You searched for:"Daniel Neves Forte"
We found (7) results for your search.-
Original Article
Exploring the association of two oxygenators in parallel or in series during respiratory support using extracorporeal membrane oxygenation
Rev Bras Ter Intensiva. 2022;34(4):402-409
Abstract
Original ArticleExploring the association of two oxygenators in parallel or in series during respiratory support using extracorporeal membrane oxygenation
Rev Bras Ter Intensiva. 2022;34(4):402-409
DOI 10.5935/0103-507X.20220299-en
Views3ABSTRACT
Objective:
To characterize the pressures, resistances, oxygenation, and decarboxylation efficacy of two oxygenators associated in series or in parallel during venous-venous extracorporeal membrane oxygenation support.
Methods:
Using the results of a swine severe respiratory failure associated with multiple organ dysfunction venous-venous extracorporeal membrane oxygenation support model and mathematical modeling, we explored the effects on oxygenation, decarboxylation and circuit pressures of in-parallel and in-series associations of oxygenators.
Results:
Five animals with a median weight of 80kg were tested. Both configurations increased the oxygen partial pressure after the oxygenators. The return cannula oxygen content was also slightly higher, but the impact on systemic oxygenation was minimal using oxygenators with a high rated flow (~ 7L/minute). Both configurations significantly reduced the systemic carbon dioxide partial pressure. As the extracorporeal membrane oxygenation blood flow increased, the oxygenator resistance decreased initially with a further increase with higher blood flows but with a small clinical impact.
Conclusion:
Association of oxygenators in parallel or in series during venous-venous extracorporeal membrane oxygenation support provides a modest increase in carbon dioxide partial pressure removal with a slight improvement in oxygenation. The effect of oxygenator associations on extracorporeal circuit pressures is minimal.
Keywords:acute respiratory distress syndromeDecarboxylationExtracorporeal membrane oxygenationHypercapniaHypoxiaOxygenatorsSwineSee more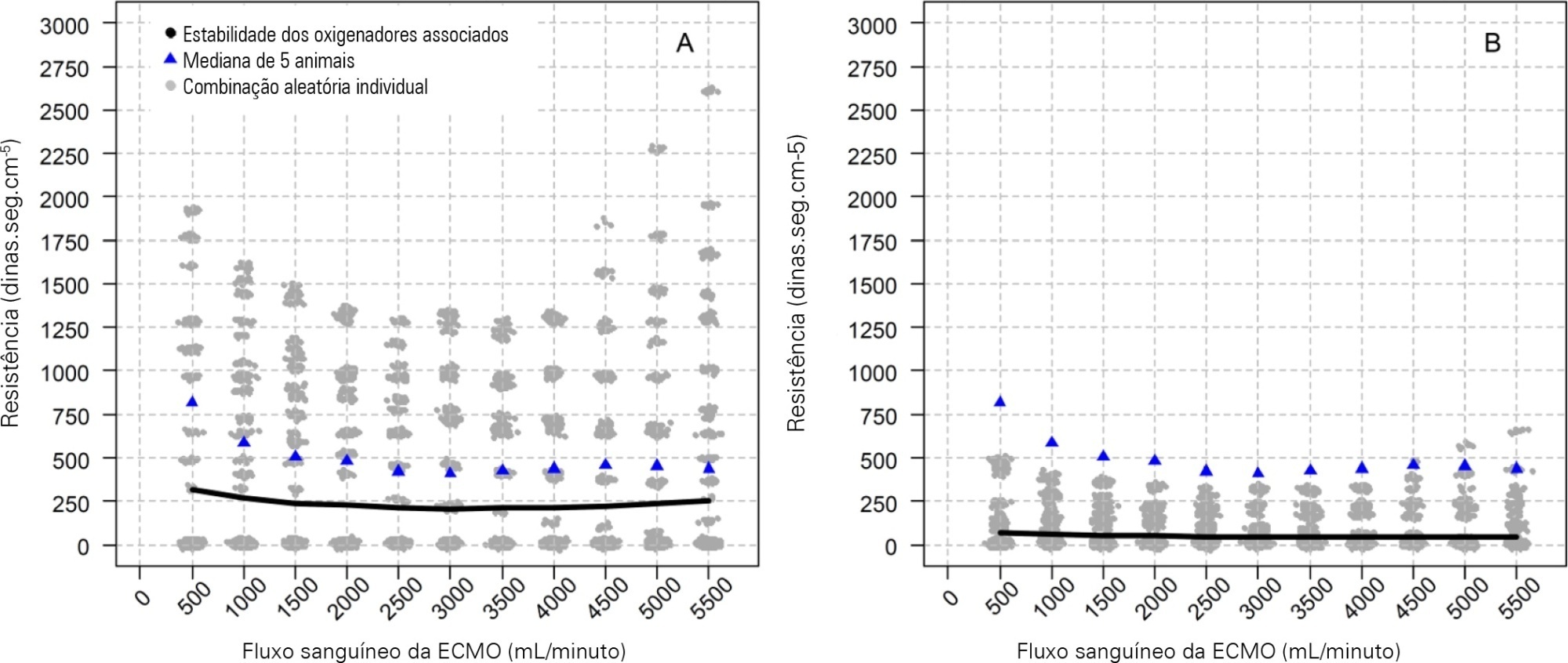
-
Original Article
Impact of nonclinical factors on intensive care unit admission decisions: a vignette-based randomized trial (V-TRIAGE)
Rev Bras Ter Intensiva. 2021;33(2):219-230
Abstract
Original ArticleImpact of nonclinical factors on intensive care unit admission decisions: a vignette-based randomized trial (V-TRIAGE)
Rev Bras Ter Intensiva. 2021;33(2):219-230
DOI 10.5935/0103-507X.20210029
Views1See moreAbstract
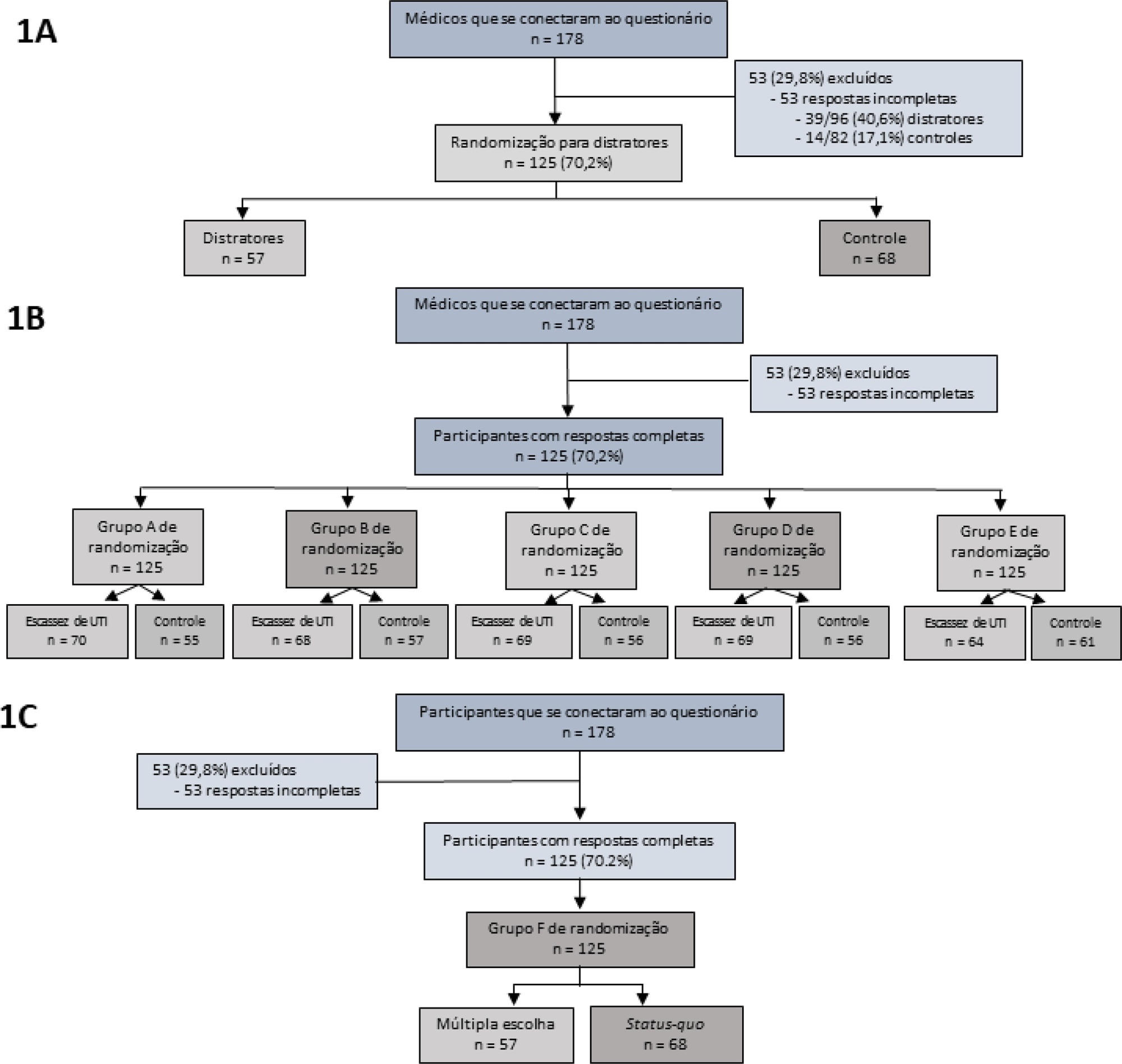
Objective:
To assess the impact of intensive care unit bed availability, distractors and choice framing on intensive care unit admission decisions.
