Abstract
Rev Bras Ter Intensiva. 2020;32(3):439-443
DOI 10.5935/0103-507X.20200074
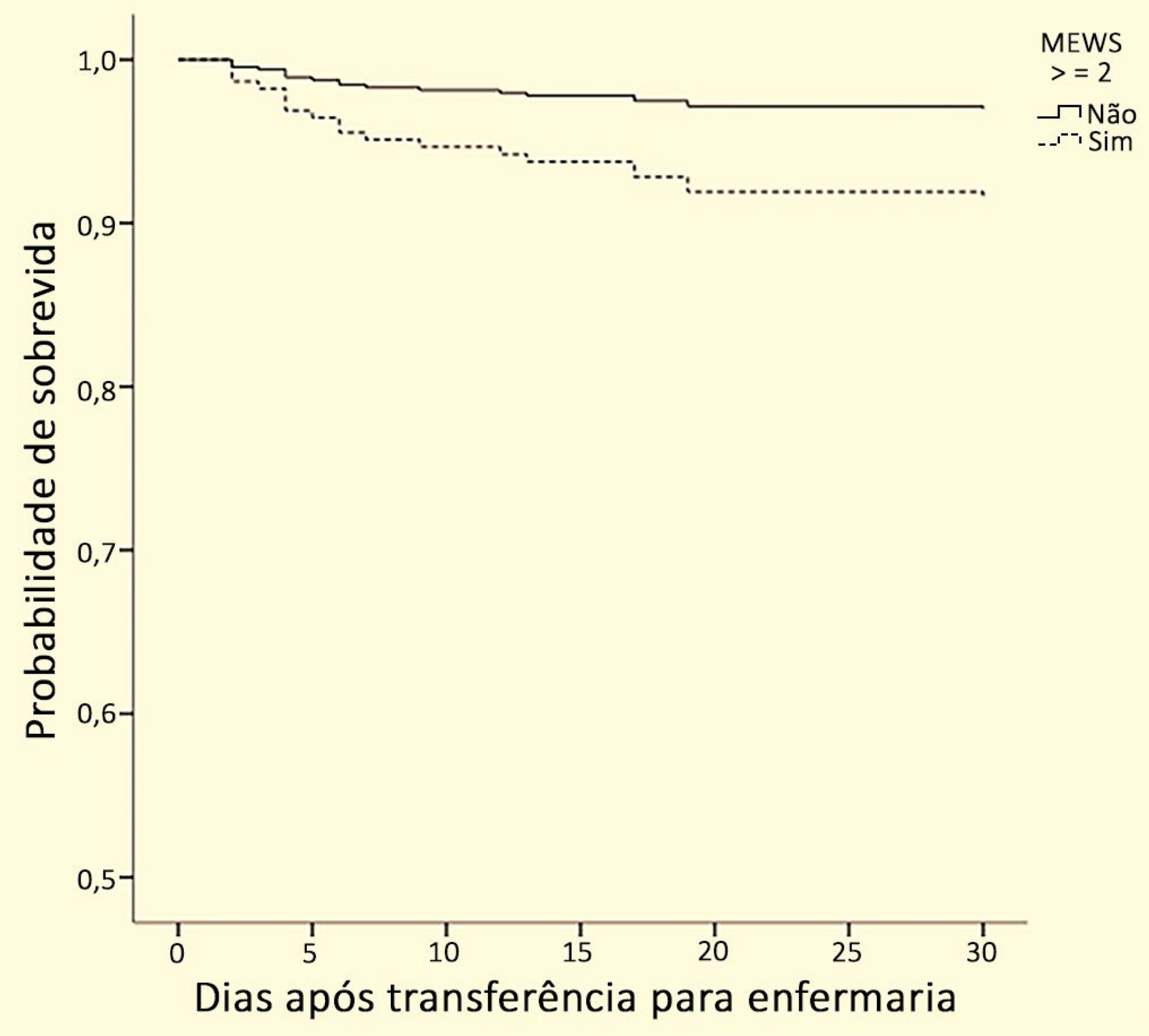
To verify whether there is an association between the Modified Early Warning Score before the transfer from the emergency room to the ward and death or admission to the intensive care unit within 30 days.
