Abstract
Rev Bras Ter Intensiva. 2020;32(3):426-432
DOI 10.5935/0103-507X.20200072
To evaluate the association between the incidence of delirium in the intensive care unit and quality of life 1 month after hospital discharge.
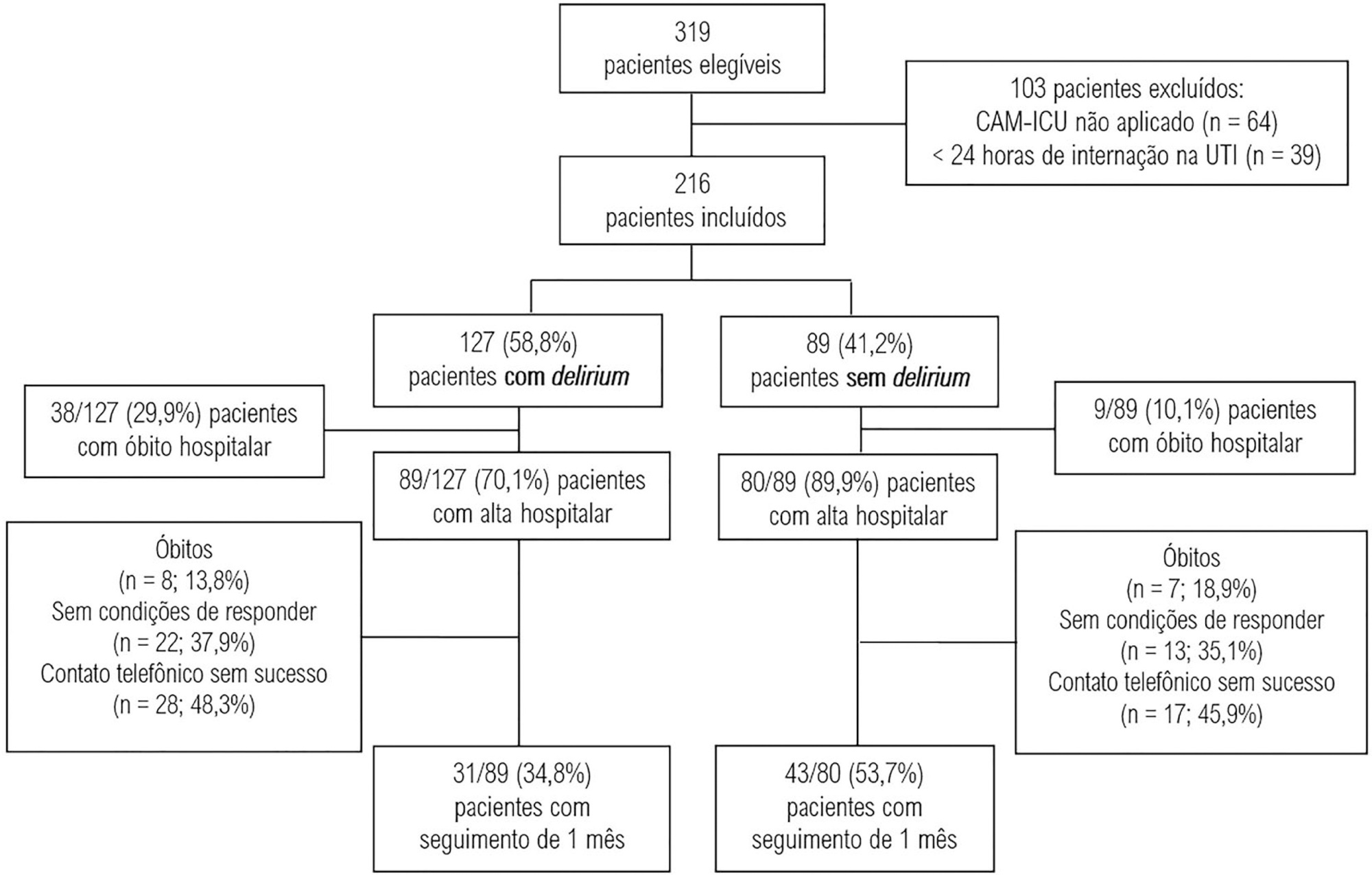
This was a prospective cohort study conducted in the intensive care units of two medium-complexity hospitals from December 2015 to December 2016. Delirium was identified using the Confusion Assessment Method for the Intensive Care Unit scale. At the time of hospital discharge, functional capacity and cognition were assessed with the Barthel index and the Mini Mental State Examination, respectively. Thirty days after patient discharge, the World Health Organization Quality of Life-BREF questionnaire was administered by telephone.
A total of 216 patients were included. Delirium was identified in 127 (58.8%) of them. Patients with delirium exhibited greater functional dependence (median Barthel index 50.0 [21.2 - 70.0] versus 80.0 [60.0 - 95.0]; p < 0.001) and lower cognition (Mini Mental State Examination score 12.9 ± 7.5 versus 20.7 ± 9.8; p < 0.001) at hospital discharge. There was no difference in any of the quality-of-life domains evaluated 1 month after hospital discharge between patients with and without delirium.