Methods:
This study was a randomized factorial trial using patient-based vignettes. The vignettes were deemed archetypical for intensive care unit admission or refusal, as judged by a group of experts. Intensive care unit physicians were randomized to 1) an increased distraction (intervention) or a control group, 2) an intensive care unit bed scarcity or nonscarcity (availability) setting, and 3) a multiple-choice or omission (status quo) vignette scenario. The primary outcome was the proportion of appropriate intensive care unit allocations, defined as concordance with the allocation decision made by the group of experts.
Results:
We analyzed 125 physicians. Overall, distractors had no impact on the outcome; however, there was a differential drop-out rate, with fewer physicians in the intervention arm completing the questionnaire. Intensive care unit bed availability was associated with an inappropriate allocation of vignettes deemed inappropriate for intensive care unit admission (OR = 2.47; 95%CI 1.19 – 5.11) but not of vignettes appropriate for intensive care unit admission. There was a significant interaction with the presence of distractors (p = 0.007), with intensive care unit bed availability being associated with increased intensive care unit admission of vignettes inappropriate for intensive care unit admission in the distractor (intervention) arm (OR = 9.82; 95%CI 2.68 – 25.93) but not in the control group (OR = 1.02; 95%CI 0.38 – 2.72). Multiple choices were associated with increased inappropriate allocation in comparison to the omission group (OR = 5.18; 95%CI 1.37 – 19.61).
Conclusion:
Intensive care unit bed availability and cognitive biases were associated with inappropriate intensive care unit allocation decisions. These findings may have implications for intensive care unit admission policies.
-
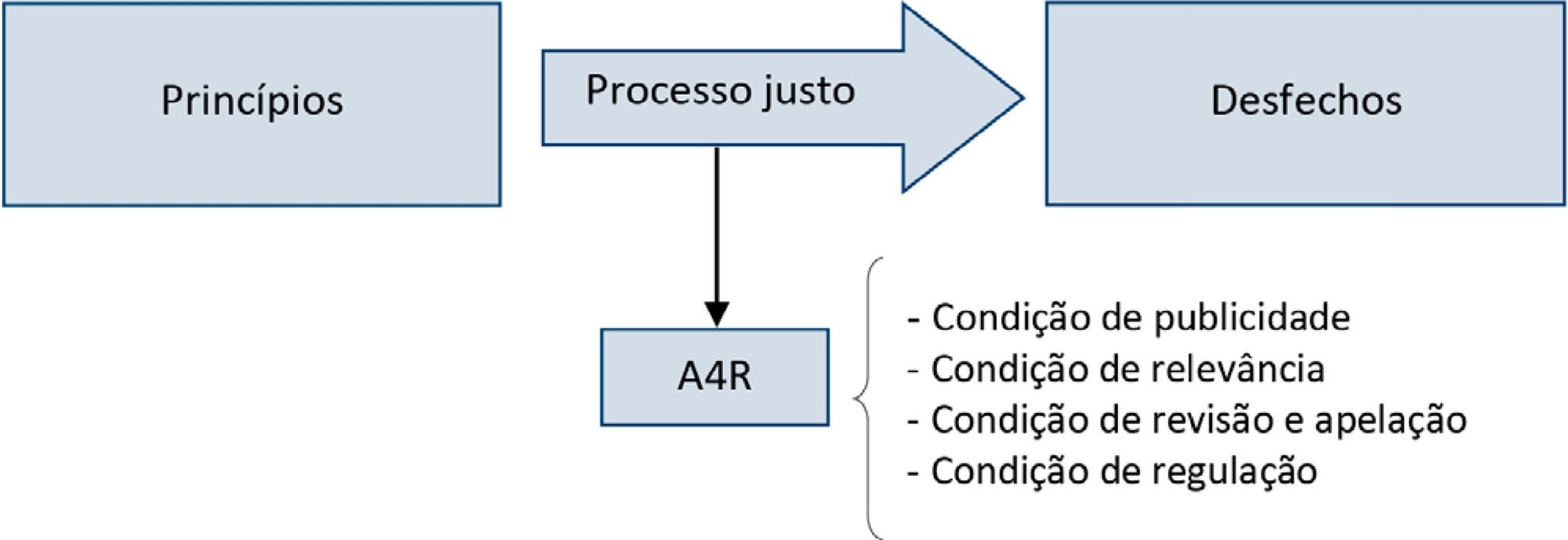
Special Article
Accountability for reasonableness and criteria for admission, triage and discharge in intensive care units: an analysis of current ethical recommendations