This is a historical cohort study conducted in a high-complexity hospital in southern Brazil with patients who were transferred from the emergency room to the ward between January and June 2017. The following data were collected: sociodemographic variables; comorbidities, as determined by the Charlson index; reason for hospitalization; Modified Early Warning Score at the time of transfer; admission to the intensive care unit; care by the Rapid Response Team; mortality within 30 days; and hospital mortality.
A total of 278 patients were included in the study. Regarding the Modified Early Warning Score, patients who died within 30 days had a significantly higher score than surviving patients during this period (2.0 [1.0 - 3.0] versus 1.0 [1.0 - 2.0], respectively; p = 0.006). The areas under the receiver operating characteristic curve for death within 30 days and for ICU admission were 0.67 (0.55 - 0.80; p = 0.012) and 0.72 (0.59 - 0.84; p = 0.02), respectively, with a Modified Early Warning Score cutoff of ≥ 2. In the Cox regression, the Modified Early Warning Score was independently associated with mortality within 30 days after multivariate adjustment (hazard ratio 2.91; 95% confidence interval 1.04 - 8.13).
The Modified Early Warning Score before intrahospital transfer from the emergency room to the ward is associated with admission to the intensive care unit and death within 30 days. The Modified Early Warning Score can be an important indicator for monitoring these patients and can prompt the receiving team to take specific actions.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):15-20
DOI 10.5935/0103-507X.20190003
To describe the incidence of clinical and non-clinical events during intrahospital transport of critically ill patients and to analyze the associated risk factors.
Cohort study with retrospective data collected from October 2016 to October 2017. All cases of intrahospital transport for diagnostic and therapeutic purposes in a large hospital with six adult intensive care units were analyzed, and the adverse events and related risk factors were evaluated.
During the study period, 1,559 intrahospital transports were performed with 1,348 patients, with a mean age of 66 ± 17 years and a mean transport time of 43 ± 34 minutes. During transport, 19.8% of the patients were using vasoactive drugs; 13.7% were under sedation; and 10.6% were under mechanical ventilation. Clinical events occurred in 117 transports (7.5%), and non-clinical events occurred in 125 (8.0%) transports. Communication failures were prevalent; however, the multivariate analysis showed that the use of sedatives, noradrenaline and nitroprusside and a transport time greater than 36.5 minutes were associated with adverse clinical events. The use of dobutamine and a transport time greater than 36.5 minutes were associated with non-clinical events. At the end of transport, 98.1% of the patients presented unchanged clinical conditions compared with baseline.
Intrahospital transport is related to a high incidence of adverse events, and transport time and the use of sedatives and vasoactive drugs were related to these events.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):162-166
DOI 10.1590/S0103-507X2012000200011
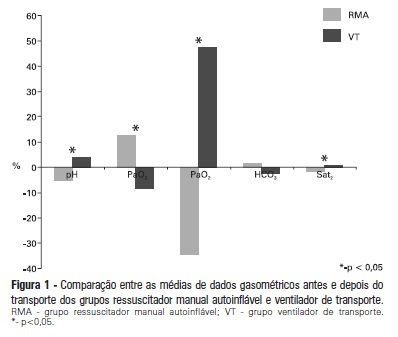
OBJECTIVE: To evaluate the effects on blood gases by two methods of ventilation (with transport ventilation or self-inflating manual resuscitator) during intra-hospital transport of patients after cardiac surgery. METHODS: Observational, longitudinal, prospective, randomized study. Two samples of arterial blood were collected at the end of the surgery and another at the end of patient transport. RESULTS: We included 23 patients: 13 in the Group with transport ventilation and 10 in the Group with self-inflating manual resuscitator. Baseline characteristics were similar between both groups, except for higher acute severity of illness in the Group with transport ventilation. We observed significant differences in comparisons of percentage variations of gasometric data: pH (transport ventilation + 4% x MR -5%, p=0.007), PaCO2 (-8% x +13%, p=0.006), PaO2 (+47% x -34%, p=0.01) and SatO2 (+0.6% x -1.7%, p=0.001). CONCLUSION: The use of mechanical ventilation results in fewer repercussions for blood gas analysis in the intra-hospital transport of cardiac surgery patients.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)