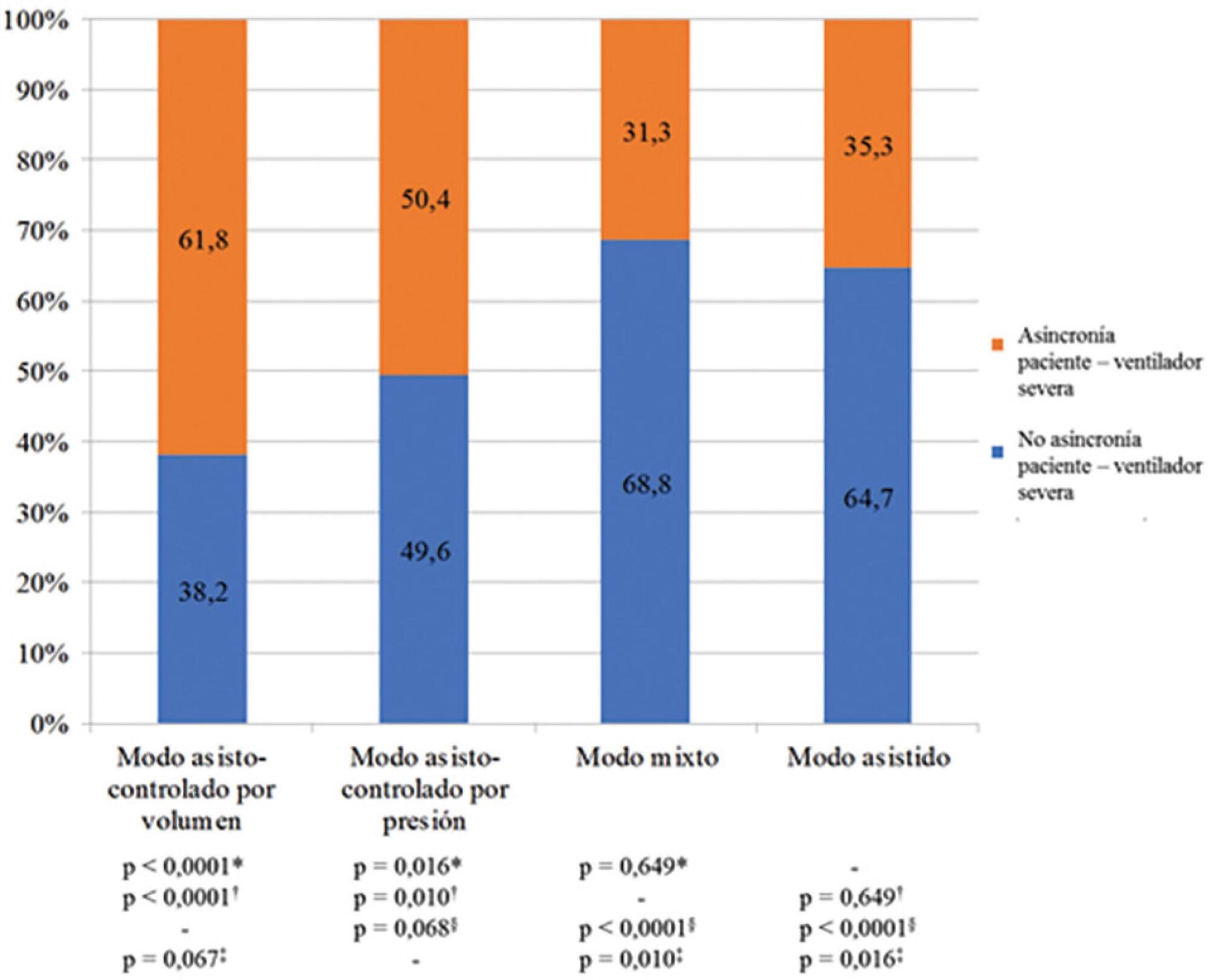
-
Original Article
Postoperative complications and clinical outcomes among patients undergoing thoracic and gastrointestinal cancer surgery: A prospective cohort study
Rev Bras Ter Intensiva. 2016;28(1):40-48
Abstract
Original ArticlePostoperative complications and clinical outcomes among patients undergoing thoracic and gastrointestinal cancer surgery: A prospective cohort study
Rev Bras Ter Intensiva. 2016;28(1):40-48
DOI 10.5935/0103-507X.20160012
Views0ABSTRACT
Objective:
This study sought to determine the influence of postoperative complications on the clinical outcomes of patients who underwent thoracic and gastrointestinal cancer surgery.
Methods:
A prospective cohort study was conducted regarding 179 consecutive patients who received thorax or digestive tract surgery due to cancer and were admitted to an oncological intensive care unit. The Postoperative Morbidity Survey was used to evaluate the incidence of postoperative complications. The influence of postoperative complications on both mortality and length of hospital stay were also assessed.