Rev Bras Ter Intensiva. 2021;33(1):38-47
Abstract
Special ArticleAccountability for reasonableness and criteria for admission, triage and discharge in intensive care units: an analysis of current ethical recommendations
Rev Bras Ter Intensiva. 2021;33(1):38-47
DOI 10.5935/0103-507X.20210004
Views0See moreAbstract
Triage for intensive care unit admission is a frequent event and is associated to worse clinical outcomes. The process of triage is variable and may be influenced by biases and prejudices, which could lead to potentially unfair decisions. The Brazilian Federal Council of Medicine (Conselho Federal de Medicina) has recently released a guideline for intensive care unit admission and discharge. The aim of this paper is to evaluate the ethical dilemmas related to the implementation of this guideline, through the accountability for reasonabless approach, known as A4R, as elaborated by Norman Daniels. We conclude that the guideline contemplates A4R conditions, but we observe that there is a need for indication of A4R-concordant criteria to operationalize the guidelines.
-
Original Article
Mechanical ventilation withdrawal as a palliative procedure in a Brazilian intensive care unit
Rev Bras Ter Intensiva. 2020;32(4):528-534
Abstract
Original ArticleMechanical ventilation withdrawal as a palliative procedure in a Brazilian intensive care unit
Rev Bras Ter Intensiva. 2020;32(4):528-534
DOI 10.5935/0103-507X.20200090
Views1See moreAbstract
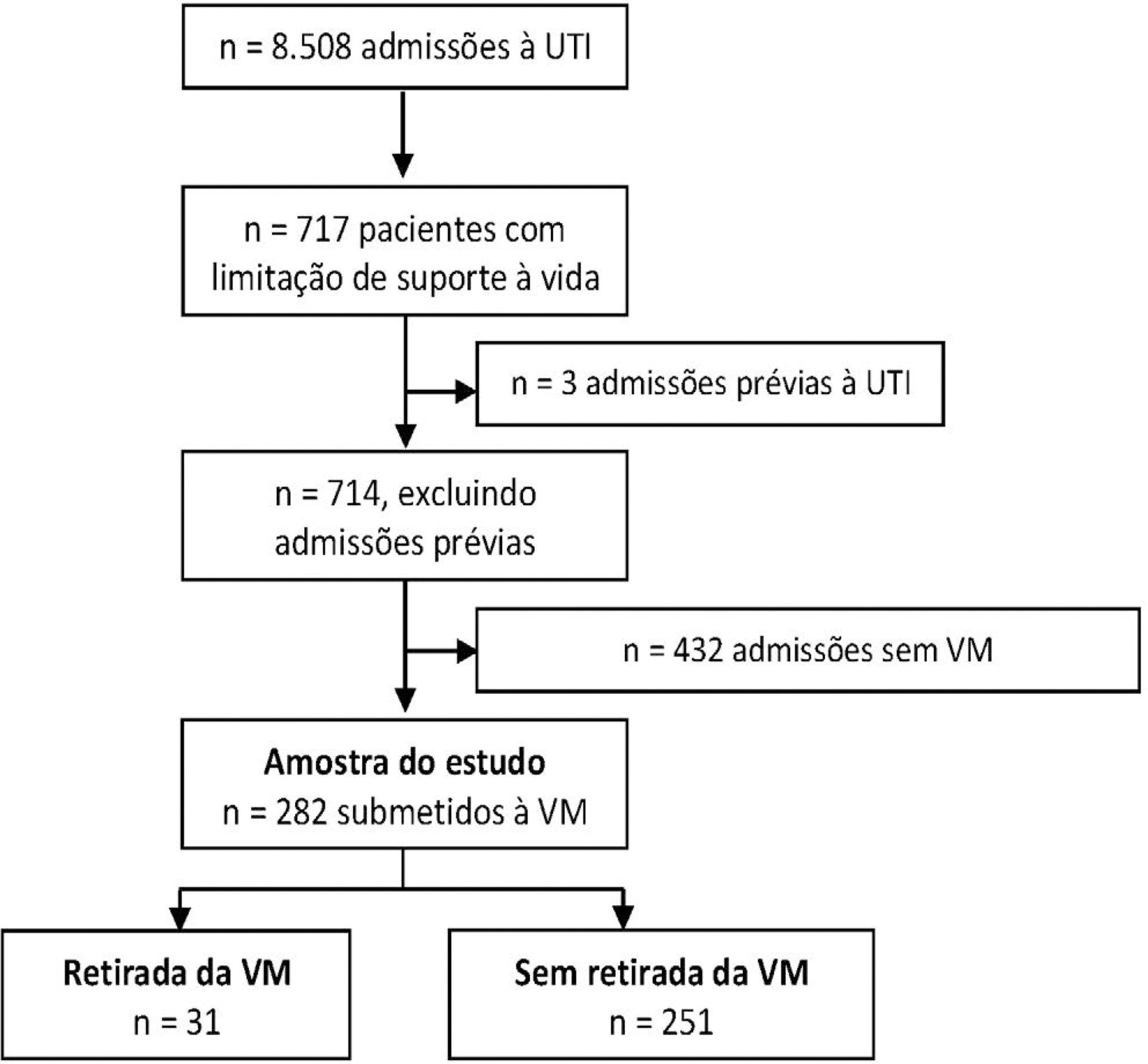
Objective:
To describe the characteristics and outcomes of patients undergoing mechanical ventilation withdrawal and to compare them to mechanically ventilated patients with limitations (withhold or withdrawal) of life-sustaining therapies but who did not undergo mechanical ventilation withdrawal.
Methods:
This was a retrospective cohort study from January 2014 to December 2018 of mechanically ventilated patients with any organ support limitation admitted to a single intensive care unit. We compared patients who underwent mechanical ventilation withdrawal and those who did not regarding intensive care unit and hospital mortality and length of stay in both an unadjusted analysis and a propensity score matched subsample. We also analyzed the time from mechanical ventilation withdrawal to death.
Results:
Out of 282 patients with life-sustaining therapy limitations, 31 (11%) underwent mechanical ventilation withdrawal. There was no baseline difference between groups. Intensive care unit and hospital mortality rates were 71% versus 57% and 93% versus 80%, respectively, among patients who underwent mechanical ventilation withdrawal and those who did not. The median intensive care unit length of stay was 7 versus 8 days (p = 0.6), and the hospital length of stay was 9 versus 15 days (p = 0.015). Hospital mortality was not significantly different (25/31; 81% versus 29/31; 93%; p = 0.26) after matching. The median time from mechanical ventilation withdrawal until death was 2 days [0 – 5], and 10/31 (32%) patients died within 24 hours after mechanical ventilation withdrawal.
Conclusion:
In this Brazilian report, mechanical ventilation withdrawal represented 11% of all patients with treatment limitations and was not associated with increased hospital mortality after propensity score matching on relevant covariates.
-
Original Articles
Factors potentially associated with the decision of admission to the intensive care unit in a middle-income country: a survey of Brazilian physicians
Rev Bras Ter Intensiva. 2017;29(2):154-162
Abstract
Original ArticlesFactors potentially associated with the decision of admission to the intensive care unit in a middle-income country: a survey of Brazilian physicians
Rev Bras Ter Intensiva. 2017;29(2):154-162
DOI 10.5935/0103-507X.20170025
Views0See moreABSTRACT
Objective:
To evaluate the factors potentially associated with the decision of admission to the intensive care unit in Brazil.
