You searched for:"João Gabriel Rosa Ramos"
We found (7) results for your search.-
Letter to the Editor
Endotracheal intubation in COVID-19 patients in Brazil: a nationwide survey
Rev Bras Ter Intensiva. 2022;34(1):202-204
Abstract
Letter to the EditorEndotracheal intubation in COVID-19 patients in Brazil: a nationwide survey
Rev Bras Ter Intensiva. 2022;34(1):202-204
DOI 10.5935/0103-507X.20220015-en
Views2To the Editor Endotracheal intubation is a life-saving procedure in acute respiratory distress syndrome. However, complications such as hypoxia, hypotension and cardiovascular collapse may occur in almost 40% of the procedures in the intensive care unit (ICU).() Evidence regarding the best practice of endotracheal intubation in this context is scarce, and most data have been […]See more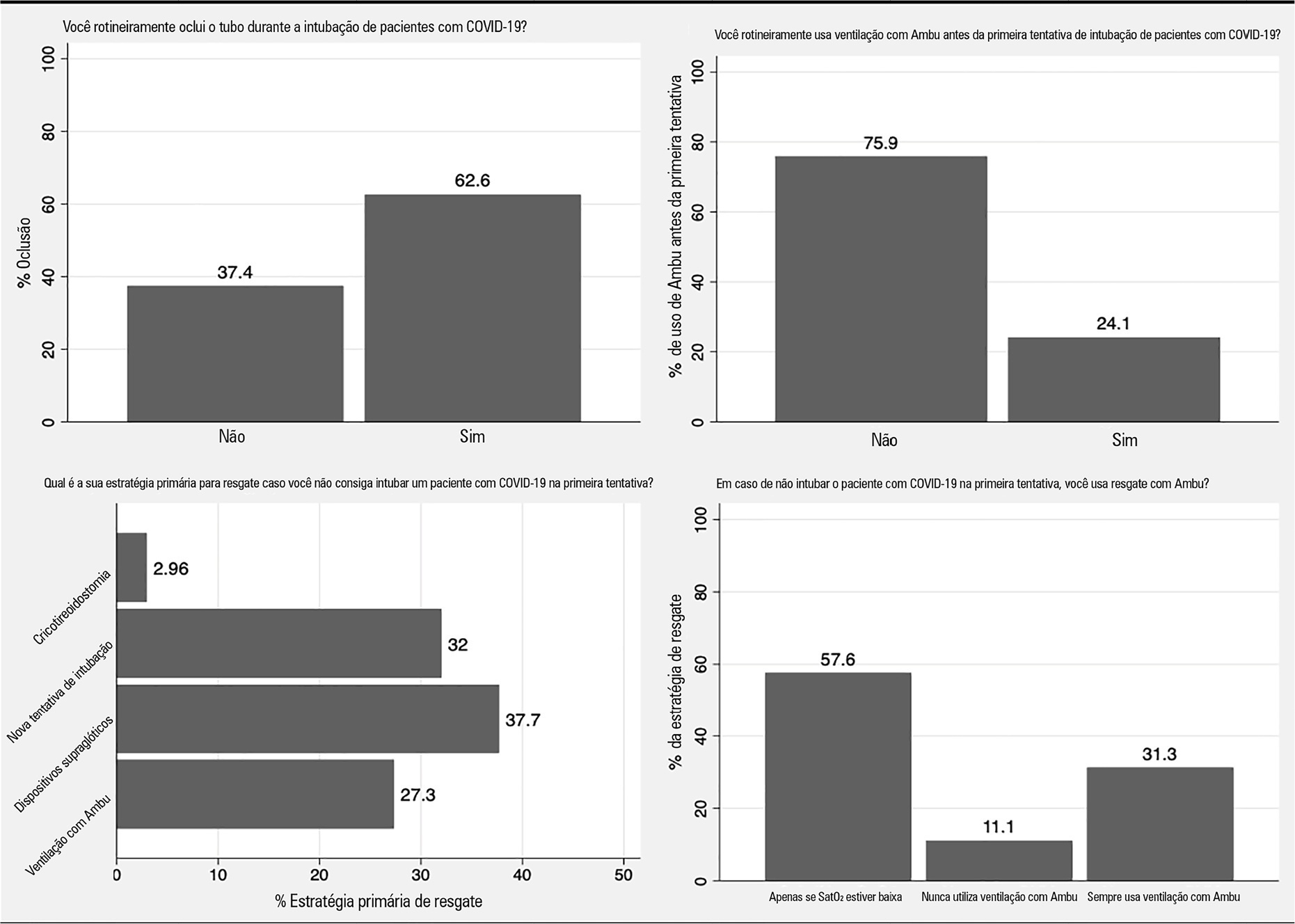
-
Original Article
Impact of nonclinical factors on intensive care unit admission decisions: a vignette-based randomized trial (V-TRIAGE)
Rev Bras Ter Intensiva. 2021;33(2):219-230
Abstract
Original ArticleImpact of nonclinical factors on intensive care unit admission decisions: a vignette-based randomized trial (V-TRIAGE)
