Abstract
Crit Care Sci. 2024;36:e20240196en
DOI 10.62675/2965-2774.20240196-en
To provide insights into the potential benefits of goal-directed therapy guided by FloTrac in reducing postoperative complications and improving outcomes.
We performed a systematic review and meta-analysis of randomized controlled trials to evaluate goal-directed therapy guided by FloTrac in major surgery, comparing goal-directed therapy with usual care or invasive monitoring in cardiac and noncardiac surgery subgroups. The quality of the articles and evidence were evaluated with a risk of bias tool and GRADE.
We included 29 randomized controlled trials with 3,468 patients. Goal-directed therapy significantly reduced the duration of hospital stay (mean difference -1.43 days; 95%CI 2.07 to -0.79; I2 81%), intensive care unit stay (mean difference -0.77 days; 95%CI -1.18 to -0.36; I2 93%), and mechanical ventilation (mean difference -2.48 hours, 95%CI -4.10 to -0.86, I2 63%). There was no statistically significant difference in mortality, myocardial infarction, acute kidney injury or hypotension, but goal-directed therapy significantly reduced the risk of heart failure or pulmonary edema (RR 0.46; 95%CI 0.23 - 0.92; I2 0%).
Goal-directed therapy guided by the FloTrac sensor improved clinical outcomes and shortened the length of stay in the hospital and intensive care unit in patients undergoing major surgery. Further research can validate these results using specific protocols and better understand the potential benefits of FloTrac beyond these outcomes.
Abstract
Rev Bras Ter Intensiva. 2020;32(1):49-57
DOI 10.5935/0103-507X.20200009
To characterize a cohort of acute-on-chronic liver failure patients in Intensive Care and to analyze the all-cause 28-day mortality risk factors assessed at ICU admission and day 3.
This was a retrospective cohort study of consecutive patients admitted to the intensive care unit between March 2013 and December 2016.