Methods:
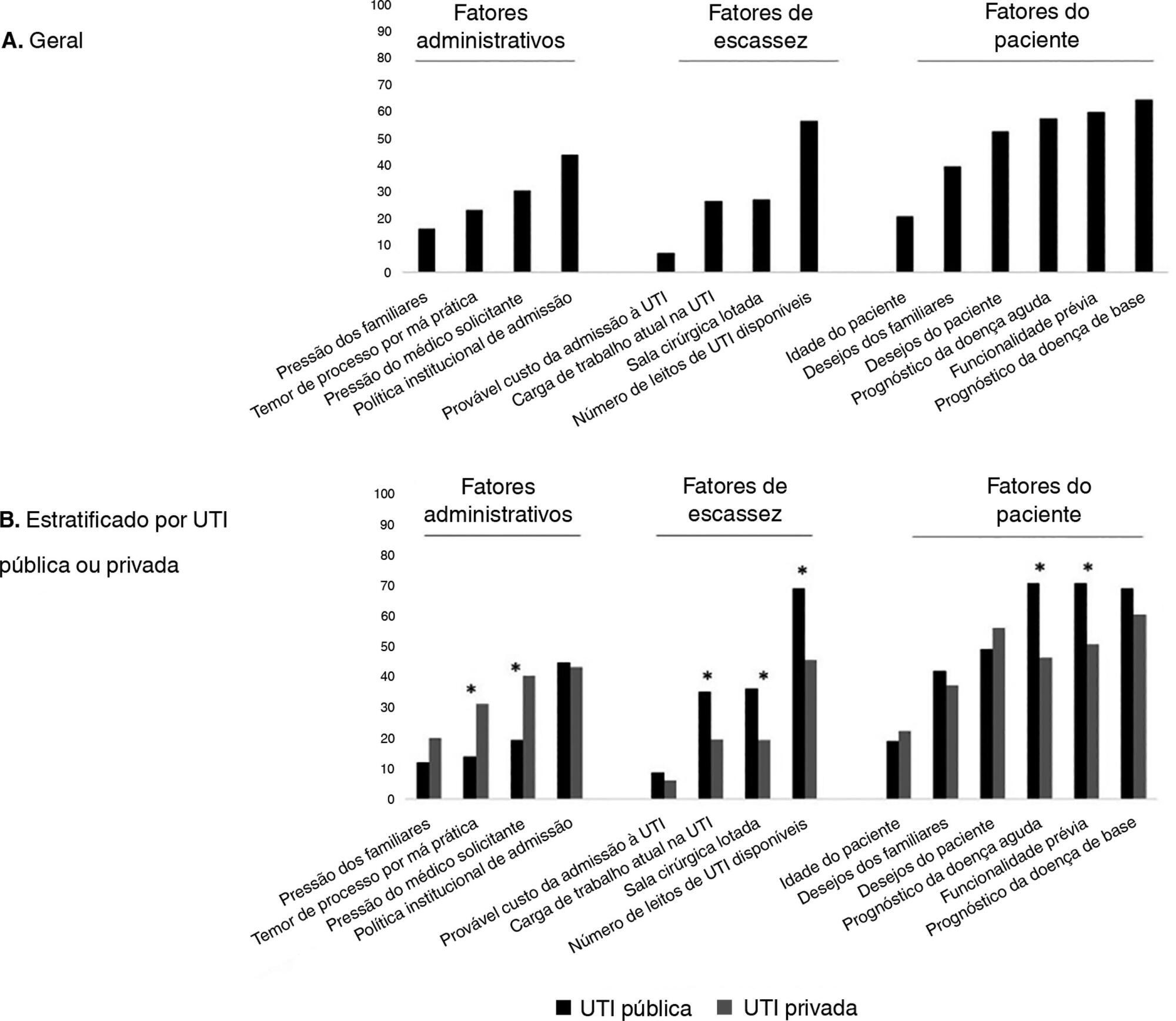
An electronic survey of Brazilian physicians working in intensive care units. Fourteen variables that were potentially associated with the decision of admission to the intensive care unit were rated as important (from 1 to 5) by the respondents and were later grouped as “patient-related,” “scarcity-related” and “administrative-related” factors. The workplace and physician characteristics were evaluated for correlation with the factor ratings.
