You searched for:"Marcio Manozzo Boniatti"
We found (8) results for your search.-
Original Article
Extubation failure and the use of noninvasive ventilation during the weaning process in critically ill COVID-19 patients
Crit Care Sci. 2023;35(2):163-167
Abstract
Original ArticleExtubation failure and the use of noninvasive ventilation during the weaning process in critically ill COVID-19 patients
Crit Care Sci. 2023;35(2):163-167
DOI 10.5935/2965-2774.20230009-pt
Views6ABSTRACT
Objective:
To assess the outcome of extubation in COVID-19 patients and the use of noninvasive ventilation in the weaning process.
Methods:
This retrospective, observational, single-center study was conducted in COVID-19 patients aged 18 years or older who were admitted to an intensive care unit between April 2020 and December 2021, placed under mechanical ventilation for more than 48 hours and progressed to weaning. Early extubation was defined as extubation without a spontaneous breathing trial and immediate use of noninvasive ventilation after extubation. In patients who underwent a spontaneous breathing trial, noninvasive ventilation could be used as prophylactic ventilatory assistance when started immediately after extubation (prophylactic noninvasive ventilation) or as rescue therapy in cases of postextubation respiratory failure (therapeutic noninvasive ventilation). The primary outcome was extubation failure during the intensive care unit stay.
Results:
Three hundred eighty-four extubated patients were included. Extubation failure was observed in 107 (27.9%) patients. Forty-seven (12.2%) patients received prophylactic noninvasive ventilation. In 26 (6.8%) patients, early extubation was performed with immediate use of noninvasive ventilation. Noninvasive ventilation for the management of postextubation respiratory failure was administered to 64 (16.7%) patients.
Conclusion:
We found that COVID-19 patients had a high rate of extubation failure. Despite the high risk of extubation failure, we observed low use of prophylactic noninvasive ventilation in these patients.
Keywords:Airway extubationartificialCoronavirus infectionsCOVID-19Noninvasive ventilationRespirationSARS-CoV-2Ventilator weaningSee more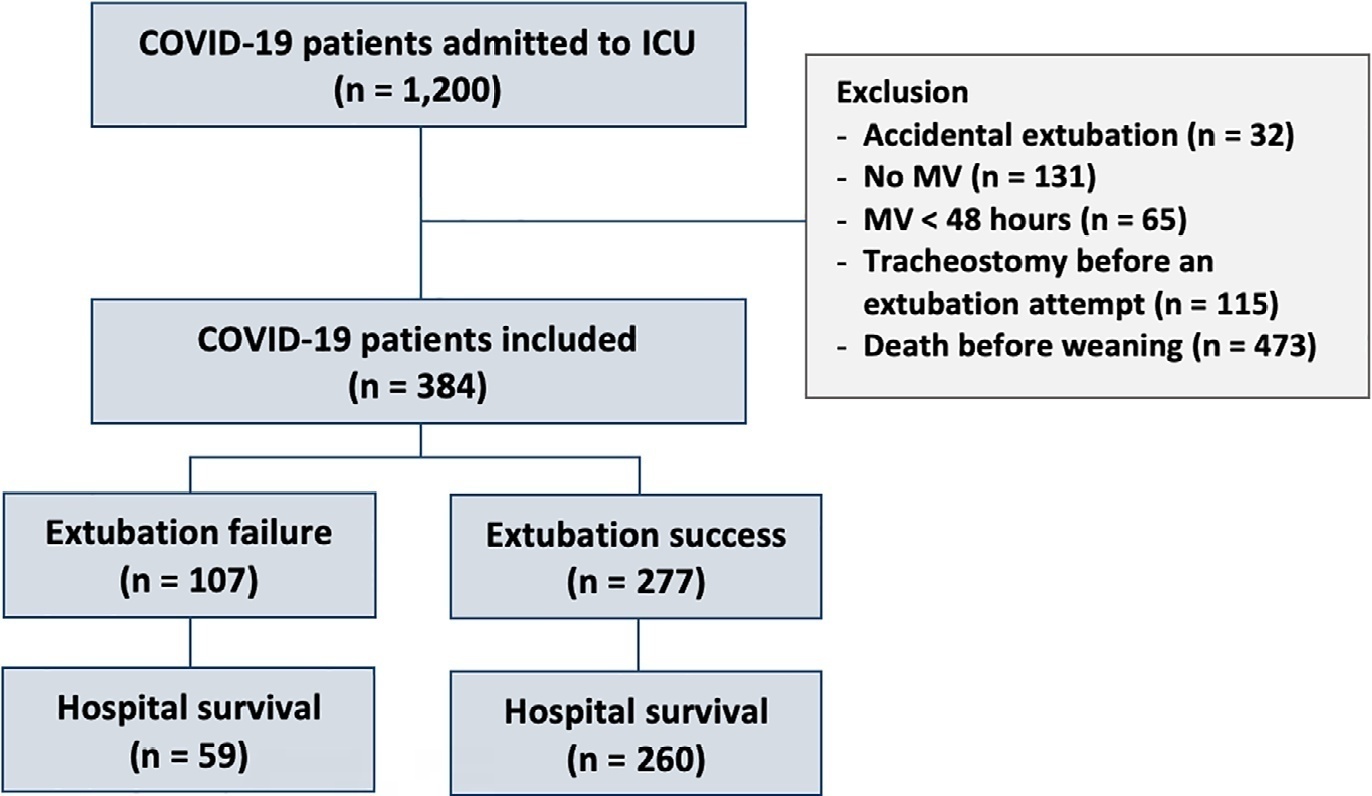
-
Original Article
Postextubation fluid balance is associated with extubation failure: a cohort study
Rev Bras Ter Intensiva. 2021;33(3):422-427
Abstract
Original ArticlePostextubation fluid balance is associated with extubation failure: a cohort study
Rev Bras Ter Intensiva. 2021;33(3):422-427
DOI 10.5935/0103-507X.20210057
Views1ABSTRACT
Objective:
To assess whether there is an association between 48-hour postextubation fluid balance and extubation failure.