Results:
Postoperative complications were found for 54 patients (30.2%); the most common complications were respiratory problems (14.5%), pain (12.9%), cardiovascular problems (11.7%), infectious disease (11.2%), and surgical wounds (10.1%). A multivariate logistic regression found that respiratory complications (OR = 18.68; 95%CI = 5.59 – 62.39; p < 0.0001), cardiovascular problems (OR = 5.06, 95%CI = 1.49 - 17.13; p = 0.009), gastrointestinal problems (OR = 26.09; 95%CI = 6.80 - 100.16; p < 0.0001), infectious diseases (OR = 20.55; 95%CI = 5.99 - 70.56; p < 0.0001) and renal complications (OR = 18.27; 95%CI = 3.88 - 83.35; p < 0.0001) were independently associated with hospital mortality. The occurrence of at least one complication increased the likelihood of remaining hospitalized (log-rank test, p = 0.002).
Conclusions:
Postoperative complications are frequent disorders that are associated with poor clinical outcomes; thus, structural and procedural changes should be implemented to reduce postoperative morbidity and mortality.
Keywords:Gastrointestinal neoplasms/complicationsGastrointestinal neoplasms/surgeryHospital mortalityLength of hospital stayPostoperative complicationThoracic neoplasms/complicationsThoracic neoplasms/surgeryTreatment outcomeSee more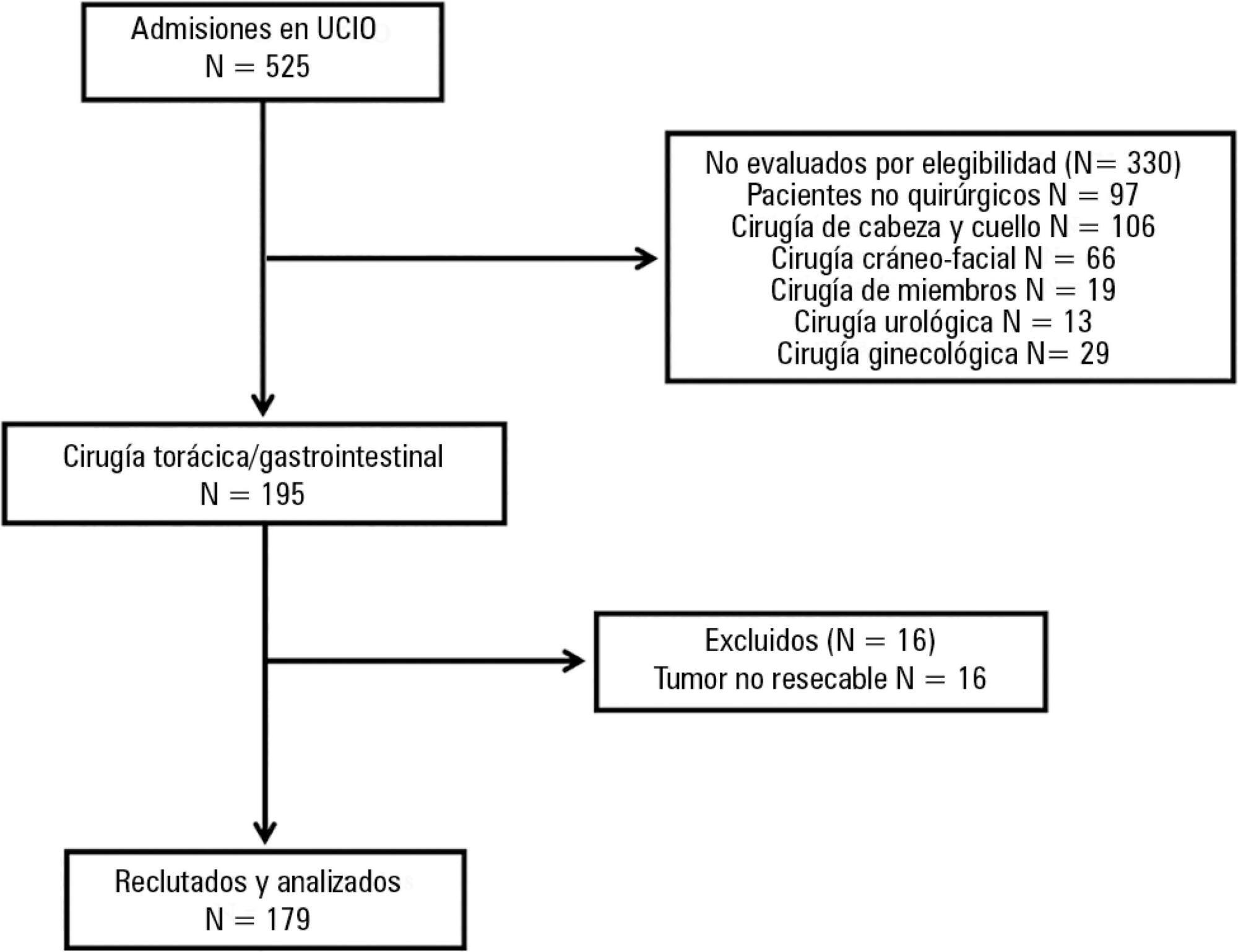
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