Rev Bras Ter Intensiva. 2021;33(2):219-230
DOI 10.5935/0103-507X.20210029
Views1See moreAbstract
Objective:
To assess the impact of intensive care unit bed availability, distractors and choice framing on intensive care unit admission decisions.
Methods:
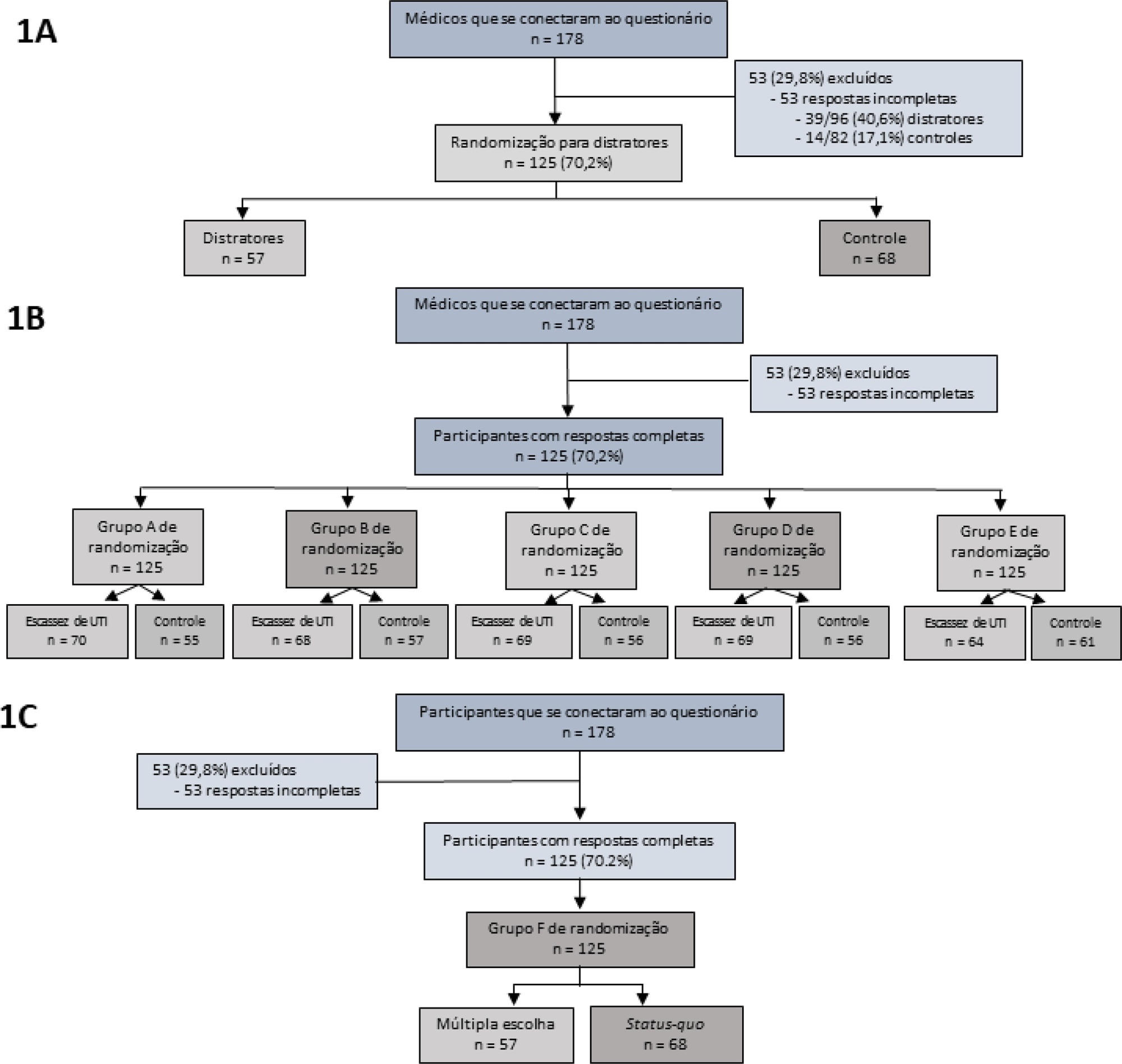
This study was a randomized factorial trial using patient-based vignettes. The vignettes were deemed archetypical for intensive care unit admission or refusal, as judged by a group of experts. Intensive care unit physicians were randomized to 1) an increased distraction (intervention) or a control group, 2) an intensive care unit bed scarcity or nonscarcity (availability) setting, and 3) a multiple-choice or omission (status quo) vignette scenario. The primary outcome was the proportion of appropriate intensive care unit allocations, defined as concordance with the allocation decision made by the group of experts.
Results:
We analyzed 125 physicians. Overall, distractors had no impact on the outcome; however, there was a differential drop-out rate, with fewer physicians in the intervention arm completing the questionnaire. Intensive care unit bed availability was associated with an inappropriate allocation of vignettes deemed inappropriate for intensive care unit admission (OR = 2.47; 95%CI 1.19 – 5.11) but not of vignettes appropriate for intensive care unit admission. There was a significant interaction with the presence of distractors (p = 0.007), with intensive care unit bed availability being associated with increased intensive care unit admission of vignettes inappropriate for intensive care unit admission in the distractor (intervention) arm (OR = 9.82; 95%CI 2.68 – 25.93) but not in the control group (OR = 1.02; 95%CI 0.38 – 2.72). Multiple choices were associated with increased inappropriate allocation in comparison to the omission group (OR = 5.18; 95%CI 1.37 – 19.61).
Conclusion:
Intensive care unit bed availability and cognitive biases were associated with inappropriate intensive care unit allocation decisions. These findings may have implications for intensive care unit admission policies.