Methods:
This was a prospective cohort study that included patients admitted to the intensive care unit of a tertiary hospital in southern Brazil from March 2019 to December 2019. Patients who required mechanical ventilation for at least 24 hours and who were extubated during the study period were included. The primary outcome was extubation failure, considered as the need for reintubation in the first 72 hours after extubation. The secondary outcome was a combined outcome with extubation failure or the need for therapeutic noninvasive ventilation.
Results:
A total of 101 patients were included. Extubation failure was observed in 29 (28.7%) patients. In univariate analysis, patients with a negative 48-hour postextubation fluid balance higher than one liter had a lower rate of extubation failure (12.0%) than patients with a negative 48-hour postextubation fluid balance lower than 1L (34.2%; p = 0.033). Mechanical ventilation duration and negative 48-hour postextubation fluid balance lower than one liter were associated with extubation failure when corrected for Simplified Acute Physiology Score 3 in multivariate analysis. When we evaluated the combined outcome, only negative 48-hour postextubation lower than 1L maintained an association when corrected for for Simplified Acute Physiology Score 3 and mechanical ventilation duration.
Conclusion:
The 48-hour postextubation fluid balance is associated with extubation failure. Further studies are necessary to assess whether avoiding positive fluid balance in this period might improve weaning outcomes.
Keywords:Airway extubationNoninvasive ventilationRespiration, artificialWater-electrolyte balanceWeaningSee more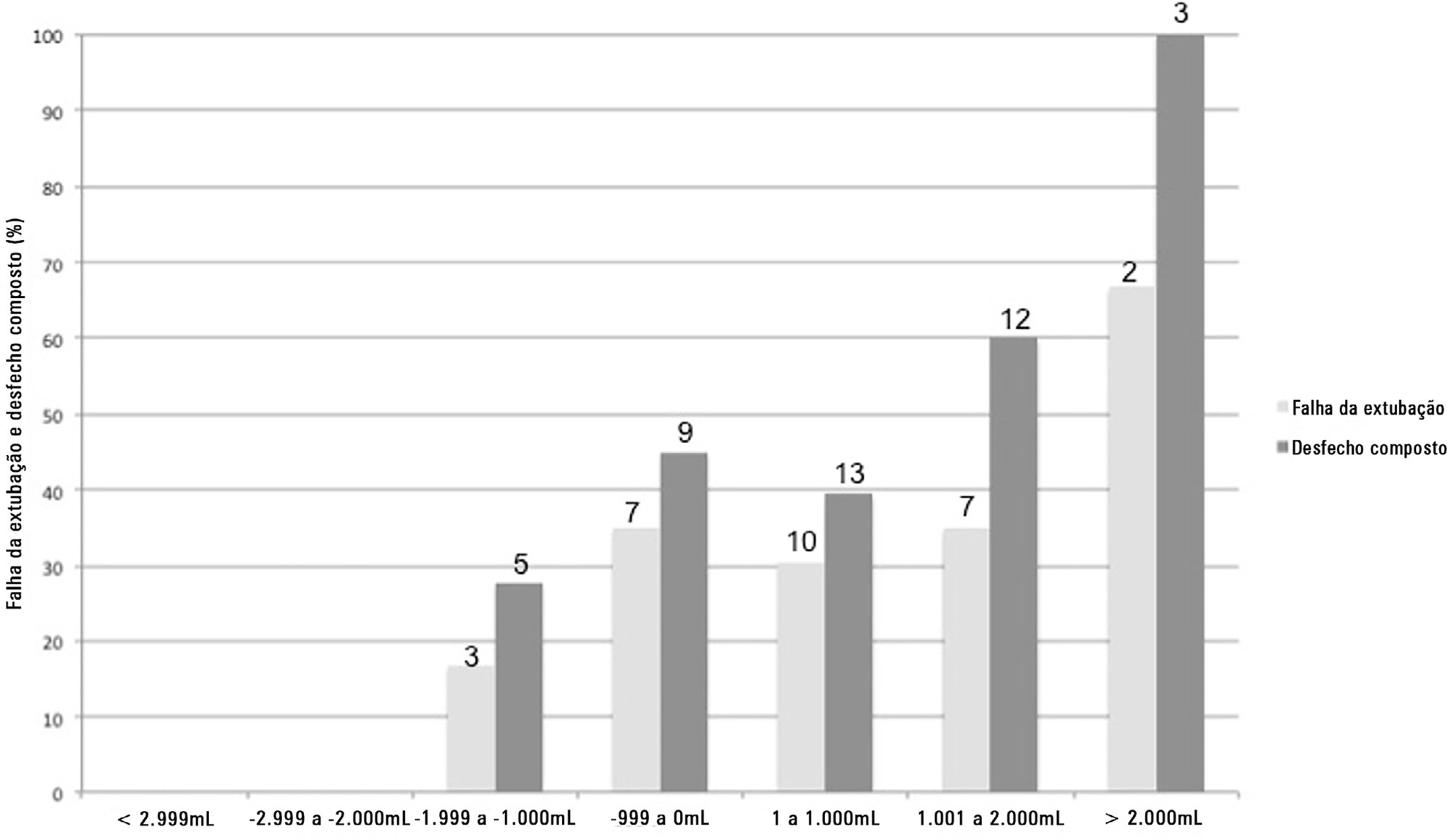
-
Original Article
Changes in cardiac arrest profiles after the implementation of a Rapid Response Team
Rev Bras Ter Intensiva. 2021;33(1):96-101
Abstract
Original ArticleChanges in cardiac arrest profiles after the implementation of a Rapid Response Team
Rev Bras Ter Intensiva. 2021;33(1):96-101
DOI 10.5935/0103-507X.20210010
Views1See moreABSTRACT
Objective:
To evaluate changes in the characteristics of in-hospital cardiac arrest after the implementation of a Rapid Response Team.
