Abstract
Rev Bras Ter Intensiva. 2022;34(2):220-226
DOI 10.5935/0103-507X.20220019-en
To compare the predictive performance of residents, senior intensive care unit physicians and surrogates early during intensive care unit stays and to evaluate whether different presentations of prognostic data (probability of survival versus probability of death) influenced their performance.
We questioned surrogates and physicians in charge of critically ill patients during the first 48 hours of intensive care unit admission on the patient’s probability of hospital outcome. The question framing (i.e., probability of survival versus probability of death during hospitalization) was randomized. To evaluate the predictive performance, we compared the areas under the ROC curves (AUCs) for hospital outcome between surrogates and physicians’ categories. We also stratified the results according to randomized question framing.
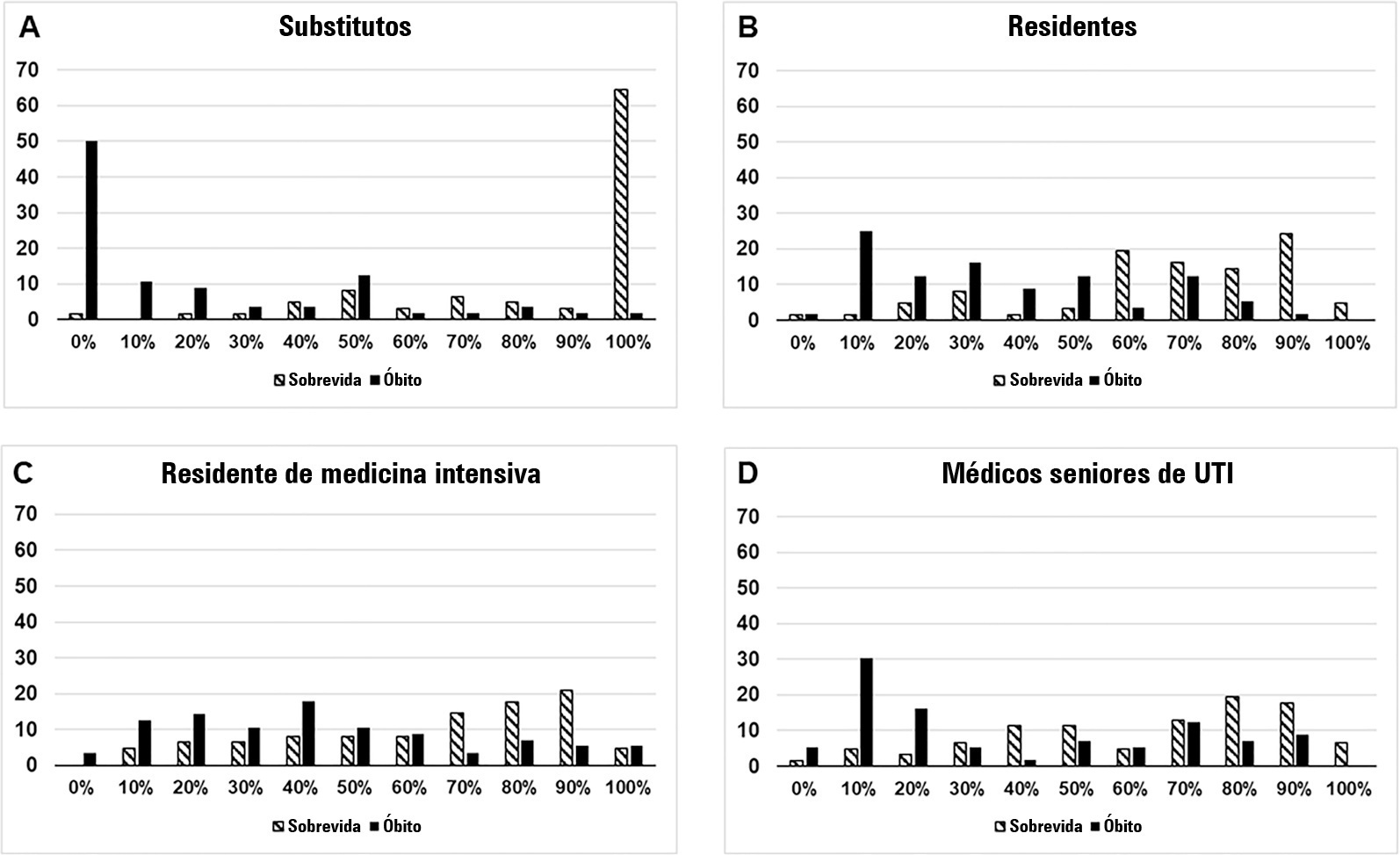
We interviewed surrogates and physicians on the hospital outcomes of 118 patients. The predictive performance of surrogate decisionmakers was significantly lower than that of physicians (AUC of 0.63 for surrogates, 0.82 for residents, 0.80 for intensive care unit fellows and 0.81 for intensive care unit senior physicians). There was no increase in predictive performance related to physicians’ experience (i.e., senior physicians did not predict outcomes better than junior physicians). Surrogate decisionmakers worsened their prediction performance when they were asked about probability of death instead of probability of survival, but there was no difference for physicians.