-
Special Article
Accountability for reasonableness and criteria for admission, triage and discharge in intensive care units: an analysis of current ethical recommendations
Rev Bras Ter Intensiva. 2021;33(1):38-47
Abstract
Special ArticleAccountability for reasonableness and criteria for admission, triage and discharge in intensive care units: an analysis of current ethical recommendations
Rev Bras Ter Intensiva. 2021;33(1):38-47
DOI 10.5935/0103-507X.20210004
Views0See moreAbstract
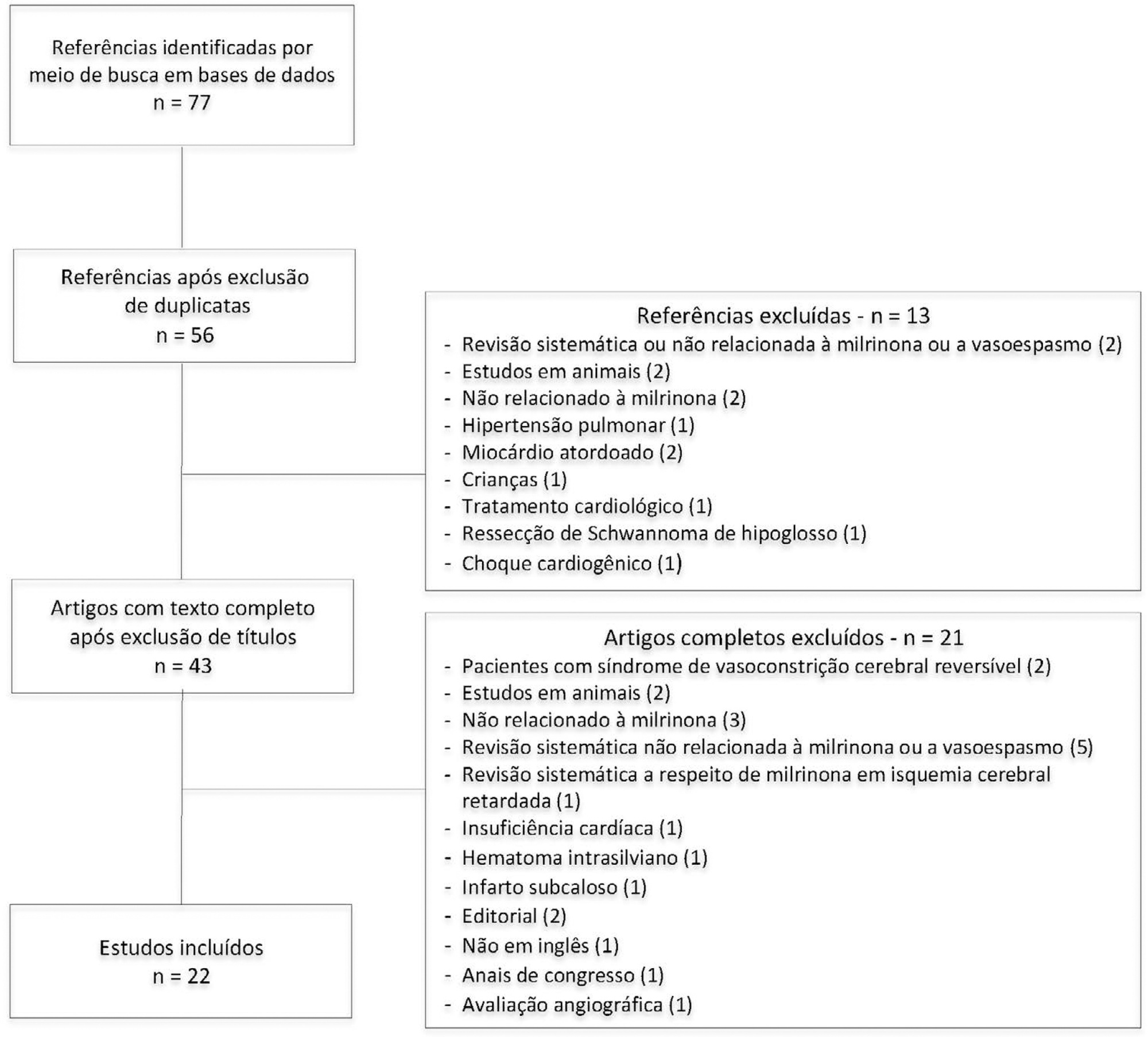
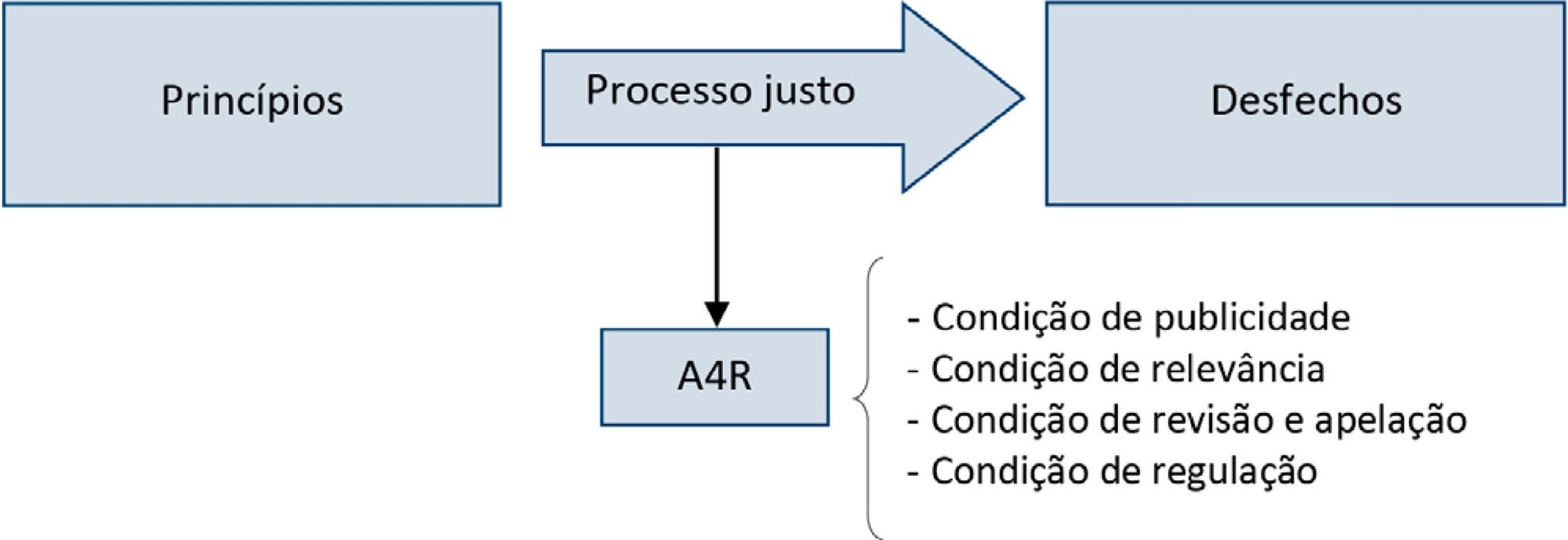
Triage for intensive care unit admission is a frequent event and is associated to worse clinical outcomes. The process of triage is variable and may be influenced by biases and prejudices, which could lead to potentially unfair decisions. The Brazilian Federal Council of Medicine (Conselho Federal de Medicina) has recently released a guideline for intensive care unit admission and discharge. The aim of this paper is to evaluate the ethical dilemmas related to the implementation of this guideline, through the accountability for reasonabless approach, known as A4R, as elaborated by Norman Daniels. We conclude that the guideline contemplates A4R conditions, but we observe that there is a need for indication of A4R-concordant criteria to operationalize the guidelines.
-
Original Article
Neuromuscular blockade and airway management during endotracheal intubation in Brazilian intensive care units: a national survey
Rev Bras Ter Intensiva. 2020;32(3):433-438
Abstract
Original ArticleNeuromuscular blockade and airway management during endotracheal intubation in Brazilian intensive care units: a national survey
Rev Bras Ter Intensiva. 2020;32(3):433-438
DOI 10.5935/0103-507X.20200073
Views0Abstract
Objective:
To describe the use of neuromuscular blockade as well as other practices among Brazilian physicians in adult intensive care units.
Methods:
An online national survey was designed and administered to Brazilian intensivists. Questions were selected using the Delphi method and assessed physicians’ demographic data, intensive care unit characteristics, practices regarding airway management, use of neuromuscular blockade and sedation during endotracheal intubation in the intensive care unit. As a secondary outcome, we applied a multivariate analysis to evaluate factors associated with the use of neuromuscular blockade.