Methods:
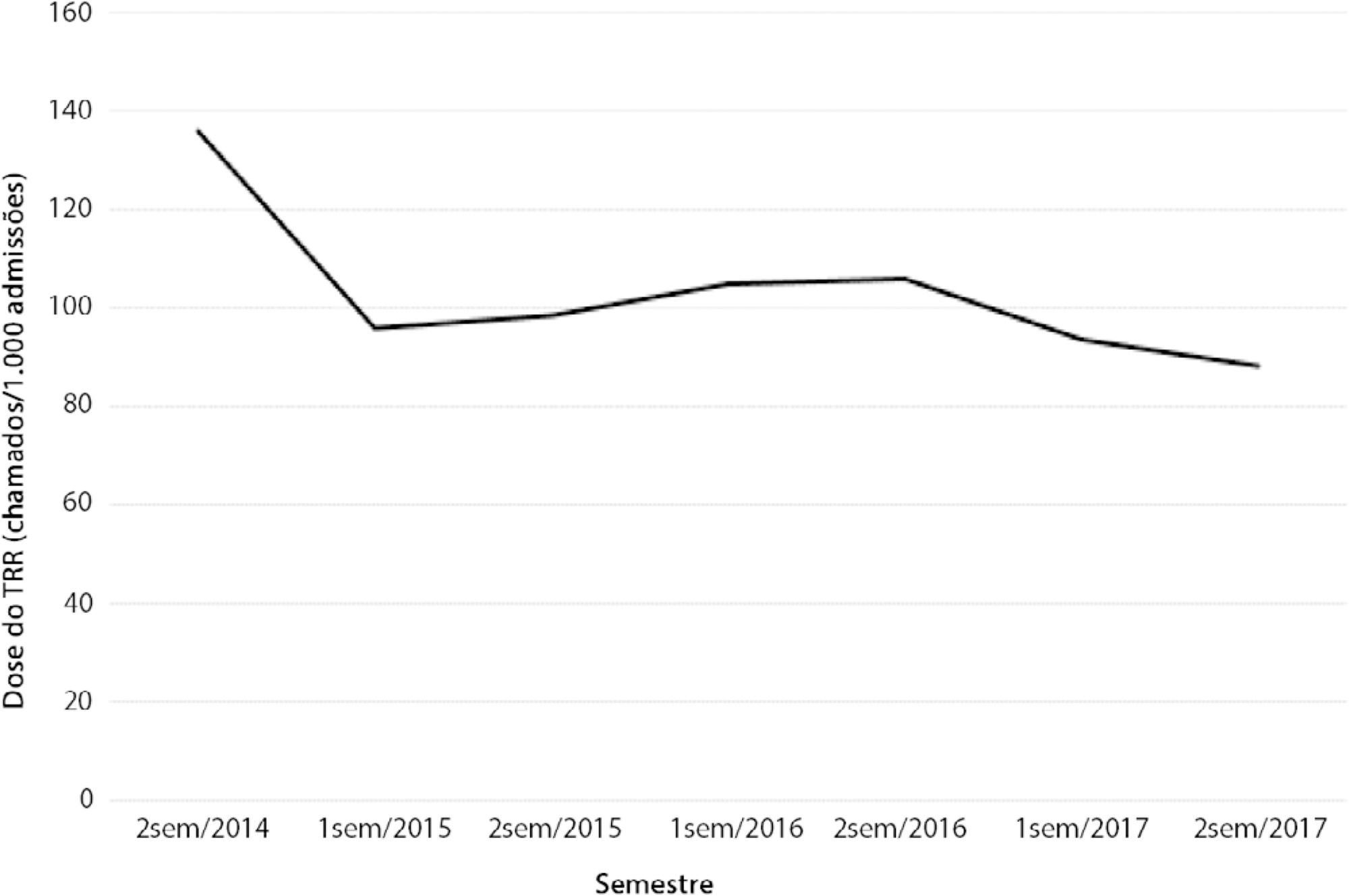
This was a prospective observational study of in-hospital cardiac arrest that occurred from January 2013 to December 2017. The exclusion criterion was in-hospital cardiac arrest in the intensive care unit, emergency room or operating room. The Rapid Response Team was implemented in July 2014 in the study hospital. Patients were classified into two groups: a Pre-Rapid Response Team (in-hospital cardiac arrest before Rapid Response Team implementation) and a Post-Rapid Response Team (in-hospital cardiac arrest after Rapid Response Team implementation). Patients were followed until hospital discharge or death.