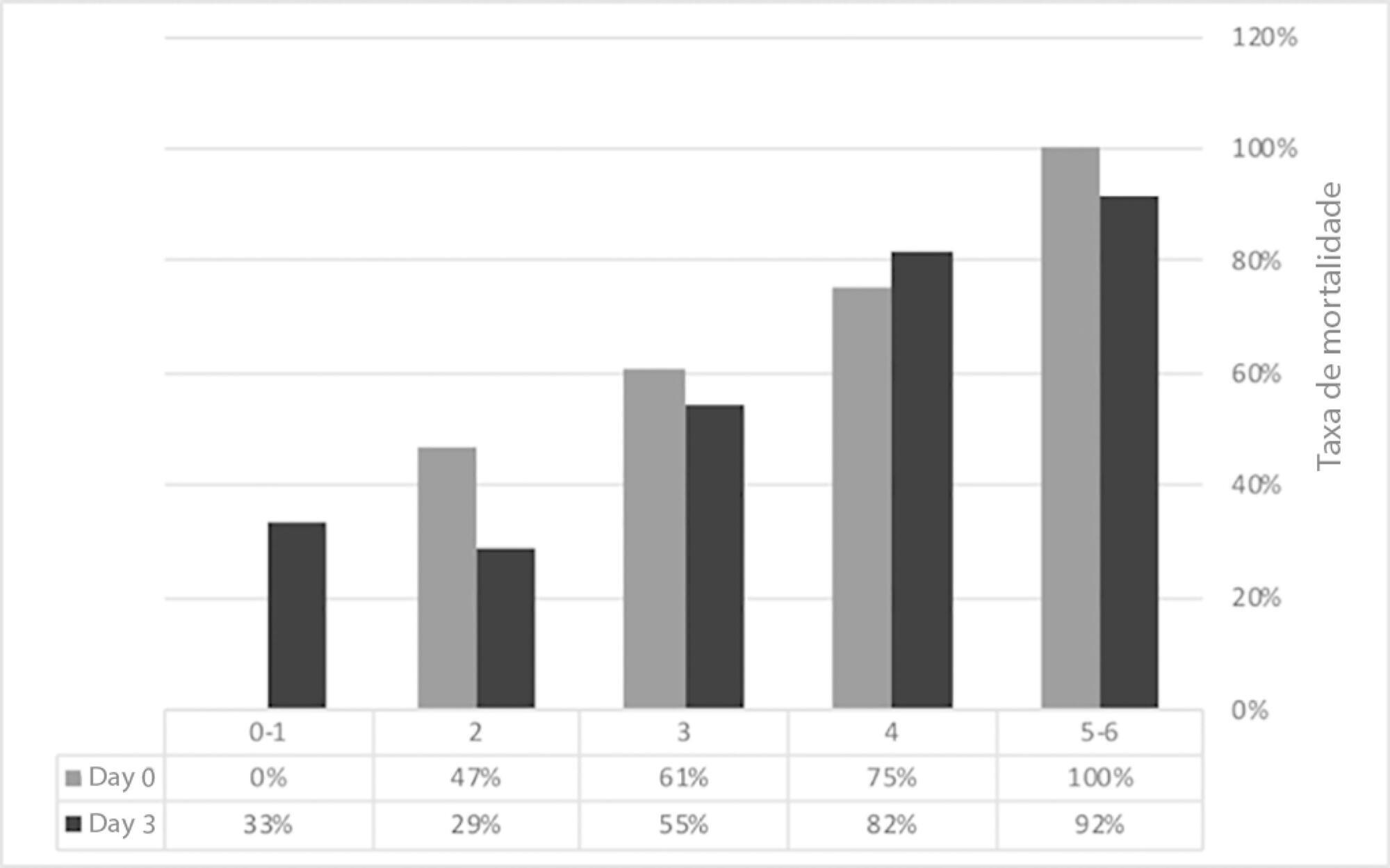
Seventy-one patients were included. The median age was 59 (51 - 64) years, and 81.7% of patients were male. Alcohol consumption alone (53.5%) was the most frequent etiology of cirrhosis and infection (53.5%) was the most common acute-on-chronic liver failure precipitating event. At intensive care unit admission, the clinical severity scores were APACHE II 21 (16 - 23), CLIF-SOFA 13 (11 - 15), Child-Pugh 12 (10 - 13) and MELD 27 (20 - 32). The acute-on-chronic liver failure scores were no-acute-on-chronic liver failure: 11.3%; one: 14.1%; two: 28.2% and three: 46.5%; and the number of organ failures was one: 4.2%; two: 42.3%; three: 32.4%; four: 16.9%; and five: 4.2%. Liver transplantation was performed in 15.5% of patients. The twenty-eight-day mortality rate was 56.3%, and the in-ICU mortality rate was 49.3%. Organ failure at intensive care unit admission (p = 0.02; OR 2.1; 95%CI 1.2 - 3.9), lactate concentration on day 3 (p = 0.02; OR 6.3; 95%CI 1.4 - 28.6) and the international normalized ratio on day 3 (p = 0.03; OR 10.2; 95%CI 1.3 - 82.8) were independent risk factors.
Acute-on-chronic liver failure patients presented with high clinical severity and mortality rates. The number of organ failures at intensive care unit admission and the lactate and international normalized ratio on day 3 were independent risk factors for 28-day mortality. We consider intensive care essential for acute-on-chronic liver failure patients and timely liver transplant was vital for selected patients.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):47-54
DOI 10.5935/0103-507X.20170008
The purpose of this study was to evaluate the clinical/functional aspects and quality of life of chronic obstructive pulmonary disease patients who were discharged after an intensive care unit admission for acute respiratory failure.