Different predictive performance was observed when comparing surrogate decision-makers and physicians, with no effect of experience on health care professionals’ prediction. Question framing affected the predictive performance of surrogates but not of physicians.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):219-230
DOI 10.5935/0103-507X.20210029
To assess the impact of intensive care unit bed availability, distractors and choice framing on intensive care unit admission decisions.
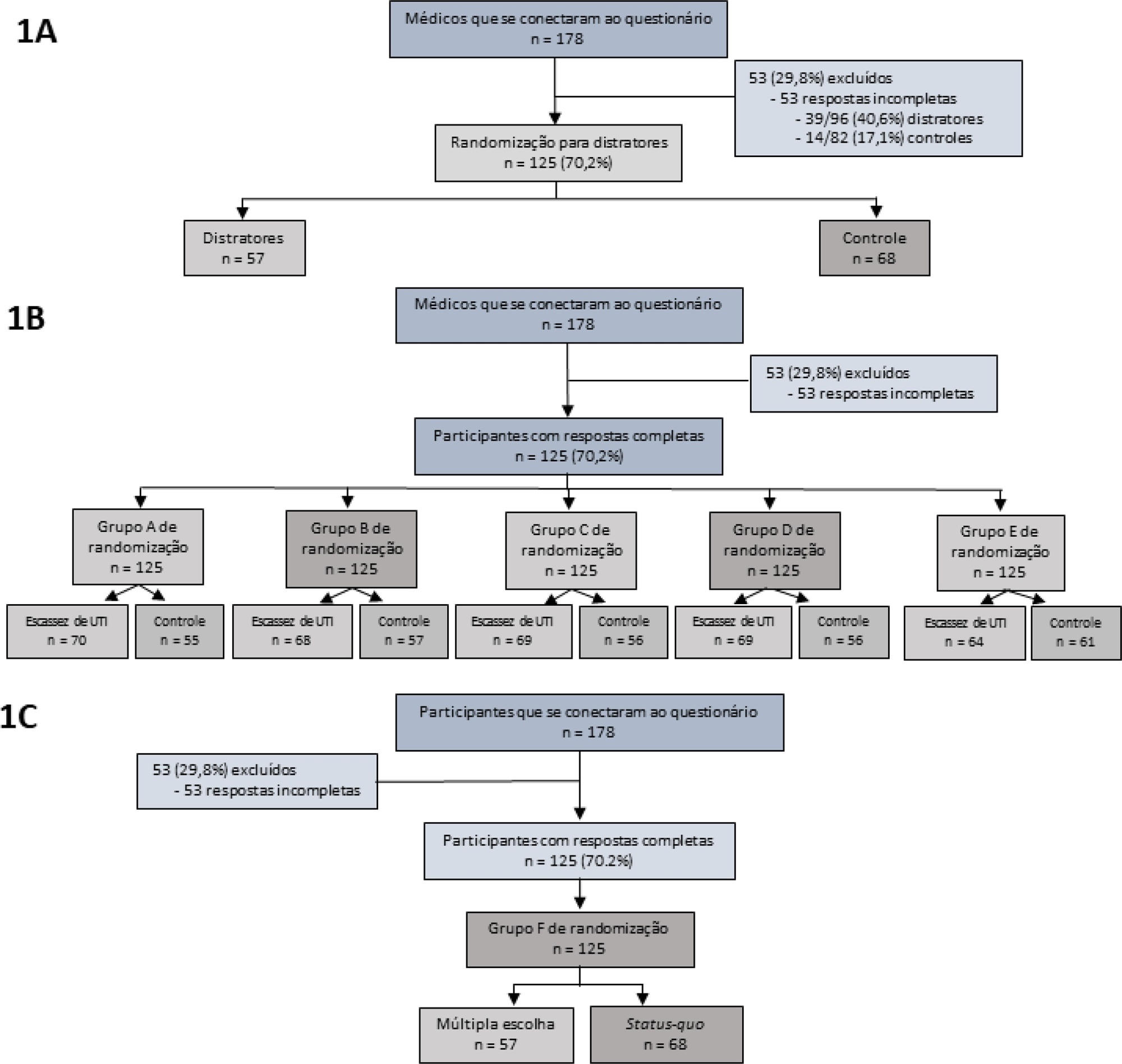
This study was a randomized factorial trial using patient-based vignettes. The vignettes were deemed archetypical for intensive care unit admission or refusal, as judged by a group of experts. Intensive care unit physicians were randomized to 1) an increased distraction (intervention) or a control group, 2) an intensive care unit bed scarcity or nonscarcity (availability) setting, and 3) a multiple-choice or omission (status quo) vignette scenario. The primary outcome was the proportion of appropriate intensive care unit allocations, defined as concordance with the allocation decision made by the group of experts.