Results:
We had a total of 308 cardiac arrests (64.6 ± 15.2 years, 60.3% men, 13.9% with initial shockable rhythm). There was a decrease from 4.2 to 2.5 in-hospital cardiac arrest/1000 admissions after implementation of the Rapid Response Team, and we had approximately 124 calls/1000 admissions. Pre-Rapid Response Team cardiac arrest was associated with more hypoxia (29.4 versus 14.3%; p = 0.006) and an altered respiratory rate (14.7 versus 4.2%; p = 0.004) compared with post-Rapid Response Team cardiac arrest. Cardiac arrest due to hypoxia was more common before Rapid Response Team implementation (61.2 versus 38.1%, p < 0.001). In multivariate analysis, return of spontaneous circulation was associated with shockable rhythm (OR 2.97; IC95% 1.04 - 8.43) and witnessed cardiac arrest (OR 2.52; IC95% 1.39 - 4.59) but not with Rapid Response Team implementation (OR 1.40; IC95% 0.70 - 2.81) or premonitory signs (OR 0.71; IC95% 0.39 - 1.28). In multivariate analysis, in-hospital mortality was associated with non-shockable rhythm (OR 5.34; IC95% 2.28 - 12.53) and age (OR 1.03; IC95% 1.01 - 1.05) but not with Rapid Response Team implementation (OR 0.89; IC95% 0.40 - 2.02).
Conclusion:
Even though Rapid Response Team implementation is associated with a reduction in in-hospital cardiac arrest, it was not associated with the mortality of in-hospital cardiac arrest victims. A significant decrease in cardiac arrests due to respiratory causes was noted after Rapid Response Team implementation.
-
Original Article
Delirium and quality of life in critically ill patients: a prospective cohort study
Rev Bras Ter Intensiva. 2020;32(3):426-432
Abstract
Original ArticleDelirium and quality of life in critically ill patients: a prospective cohort study
Rev Bras Ter Intensiva. 2020;32(3):426-432
DOI 10.5935/0103-507X.20200072
Views0Abstract
Objective:
To evaluate the association between the incidence of delirium in the intensive care unit and quality of life 1 month after hospital discharge.
Methods:
This was a prospective cohort study conducted in the intensive care units of two medium-complexity hospitals from December 2015 to December 2016. Delirium was identified using the Confusion Assessment Method for the Intensive Care Unit scale. At the time of hospital discharge, functional capacity and cognition were assessed with the Barthel index and the Mini Mental State Examination, respectively. Thirty days after patient discharge, the World Health Organization Quality of Life-BREF questionnaire was administered by telephone.
Results:
A total of 216 patients were included. Delirium was identified in 127 (58.8%) of them. Patients with delirium exhibited greater functional dependence (median Barthel index 50.0 [21.2 – 70.0] versus 80.0 [60.0 – 95.0]; p < 0.001) and lower cognition (Mini Mental State Examination score 12.9 ± 7.5 versus 20.7 ± 9.8; p < 0.001) at hospital discharge. There was no difference in any of the quality-of-life domains evaluated 1 month after hospital discharge between patients with and without delirium.
Conclusion:
Our findings suggest that patients with delirium in the intensive care unit do not have worse quality of life 1 month after hospital discharge, despite presenting greater cognitive impairment and functional disability at the time of hospital discharge.