Results:
During the study period, 125 physicians completed the survey. The scores on patient-related factors were rated higher on their potential to affect decisions than scarcity-related or administrative-related factors, with a mean ± SD of 3.42 ± 0.7, 2.75 ± 0.7 and 2.87 ± 0.7, respectively (p < 0.001). The patient's underlying illness prognosis was rated by 64.5% of the physicians as always or frequently affecting decisions, followed by acute illness prognosis (57%), number of intensive care unit beds available (56%) and patient's wishes (53%). After controlling for confounders, receiving specific training on intensive care unit triage was associated with higher ratings of the patient-related factors and scarcity-related factors, while working in a public intensive care unit (as opposed to a private intensive care unit) was associated with higher ratings of the scarcity-related factors.
Conclusions:
Patient-related factors were more frequently rated as potentially affecting intensive care unit admission decisions than scarcity-related or administrative-related factors. Physician and workplace characteristics were associated with different factor ratings.
-
Original Articles
Palliative care for patients with HIV/AIDS admitted to intensive care units
Rev Bras Ter Intensiva. 2016;28(3):301-309
Abstract
Original ArticlesPalliative care for patients with HIV/AIDS admitted to intensive care units
Rev Bras Ter Intensiva. 2016;28(3):301-309
DOI 10.5935/0103-507X.20160054
Views0See moreABSTRACT
Objective:
To describe the characteristics of patients with HIV/AIDS and to compare the therapeutic interventions and end-of-life care before and after evaluation by the palliative care team.
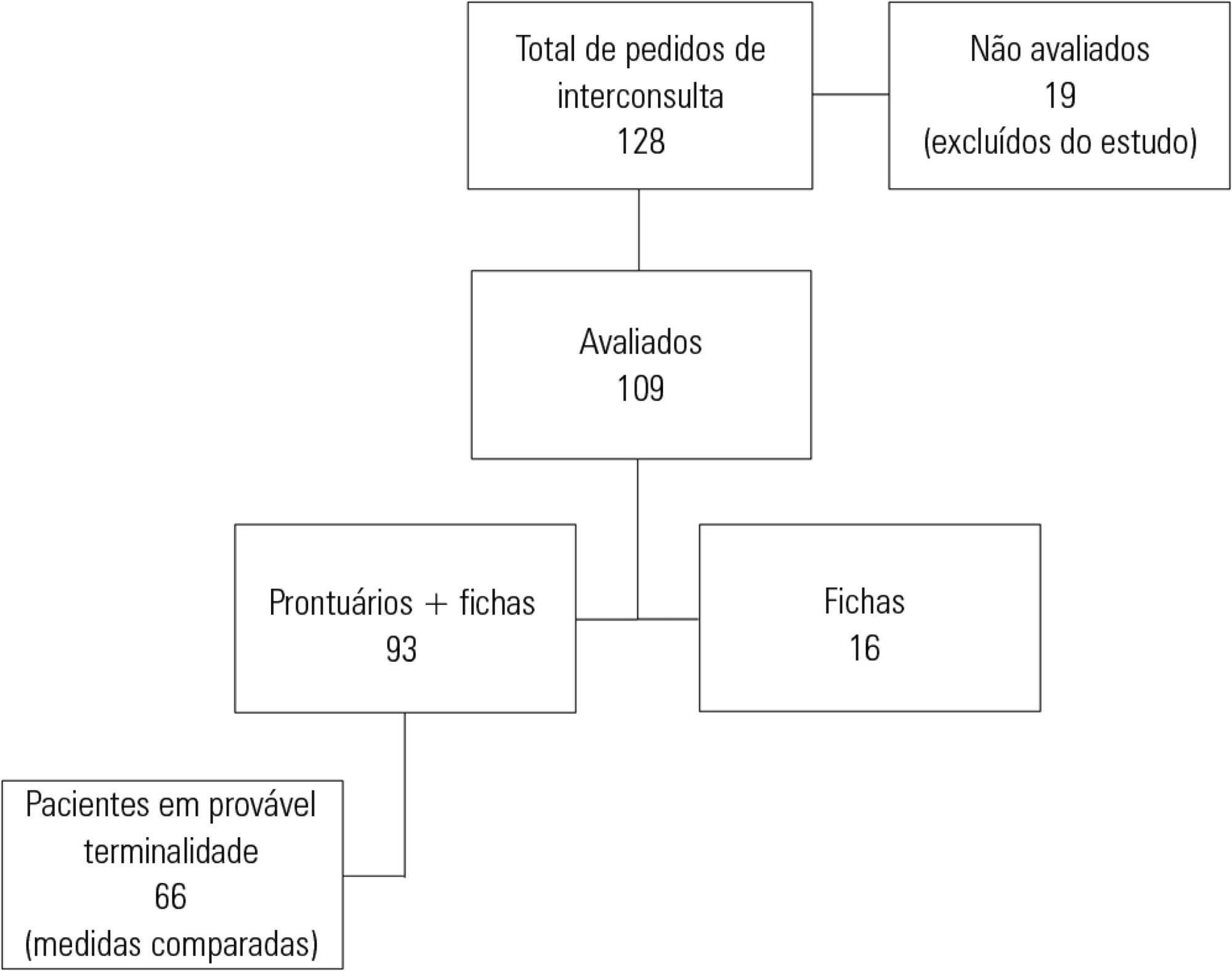
Methods:
This retrospective cohort study included all patients with HIV/AIDS admitted to the intensive care unit of the Instituto de Infectologia Emílio Ribas who were evaluated by a palliative care team between January 2006 and December 2012.