We analyzed 125 physicians. Overall, distractors had no impact on the outcome; however, there was a differential drop-out rate, with fewer physicians in the intervention arm completing the questionnaire. Intensive care unit bed availability was associated with an inappropriate allocation of vignettes deemed inappropriate for intensive care unit admission (OR = 2.47; 95%CI 1.19 - 5.11) but not of vignettes appropriate for intensive care unit admission. There was a significant interaction with the presence of distractors (p = 0.007), with intensive care unit bed availability being associated with increased intensive care unit admission of vignettes inappropriate for intensive care unit admission in the distractor (intervention) arm (OR = 9.82; 95%CI 2.68 - 25.93) but not in the control group (OR = 1.02; 95%CI 0.38 - 2.72). Multiple choices were associated with increased inappropriate allocation in comparison to the omission group (OR = 5.18; 95%CI 1.37 - 19.61).
Intensive care unit bed availability and cognitive biases were associated with inappropriate intensive care unit allocation decisions. These findings may have implications for intensive care unit admission policies.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):154-162
DOI 10.5935/0103-507X.20170025
To evaluate the factors potentially associated with the decision of admission to the intensive care unit in Brazil.
An electronic survey of Brazilian physicians working in intensive care units. Fourteen variables that were potentially associated with the decision of admission to the intensive care unit were rated as important (from 1 to 5) by the respondents and were later grouped as "patient-related," "scarcity-related" and "administrative-related" factors. The workplace and physician characteristics were evaluated for correlation with the factor ratings.
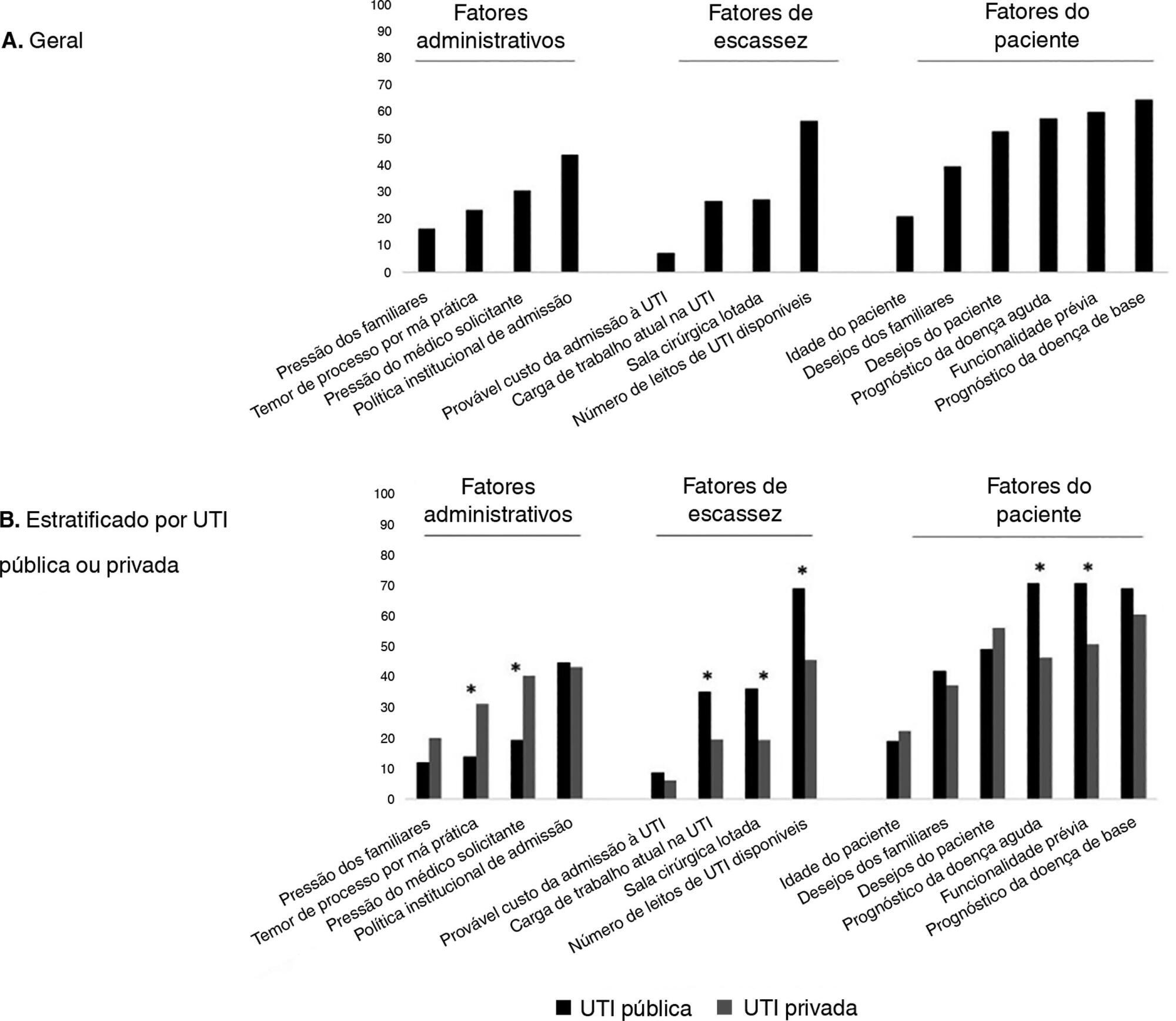
During the study period, 125 physicians completed the survey. The scores on patient-related factors were rated higher on their potential to affect decisions than scarcity-related or administrative-related factors, with a mean ± SD of 3.42 ± 0.7, 2.75 ± 0.7 and 2.87 ± 0.7, respectively (p < 0.001). The patient's underlying illness prognosis was rated by 64.5% of the physicians as always or frequently affecting decisions, followed by acute illness prognosis (57%), number of intensive care unit beds available (56%) and patient's wishes (53%). After controlling for confounders, receiving specific training on intensive care unit triage was associated with higher ratings of the patient-related factors and scarcity-related factors, while working in a public intensive care unit (as opposed to a private intensive care unit) was associated with higher ratings of the scarcity-related factors.