Keywords:CognitionDeliriumIntensive care unitsPatient dischargePhysical functional performanceQuality of lifeSee more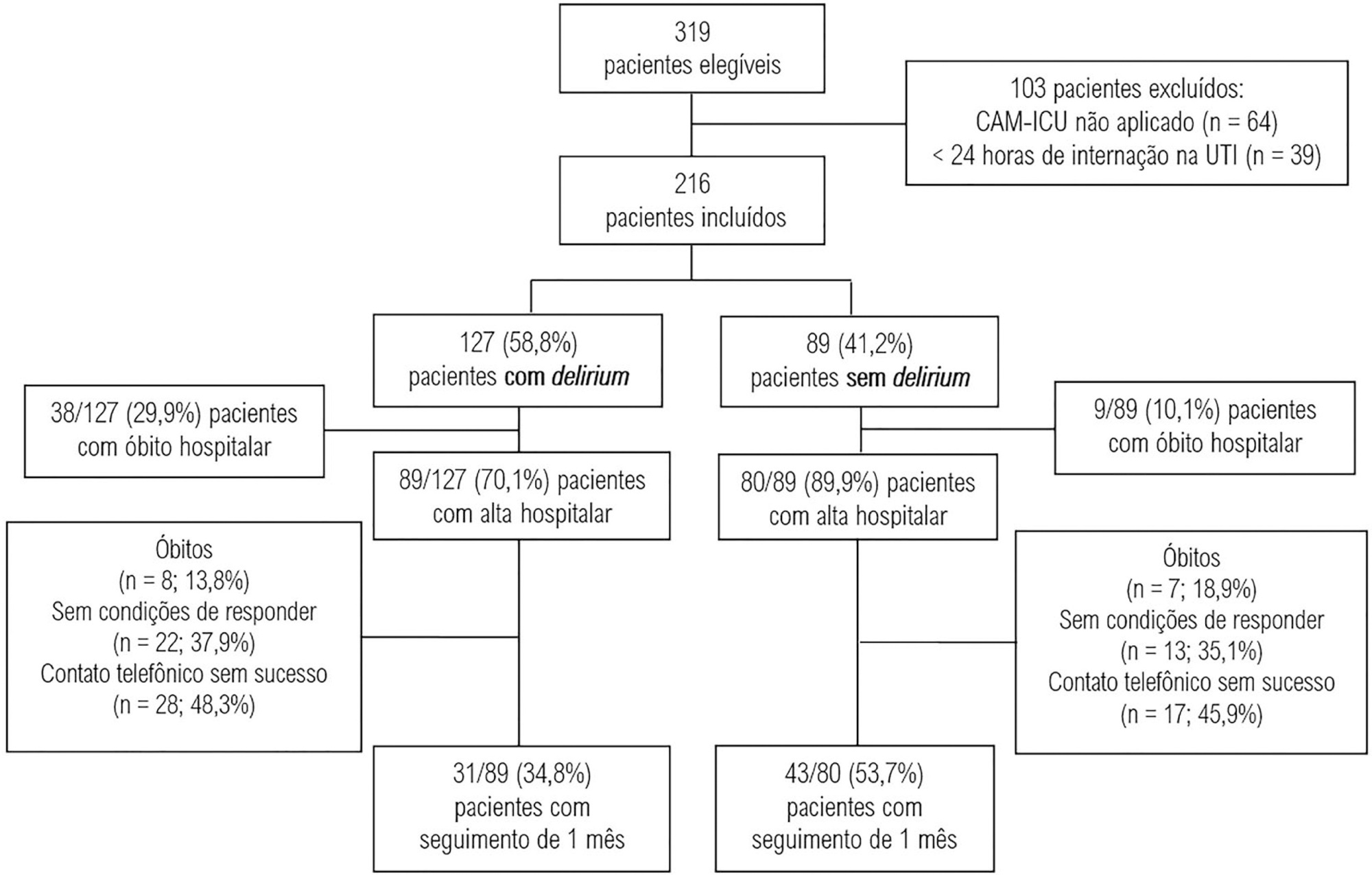
-
Original Article
Use of the Modified Early Warning Score in intrahospital transfer of patients
Rev Bras Ter Intensiva. 2020;32(3):439-443
Abstract
Original ArticleUse of the Modified Early Warning Score in intrahospital transfer of patients
Rev Bras Ter Intensiva. 2020;32(3):439-443
DOI 10.5935/0103-507X.20200074
Views0See moreAbstract
Objective:
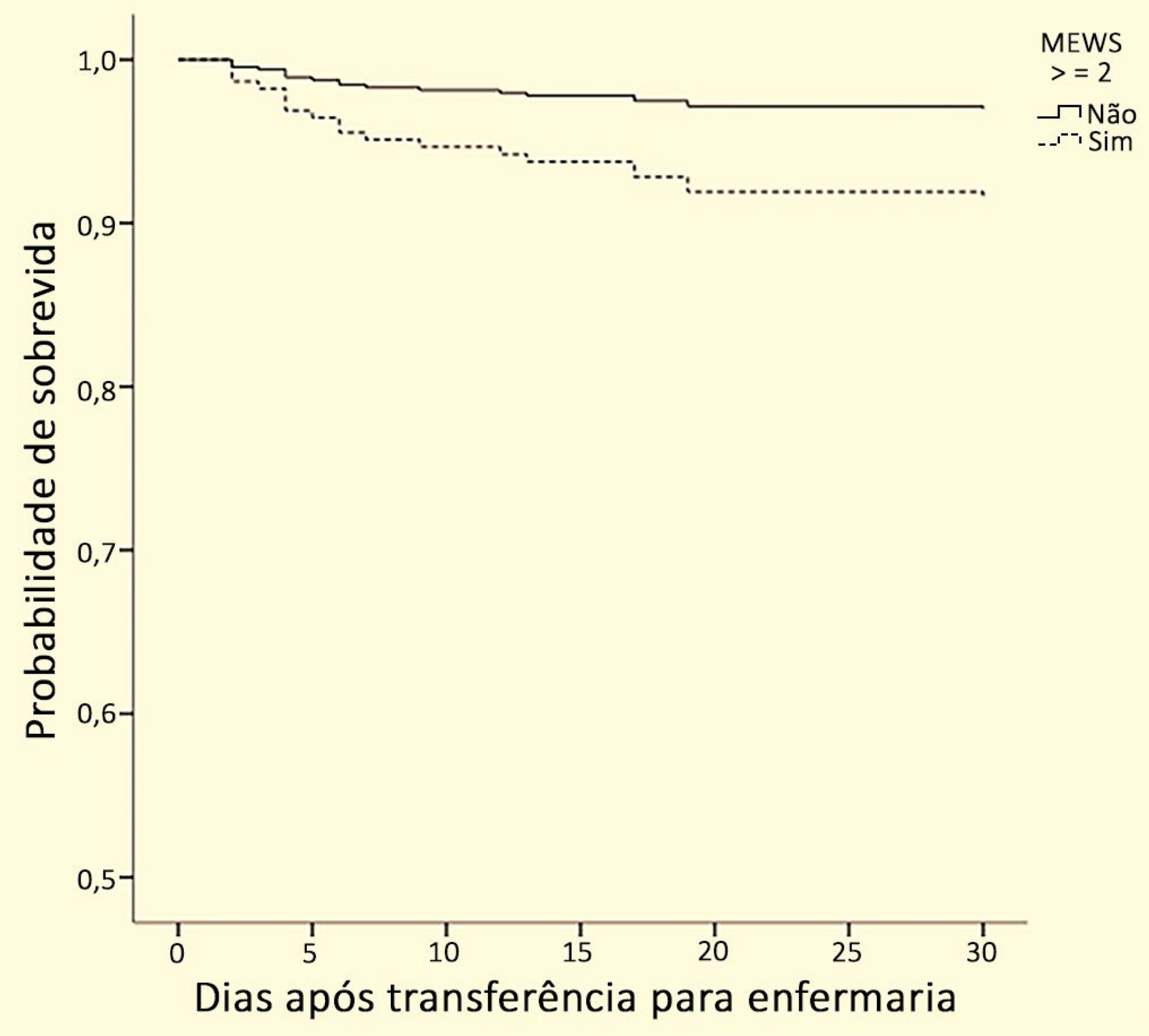
To verify whether there is an association between the Modified Early Warning Score before the transfer from the emergency room to the ward and death or admission to the intensive care unit within 30 days.
Methods:
This is a historical cohort study conducted in a high-complexity hospital in southern Brazil with patients who were transferred from the emergency room to the ward between January and June 2017. The following data were collected: sociodemographic variables; comorbidities, as determined by the Charlson index; reason for hospitalization; Modified Early Warning Score at the time of transfer; admission to the intensive care unit; care by the Rapid Response Team; mortality within 30 days; and hospital mortality.
Results:
A total of 278 patients were included in the study. Regarding the Modified Early Warning Score, patients who died within 30 days had a significantly higher score than surviving patients during this period (2.0 [1.0 – 3.0] versus 1.0 [1.0 – 2.0], respectively; p = 0.006). The areas under the receiver operating characteristic curve for death within 30 days and for ICU admission were 0.67 (0.55 – 0.80; p = 0.012) and 0.72 (0.59 – 0.84; p = 0.02), respectively, with a Modified Early Warning Score cutoff of ≥ 2. In the Cox regression, the Modified Early Warning Score was independently associated with mortality within 30 days after multivariate adjustment (hazard ratio 2.91; 95% confidence interval 1.04 – 8.13).