Results:
Five hundred sixty-five intensivists from all Brazilian regions responded to the questionnaire. The majority of respondents were male (65%), with a mean age of 38 ( 8.4 years, and 58.5% had a board certification in critical care. Only 40.7% of the intensivists reported the use of neuromuscular blockade during all or in more than 75% of endotracheal intubations. In the multivariate analysis, the number of intubations performed monthly and physician specialization in anesthesiology were directly associated with frequent use of neuromuscular blockade. Etomidate and ketamine were more commonly used in the clinical situation of hypotension and shock, while propofol and midazolam were more commonly prescribed in the situation of clinical stability.
Conclusion:
The reported use of neuromuscular blockade was low among intensivists, and sedative drugs were chosen in accordance with patient hemodynamic stability. These results may help the design of future studies regarding airway management in Brazil.
Keywords:Airway managementBrazilHypnotics and sedativesIntensive care unitsIntubationNeuromuscular blockadeSee more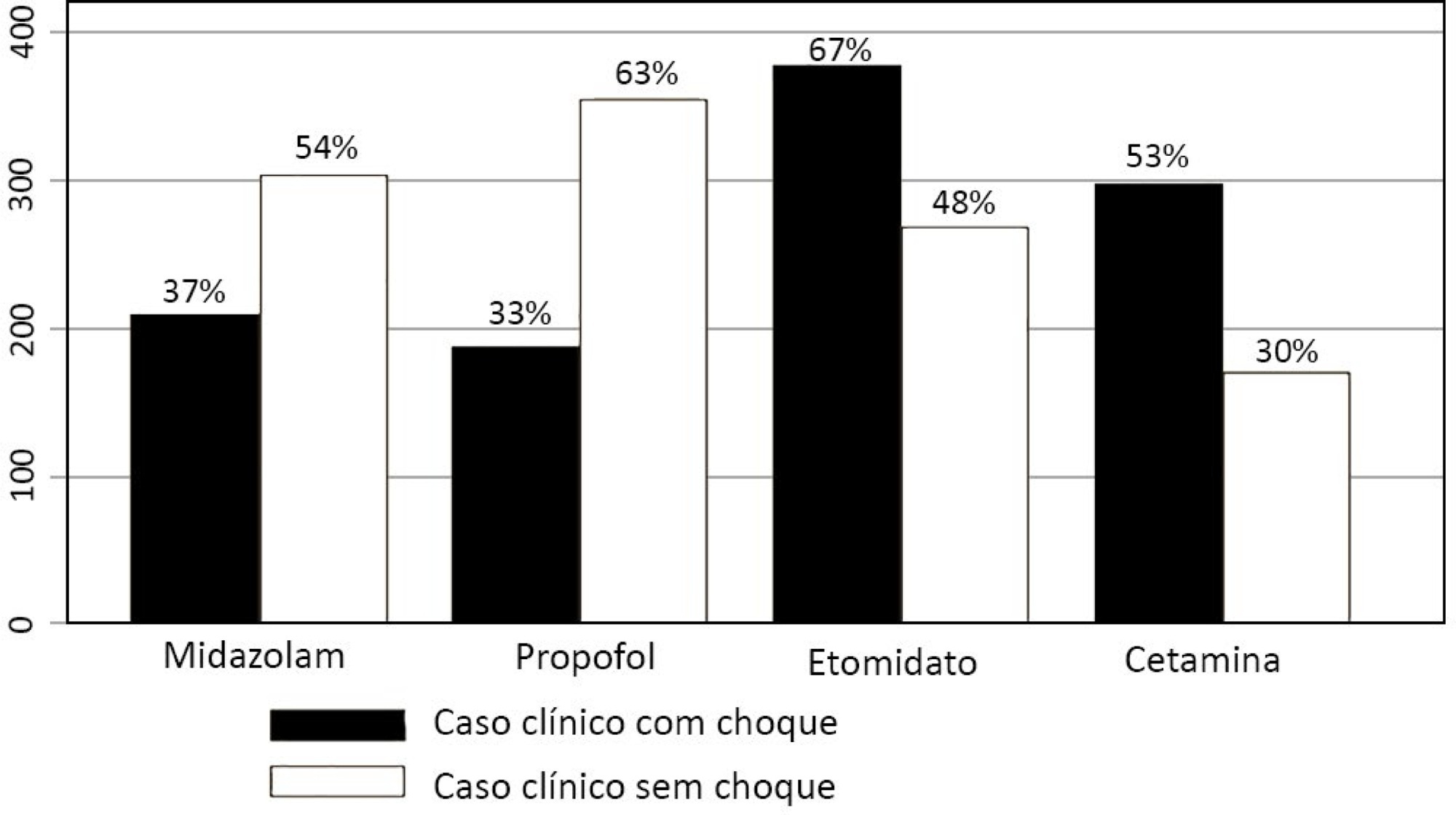
-
Original Article
Effect of a palliative care program on trends in intensive care unit utilization and do-not-resuscitate orders during terminal hospitalizations. An interrupted time series analysis
Rev Bras Ter Intensiva. 2018;30(3):308-316
Abstract
Original ArticleEffect of a palliative care program on trends in intensive care unit utilization and do-not-resuscitate orders during terminal hospitalizations. An interrupted time series analysis
Rev Bras Ter Intensiva. 2018;30(3):308-316
DOI 10.5935/0103-507X.20180042
Views2ABSTRACT
Objective:
To assess the effect of the implementation of a palliative care program on do-not-resuscitate orders and intensive care unit utilization during terminal hospitalizations.
Methods:
Data were retrospectively collected for all patients who died in a tertiary hospital in Brazil from May 2014 to September 2016. We analyzed the frequency of do-not-resuscitate orders and intensive care unit admissions among in-hospital deaths. Interrupted time series analyses were used to evaluate differences in trends of do-not-resuscitate orders and intensive care unit admissions before (17 months) and after (12 months) the implementation of a palliative care program.
Results:
We analyzed 48,372 hospital admissions and 1,071 in-hospital deaths. Deaths were preceded by do-not-resuscitate orders in 276 (25.8%) cases and admissions to the intensive care unit occurred in 814 (76%) cases. Do-not-resuscitate orders increased from 125 (20.4%) to 151 (33%) cases in the pre-implementation and post-implementation periods, respectively (p < 0.001). Intensive care unit admissions occurred in 469 (76.5%) and 345 (75.3%) cases in the pre-implementation and post-implementation periods, respectively (p = 0.654). Interrupted time series analyses confirmed a trend of increased do-not-resuscitate order registrations, from an increase of 0.5% per month pre-implementation to an increase of 2.9% per month post-implementation (p < 0.001), and demonstrated a trend of decreased intensive care unit utilization, from an increase of 0.6% per month pre-implementation to a decrease of -0.9% per month in the post-implementation period (p = 0.001).
Conclusion:
The implementation of a palliative care program was associated with a trend of increased registration of do-not-resuscitate orders and a trend of decreased intensive care unit utilization during terminal hospitalizations.