Patient-related factors were more frequently rated as potentially affecting intensive care unit admission decisions than scarcity-related or administrative-related factors. Physician and workplace characteristics were associated with different factor ratings.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):335-340
DOI 10.5935/0103-507X.20160057
To evaluate the perceptions of physicians, nurses and nursing technicians of their participation in the decision-making process surrounding life support limitation in terminally ill pediatric patients, with comparisons by professional category.
A cross-sectional study was conducted in the pediatric intensive care unit of a tertiary public university hospital with the participation of physicians, nurses and nursing technicians. The MacArthur Admission Experience Survey Voice Scale was used to assess and quantify the perceptions of professionals who assisted 17 pediatric patients with life support limitation within 24 hours after the outcome of each patient was determined. All professionals working in the unit (n = 117) who were potentially eligible for the study received a free and informed consent form prior to the occurrence of the cases studied.
Study participants included 25/40 (62.5%) physicians, 10/17 (58.8%) nurses and 41/60 (68.3%) nursing technicians, representing 65% of the eligible professionals identified. The questionnaire return rate was higher for physicians than technicians (p = 0.0258). A perceived lack of voice was reported in all three professional categories at varying rates that were lower for physicians than for nurses and nursing technicians (p < 0.00001); there was no difference between the latter (p = 0.7016). In the three professional categories studied, three subscale items were reported. For two of the three statements, there were significant differences between physicians and nurses (p = 0.004) and between physicians and nursing technicians (p = 0.001). For one of the statements, there was no difference among the three professional categories.
Respondents perceived a lack of voice in the decision-making process at varying rates across the three categories of studied professionals who assisted terminally ill pediatric patients with life support limitation, with physicians expressing lowered rates of perceived coercion.