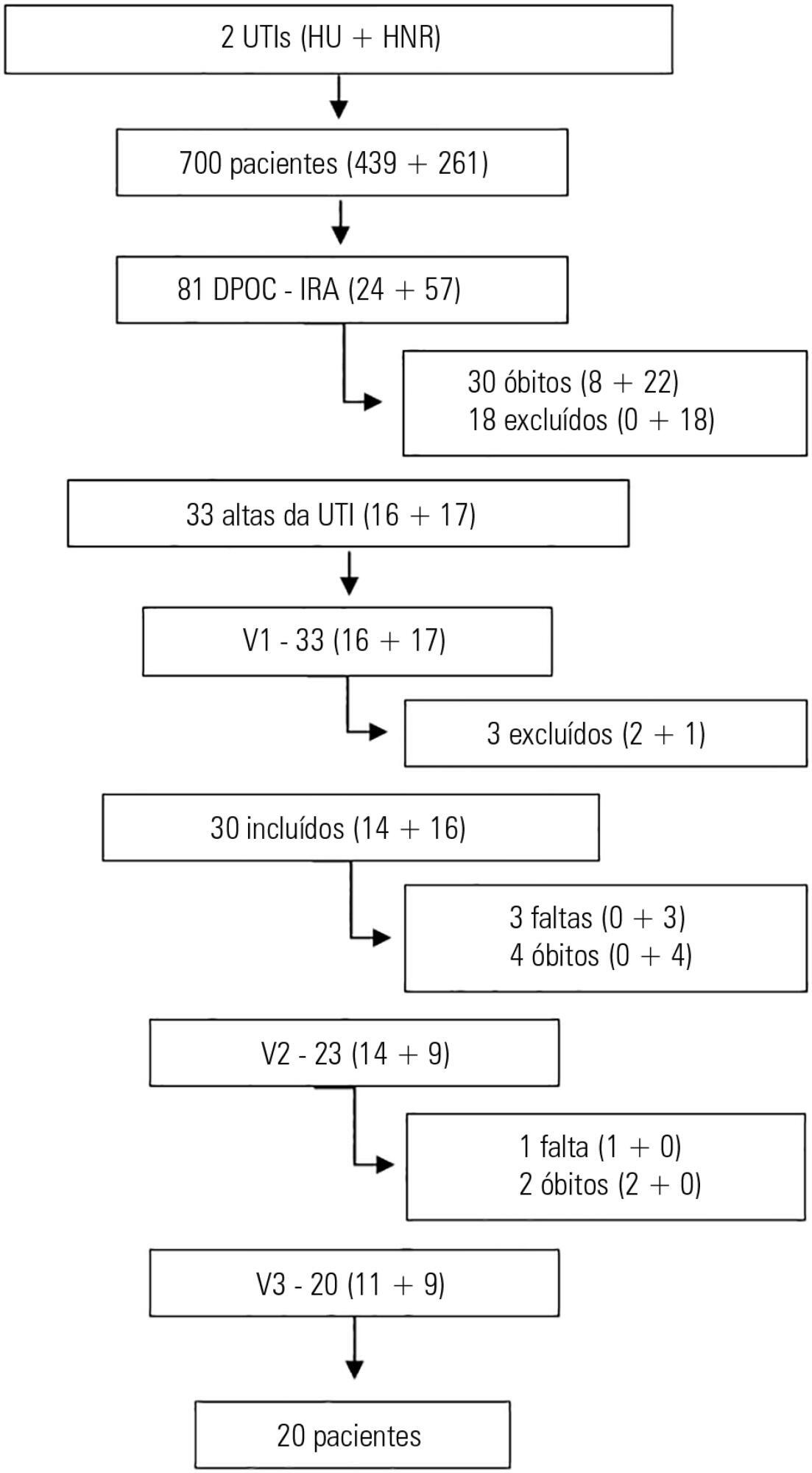
This prospective study included chronic obstructive pulmonary disease patients who were admitted to two intensive care units between December of 2010 and August of 2011 and evaluated over three visits after discharge. Thirty patients were included, and 20 patients completed the three-month follow up.
There was a significant improvement in the following: forced expiratory flow in one second (L) (1.1/1.4/1.4; p = 0.019), six-minute walk test (m) (- /232.8 /272.6; p = 0.04), BODE score (7.5/5.0/3.8; p = 0.001), cognition measured by the Mini Mental State Examination (21/23.5/23.5; p = 0.008) and quality of life measured by the total Saint George Respiratory Questionnaire score (63.3/56.8/51, p = 0.02). The mean difference in the total score was 12.3 (between visits 1 and three). Important clinical differences were observed for the symptom score (18.8), activities score (5.2) and impact score (14.3). The majority of participants (80%) reported they would be willing to undergo a new intensive care unit admission.
Despite the disease severity, there was a significant clinical, functional and quality of life improvement at the end of the third month. Most patients would be willing to undergo a new intensive care unit admission.
Abstract
Rev Bras Ter Intensiva. 2016;28(1):40-48
DOI 10.5935/0103-507X.20160012
This study sought to determine the influence of postoperative complications on the clinical outcomes of patients who underwent thoracic and gastrointestinal cancer surgery.