Our findings suggest that patients with delirium in the intensive care unit do not have worse quality of life 1 month after hospital discharge, despite presenting greater cognitive impairment and functional disability at the time of hospital discharge.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):47-54
DOI 10.5935/0103-507X.20170008
The purpose of this study was to evaluate the clinical/functional aspects and quality of life of chronic obstructive pulmonary disease patients who were discharged after an intensive care unit admission for acute respiratory failure.
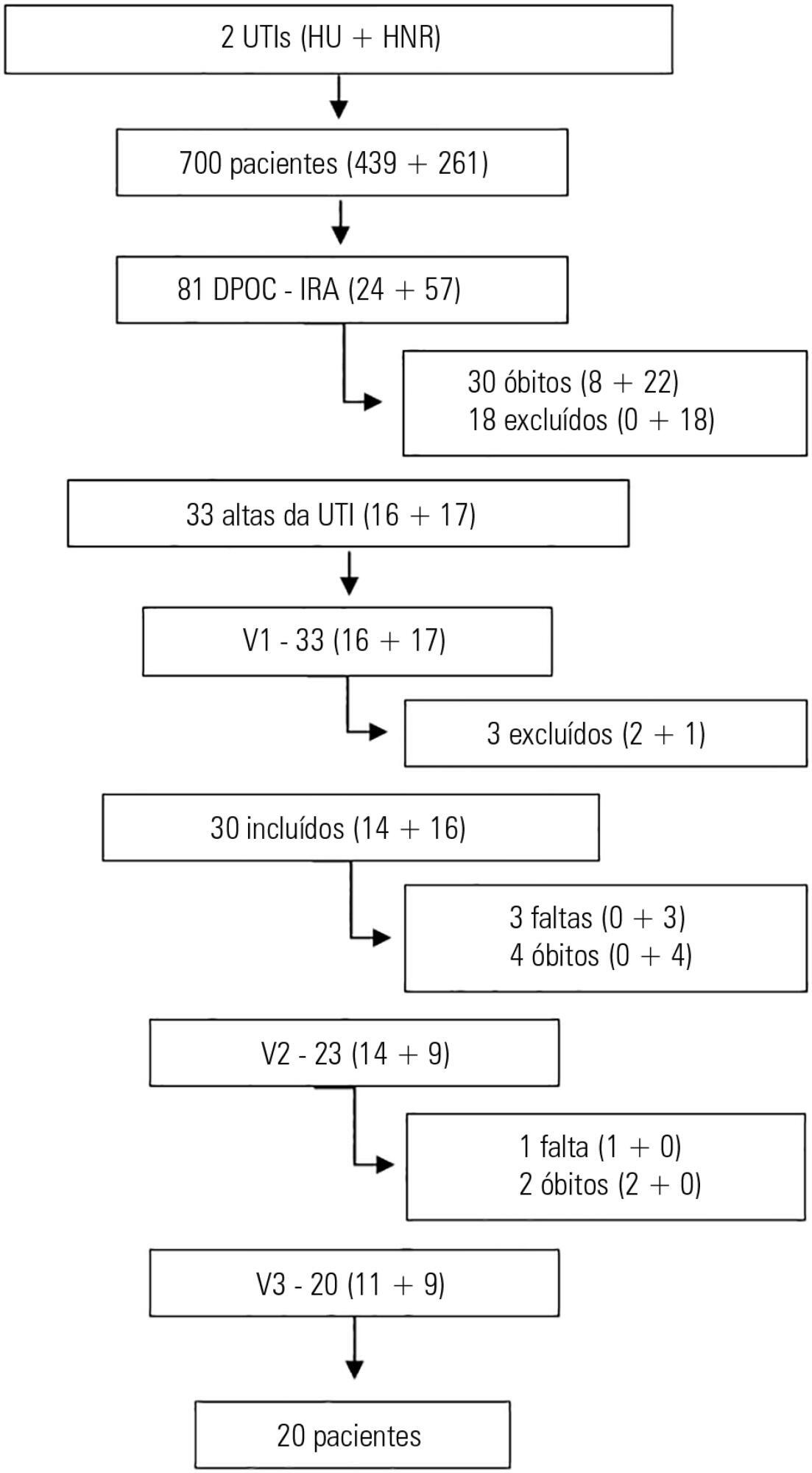
This prospective study included chronic obstructive pulmonary disease patients who were admitted to two intensive care units between December of 2010 and August of 2011 and evaluated over three visits after discharge. Thirty patients were included, and 20 patients completed the three-month follow up.
There was a significant improvement in the following: forced expiratory flow in one second (L) (1.1/1.4/1.4; p = 0.019), six-minute walk test (m) (- /232.8 /272.6; p = 0.04), BODE score (7.5/5.0/3.8; p = 0.001), cognition measured by the Mini Mental State Examination (21/23.5/23.5; p = 0.008) and quality of life measured by the total Saint George Respiratory Questionnaire score (63.3/56.8/51, p = 0.02). The mean difference in the total score was 12.3 (between visits 1 and three). Important clinical differences were observed for the symptom score (18.8), activities score (5.2) and impact score (14.3). The majority of participants (80%) reported they would be willing to undergo a new intensive care unit admission.
Despite the disease severity, there was a significant clinical, functional and quality of life improvement at the end of the third month. Most patients would be willing to undergo a new intensive care unit admission.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)