Conclusion:
The Modified Early Warning Score before intrahospital transfer from the emergency room to the ward is associated with admission to the intensive care unit and death within 30 days. The Modified Early Warning Score can be an important indicator for monitoring these patients and can prompt the receiving team to take specific actions.
-
Editorials
Advances in performance, more benefits… the perspectives of rapid response teams
Rev Bras Ter Intensiva. 2016;28(3):217-219
Abstract
EditorialsAdvances in performance, more benefits… the perspectives of rapid response teams
Rev Bras Ter Intensiva. 2016;28(3):217-219
DOI 10.5935/0103-507X.20160048
Views0Rapid response teams (RRT) emerged in 1990 with the goals of improving the identification of ward patients with clinical deterioration and offering, based on this identification, early intervention.(–) An RRT is activated according to previously defined triggers, traditionally vital signs, by themselves or as part of aggregated scores, other clinical changes, such as seizures, or […]See more -
Original Articles
The reality of patients requiring prolonged mechanical ventilation: a multicenter study
Rev Bras Ter Intensiva. 2015;27(1):26-35
Abstract
Original ArticlesThe reality of patients requiring prolonged mechanical ventilation: a multicenter study
Rev Bras Ter Intensiva. 2015;27(1):26-35
DOI 10.5935/0103-507X.20150006
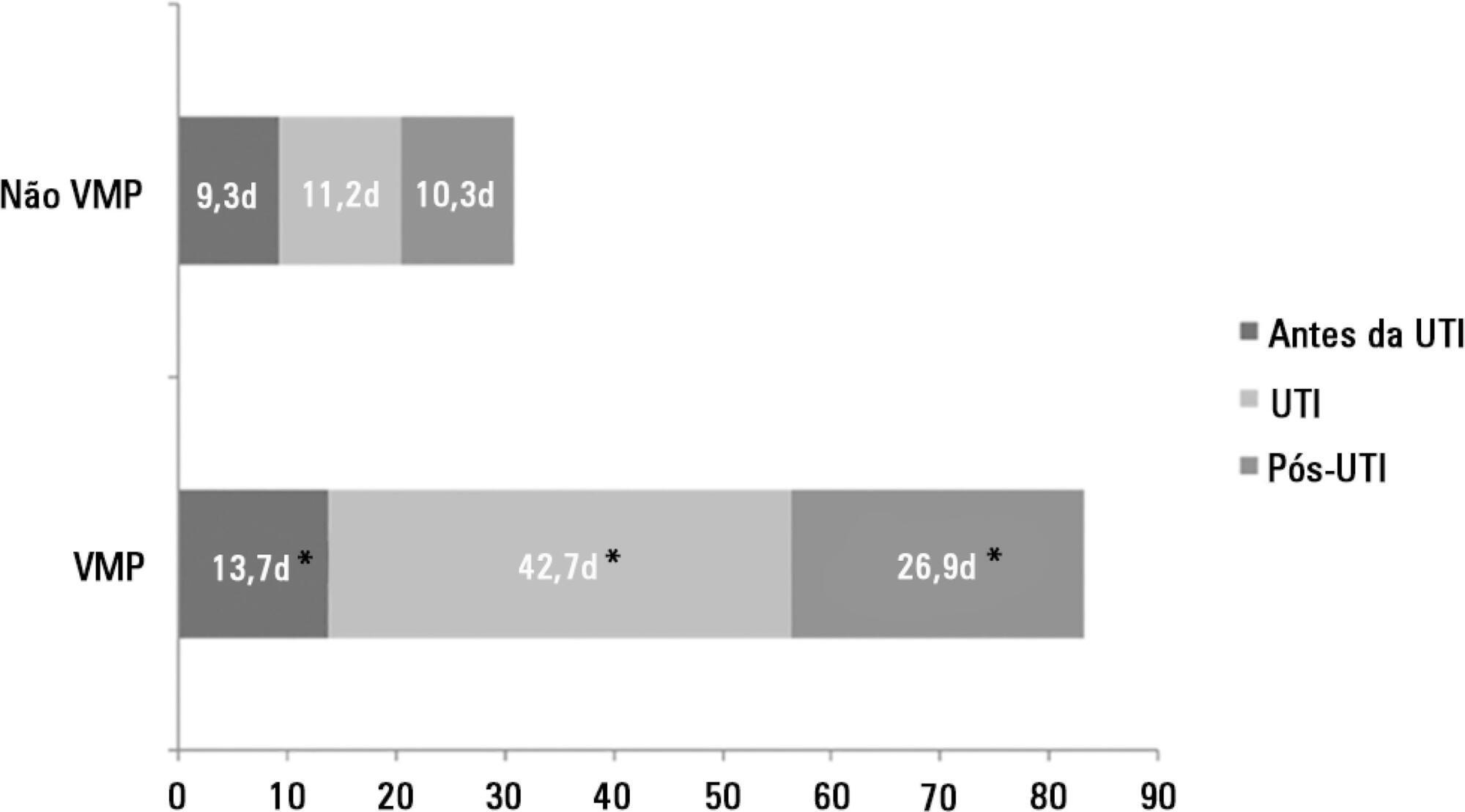
Views5See moreObjective:
The number of patients who require prolonged mechanical ventilation increased during the last decade, which generated a large population of chronically ill patients. This study established the incidence of prolonged mechanical ventilation in four intensive care units and reported different characteristics, hospital outcomes, and the impact of costs and services of prolonged mechanical ventilation patients (mechanical ventilation dependency ≥ 21 days) compared with non-prolonged mechanical ventilation patients (mechanical ventilation dependency < 21 days).
Methods:
This study was a multicenter cohort study of all patients who were admitted to four intensive care units. The main outcome measures were length of stay in the intensive care unit, hospital, complications during intensive care unit stay, and intensive care unit and hospital mortality.
Results:
There were 5,287 admissions to the intensive care units during study period. Some of these patients (41.5%) needed ventilatory support (n = 2,197), and 218 of the patients met criteria for prolonged mechanical ventilation (9.9%). Some complications developed during intensive care unit stay, such as muscle weakness, pressure ulcers, bacterial nosocomial sepsis, candidemia, pulmonary embolism, and hyperactive delirium, were associated with a significantly higher risk of prolonged mechanical ventilation. Prolonged mechanical ventilation patients had a significant increase in intensive care unit mortality (absolute difference = 14.2%, p < 0.001) and hospital mortality (absolute difference = 19.1%, p < 0.001). The prolonged mechanical ventilation group spent more days in the hospital after intensive care unit discharge (26.9 ± 29.3 versus 10.3 ± 20.4 days, p < 0.001) with higher costs.
Conclusion:
The classification of chronically critically ill patients according to the definition of prolonged mechanical ventilation adopted by our study (mechanical ventilation dependency ≥ 21 days) identified patients with a high risk for complications during intensive care unit stay, longer intensive care unit and hospital stays, high death rates, and higher costs.