Results:
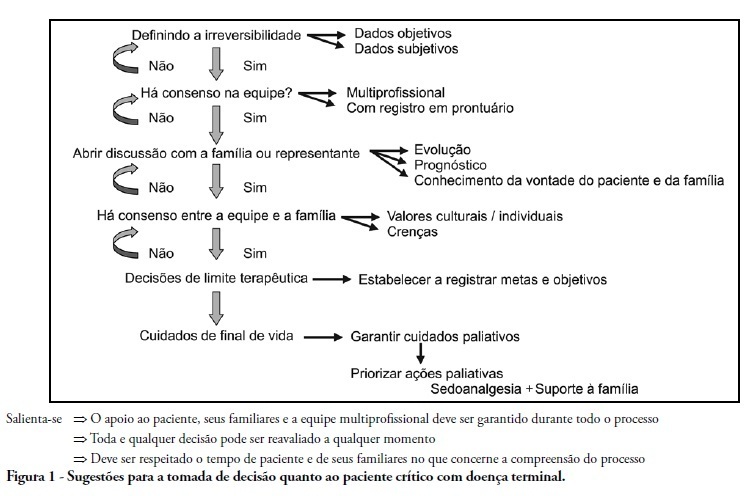
Of the 109 patients evaluated, 89% acquired opportunistic infections, 70% had CD4 counts lower than 100 cells/mm3, and only 19% adhered to treatment. The overall mortality rate was 88%. Among patients predicted with a terminally ill (68%), the use of highly active antiretroviral therapy decreased from 50.0% to 23.1% (p = 0.02), the use of antibiotics decreased from 100% to 63.6% (p < 0.001), the use of vasoactive drugs decreased from 62.1% to 37.8% (p = 0.009), the use of renal replacement therapy decreased from 34.8% to 23.0% (p < 0.0001), and the number of blood product transfusions decreased from 74.2% to 19.7% (p < 0.0001). Meetings with the family were held in 48 cases, and 23% of the terminally ill patients were discharged from the intensive care unit.
Conclusion:
Palliative care was required in patients with severe illnesses and high mortality. The number of potentially inappropriate interventions in terminally ill patients monitored by the palliative care team significantly decreased, and 26% of the patients were discharged from the intensive care unit.
-
II Forum of the “End of Life Study Group of the Southern Cone of America”: palliative care definitions, recommendations and integrated actions for intensive care and pediatric intensive care units
Rev Bras Ter Intensiva. 2011;23(1):24-29
Abstract
II Forum of the “End of Life Study Group of the Southern Cone of America”: palliative care definitions, recommendations and integrated actions for intensive care and pediatric intensive care units
Rev Bras Ter Intensiva. 2011;23(1):24-29
DOI 10.1590/S0103-507X2011000100005
Views0See morePalliative care is aimed to improve the quality of life of both patients and their family members during the course of life-threatening diseases through the prevention, early identification and treatment of the symptoms of physical, psychological, spiritual and social suffering. Palliative care should be provided to every critically ill patient; this requirement renders the training of intensive care practitioners and education initiatives fundamental. Continuing the Technical Council on End of Life and Palliative Care of the Brazilian Association of Intensive Medicine activities and considering previously established concepts, the II Forum of the End of Life Study Group of the Southern Cone of America was conducted in October 2010. The forum aimed to develop palliative care recommendations for critically ill patients.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