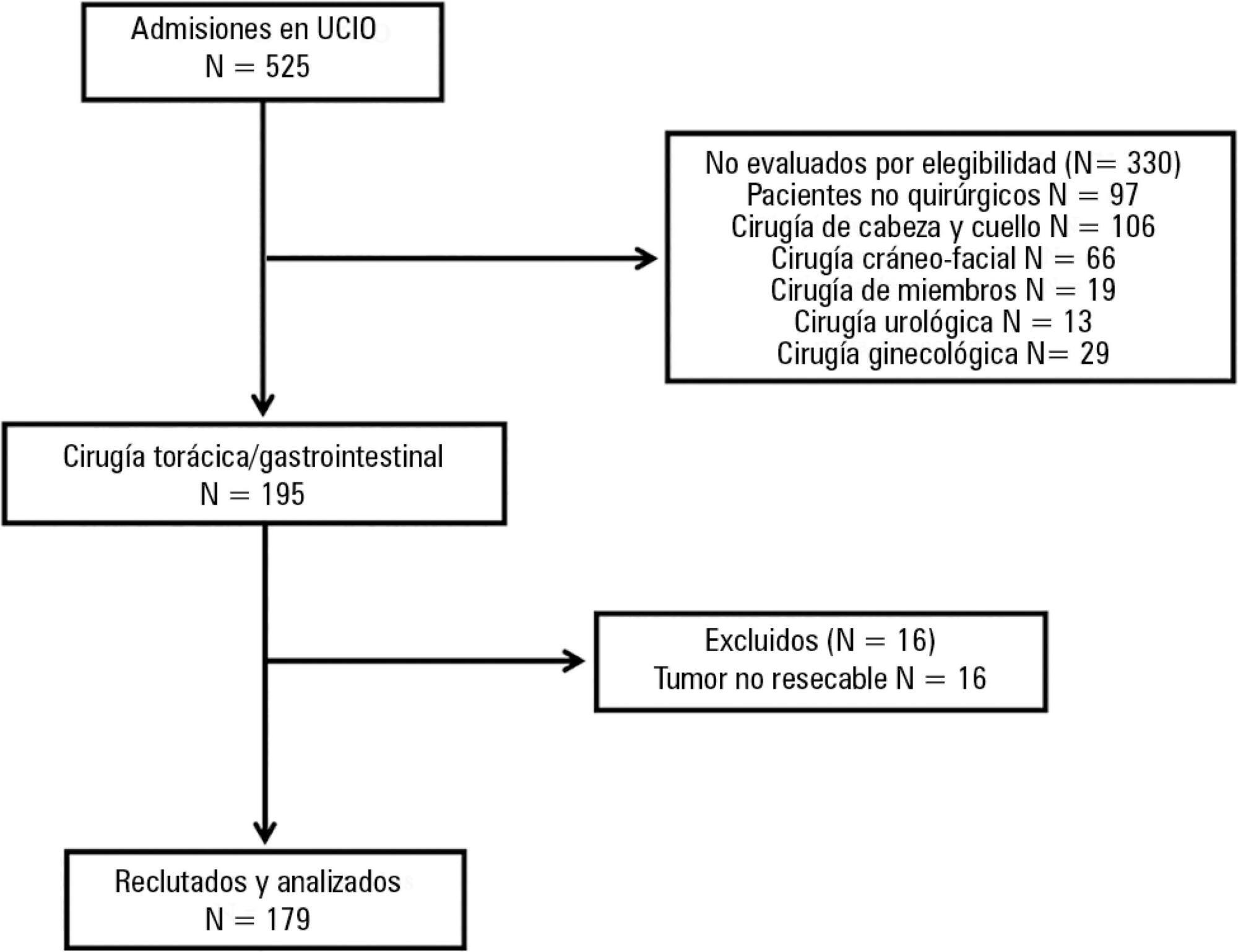
A prospective cohort study was conducted regarding 179 consecutive patients who received thorax or digestive tract surgery due to cancer and were admitted to an oncological intensive care unit. The Postoperative Morbidity Survey was used to evaluate the incidence of postoperative complications. The influence of postoperative complications on both mortality and length of hospital stay were also assessed.