-
Original Articles
Inflammatory and perfusion markers as risk factors and predictors of critically ill patient readmission
Rev Bras Ter Intensiva. 2014;26(2):130-136
Abstract
Original ArticlesInflammatory and perfusion markers as risk factors and predictors of critically ill patient readmission
Rev Bras Ter Intensiva. 2014;26(2):130-136
DOI 10.5935/0103-507X.20140019
Views0Objective:
To assess the performance of central venous oxygen saturation, lactate, base deficit, and C-reactive protein levels and SOFA and SWIFT scores on the day of discharge from the intensive care unit as predictors of patient readmission to the intensive care unit.
Methods:
This prospective and observational study collected data from 1,360 patients who were admitted consecutively to a clinical-surgical intensive care unit from August 2011 to August 2012. The clinical characteristics and laboratory data of readmitted and non-readmitted patients after discharge from the intensive care unit were compared. Using a multivariate analysis, the risk factors independently associated with readmission were identified.
Results:
The C-reactive protein, central venous oxygen saturation, base deficit, and lactate levels and the SWIFT and SOFA scores did not correlate with the readmission of critically ill patients. Increased age and contact isolation because of multidrug-resistant organisms were identified as risk factors that were independently associated with readmission in this study group.
Conclusion:
Inflammatory and perfusion parameters were not associated with patient readmission. Increased age and contact isolation because of multidrug-resistant organisms were identified as predictors of readmission to the intensive care unit.
Keywords:C-reactive proteinLactatePatient readmissionPatient readmission/economicsPatient safetyrisk factorsSee more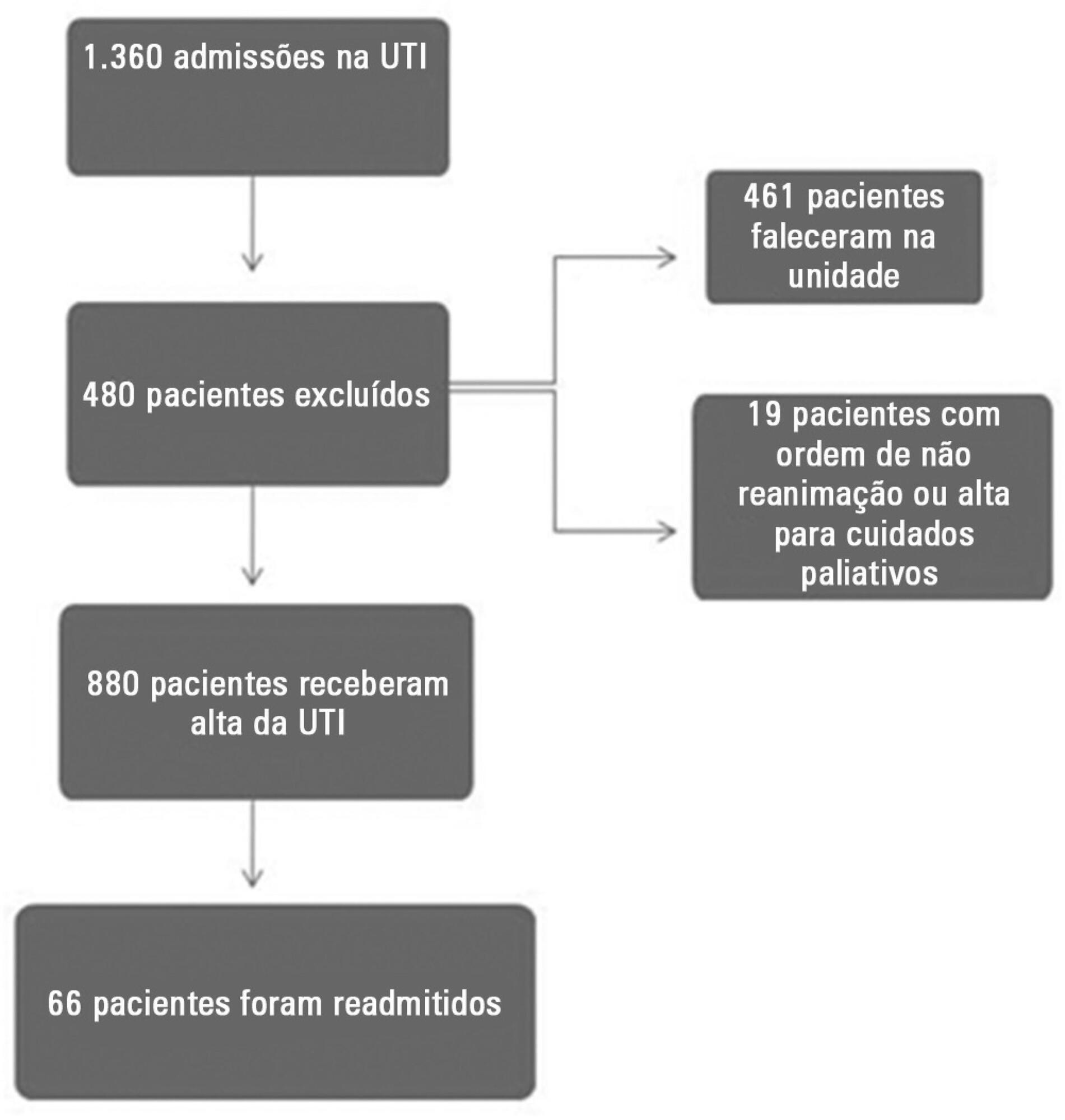
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis Septic shock