Abstract
Rev Bras Ter Intensiva. 2011;23(1):78-86
DOI 10.1590/S0103-507X2011000100013
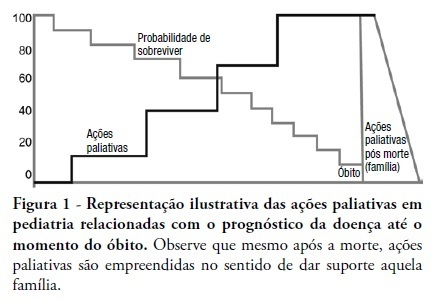
This review discusses the main dilemmas and difficulties related to end-of-life decision's in children with terminal and irreversible diseases and propose a rational sequence for delivering palliative care to this patients' group. The Medline and Lilacs databases were searched using the terms 'end of life', 'palliative care', 'death' and 'terminal disease' for articles published in recent years. The most relevant articles and those enrolling pediatric patients were selected and compared to previous authors' studies in this field. The current Brazilian Medical Ethics Code (2010) was analyzed regarding end-oflife practices and palliative care for terminal patients. Lack of knowledge, insufficient specific training, and legal concerns are the main reasons why end-of-life decisions in terminal children are based on medical opinion with scarce family participation. The current Brazilian Medical Ethics Code (2010) fully supports end-of-life decisions made consensually with active family participation. Honest dialogue with the family regarding diagnostic, prognostic, therapeutic and palliative care measures should be established gradually to identify the best strategy to meet the child's end-of-life needs. Treatment focused on the child's welfare combined with the family's participation is the basis for successful palliative care of children with terminal diseases.
Abstract
Rev Bras Ter Intensiva. 2006;18(2):137-142
DOI 10.1590/S0103-507X2006000200006
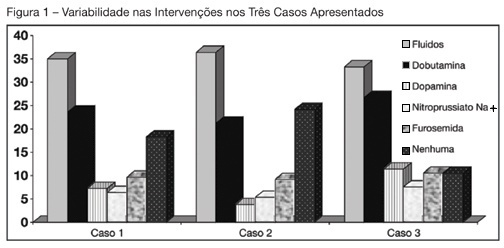
BACKGROUND AND OBJECTIVES: Use of Pulmonary Artery Catheter (PAC) is still a debatable issue, mainly due to questions raised about its security and efficacy. This study reproduced in a sample of Brazilian physicians, another one conducted amidst American doctors, in which was pointed out the heterogeneity of clinical decisions guided by data obtained from PAC. METHODS: During the Brazilian Congress of Intensive Care Medicine (Curitiba 2004), doctors were asked to answer a survey form with three vignettes. Each of them contained PAC data and one half of the surveys contained echocardiographic information. Every doctor was asked to select one of six interventions for each vignette. A homogeneous answer was considered when it was selected by at least 80% of the respondents. RESULTS: Two hundred and thirty seven doctors answered the questionnaires. They selected completely different therapeutic interventions in all three vignettes and none of the interventions achieved more than 80% agreement. Variability persisted with the choices guided by echocardiography. CONCLUSIONS: As in the original study, we observed total heterogeneity of therapeutic interventions guided by CAP and echocardiography. These results could be caused by lack of knowledge about basic pathophysiologic concepts and maybe we had to improve its teaching at the medical school benches.
Abstract
Rev Bras Ter Intensiva. 2007;19(3):364-368
DOI 10.1590/S0103-507X2007000300018
BACKGROUND AND OBJECTIVES: To analyze and discuss the medical aspects related to the family involvement in the decision making process regarding end of life care to children admitted to the pediatric intensive care unit (PICU). CONTENTS: The authors selected articles on end-of-life care published during the last years searching the PubMed, MedLine and LILACS database, with special interest on studies of death conducted in pediatric intensive care units in Brazil, Latin America, Europe and North America, using the following keywords: death, bioethics, PICU, decision-making, terminal care, parents interview and life support limitation (LSL). CONCLUSIONS: Several studies have demonstrated the relevance of the family participation in the decision making process regarding LSL. In our region the family participation in this process is not stimulated and valued, ranging from 20%-55%. The authors present a practical sequence for discussing and defining LSL with the families. Despite of the family participation in the decision making process for LSL be legally, morally and ethically accepted in developed countries, this approach is adopted in a very few cases in our region. To explain this difficulty observed among the Brazilian pediatric intensivist, some studies should be conducted in our region.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)