Postoperative complications were found for 54 patients (30.2%); the most common complications were respiratory problems (14.5%), pain (12.9%), cardiovascular problems (11.7%), infectious disease (11.2%), and surgical wounds (10.1%). A multivariate logistic regression found that respiratory complications (OR = 18.68; 95%CI = 5.59 - 62.39; p < 0.0001), cardiovascular problems (OR = 5.06, 95%CI = 1.49 - 17.13; p = 0.009), gastrointestinal problems (OR = 26.09; 95%CI = 6.80 - 100.16; p < 0.0001), infectious diseases (OR = 20.55; 95%CI = 5.99 - 70.56; p < 0.0001) and renal complications (OR = 18.27; 95%CI = 3.88 - 83.35; p < 0.0001) were independently associated with hospital mortality. The occurrence of at least one complication increased the likelihood of remaining hospitalized (log-rank test, p = 0.002).
Postoperative complications are frequent disorders that are associated with poor clinical outcomes; thus, structural and procedural changes should be implemented to reduce postoperative morbidity and mortality.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):212-219
DOI 10.5935/0103-507X.20150034
To evaluate the clinical characteristics of patients with hematological disease admitted to the intensive care unit and the use of noninvasive mechanical ventilation in a subgroup with respiratory dysfunction.
A retrospective observational study from September 2011 to January 2014.
Overall, 157 patients were included. The mean age was 45.13 (± 17.2) years and 46.5% of the patients were female. Sixty-seven (48.4%) patients had sepsis, and 90 (57.3%) patients required vasoactive vasopressors. The main cause for admission to the intensive care unit was acute respiratory failure (94.3%). Among the 157 studied patients, 47 (29.9%) were intubated within the first 24 hours, and 38 (24.2%) underwent noninvasive mechanical ventilation. Among the 38 patients who initially received noninvasive mechanical ventilation, 26 (68.4%) were subsequently intubated, and 12 (31.6%) responded to this mode of ventilation. Patients who failed to respond to noninvasive mechanical ventilation had higher intensive care unit mortality (66.7% versus 16.7%; p = 0.004) and a longer stay in the intensive care unit (9.6 days versus 4.6 days, p = 0.02) compared with the successful cases. Baseline severity scores (SOFA and SAPS 3) and the total leukocyte count were not significantly different between these two subgroups. In a multivariate logistic regression model including the 157 patients, intubation at any time during the stay in the intensive care unit and SAPS 3 were independently associated with intensive care unit mortality, while using noninvasive mechanical ventilation was not.
In this retrospective study with severely ill hematologic patients, those who underwent noninvasive mechanical ventilation at admission and failed to respond to it presented elevated intensive care unit mortality. However, only intubation during the intensive care unit stay was independently associated with a poor outcome. Further studies are needed to define predictors of noninvasive mechanical ventilation failure.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):11-18
DOI 10.1590/S0103-507X2010000100004
OBJECTIVE: This study aimed to evaluate the outcome of cirrhotic patients admitted to Intensive Care Unit. METHODS: We conducted a prospective cohort of cirrhotic patients admitted to two intensive care unit between June 1999 to September 2004. We collected demographic, comorbid conditions, diagnosis, vital signs, laboratory data, prognostic scores and evolution in intensive care unit and hospital. The patients were divided in groups: non surgical, non liver surgery, surgery for portal hypertension, liver surgery, liver transplantation, and urgent surgery. RESULTS: We studied 304 patients, which 190 (62.5%) were male. The median of age was 54 (47-61) years. The mortality rate in intensive care unit and hospital were 29.3 and 39.8%, respectively, more elevated than in the other patients admitted critically ill patients (19.6 and 28.3%; p<0.001). Non surgical patients and those submitted to urgent surgery presented high mortality rate in the intensive care unit (64.3 and 65.4%) and in the hospital (80.4 and 76.9%). The variables related to hospital mortality were [Odds ratio (confidence interval 95%)]: mean arterial pressure [0.985 (0.974-0.997)]; mechanical ventilation in the first 24 h [4.080 (1.990-8.364)]; confirmed infection in the first 24 h [7.899 (2.814-22.175)]; acute renal failure [5.509 (1.708-17.766)] and APACHE II score (points) [1.078 (1.017-1.143)]. CONCLUSIONS: Cirrhotic patients had higher mortality rate compared to non cirrhotic critically ill patients. Those admitted after urgent surgery and non surgical had higher mortality rate.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)