Keywords:Intensive care unitsInterrupted time series analysisPalliative CarePatient care planningResuscitation OrdersSee more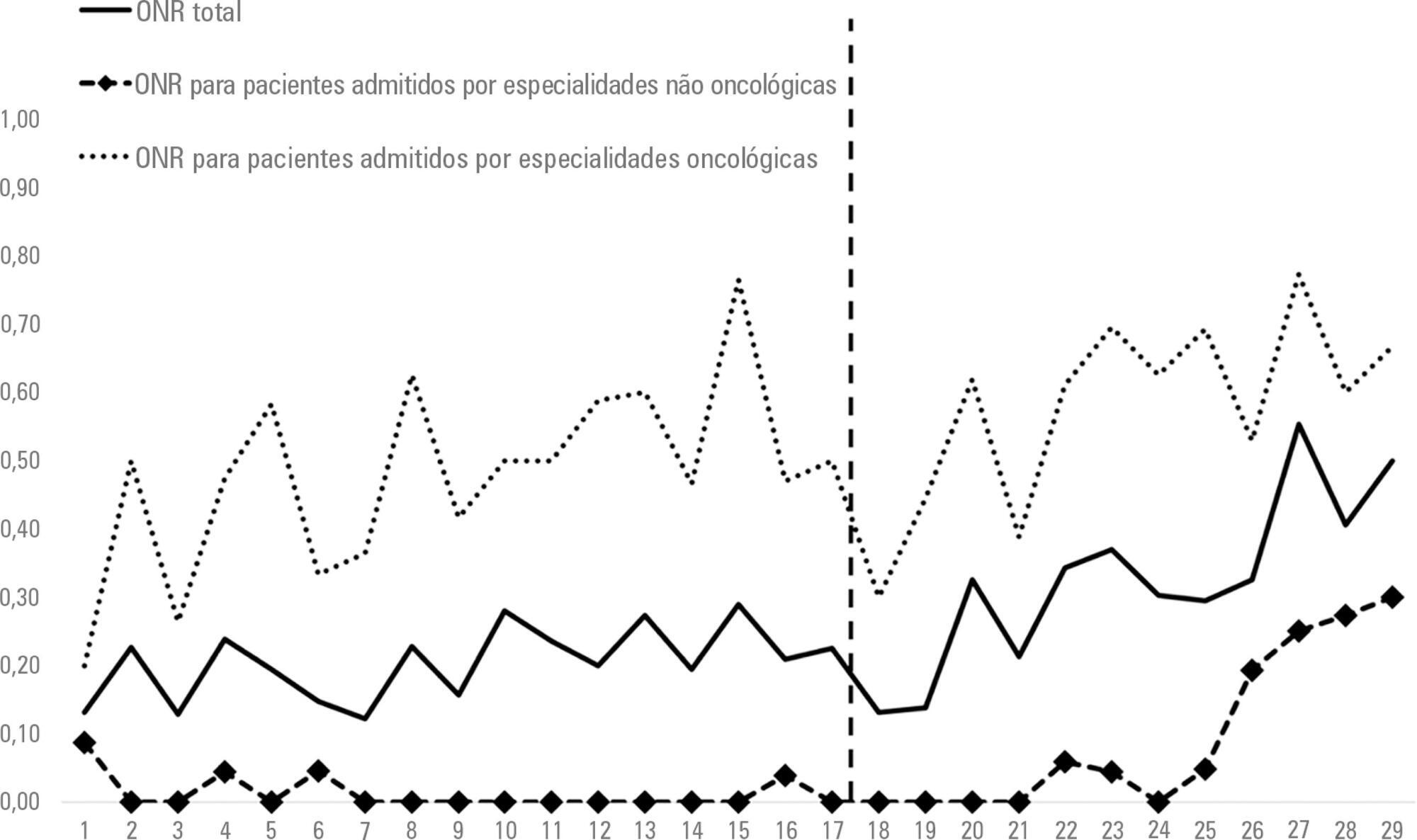
-
Original Articles
Factors potentially associated with the decision of admission to the intensive care unit in a middle-income country: a survey of Brazilian physicians
Rev Bras Ter Intensiva. 2017;29(2):154-162
Abstract
Original ArticlesFactors potentially associated with the decision of admission to the intensive care unit in a middle-income country: a survey of Brazilian physicians
Rev Bras Ter Intensiva. 2017;29(2):154-162
DOI 10.5935/0103-507X.20170025
Views0See moreABSTRACT
Objective:
To evaluate the factors potentially associated with the decision of admission to the intensive care unit in Brazil.
Methods:
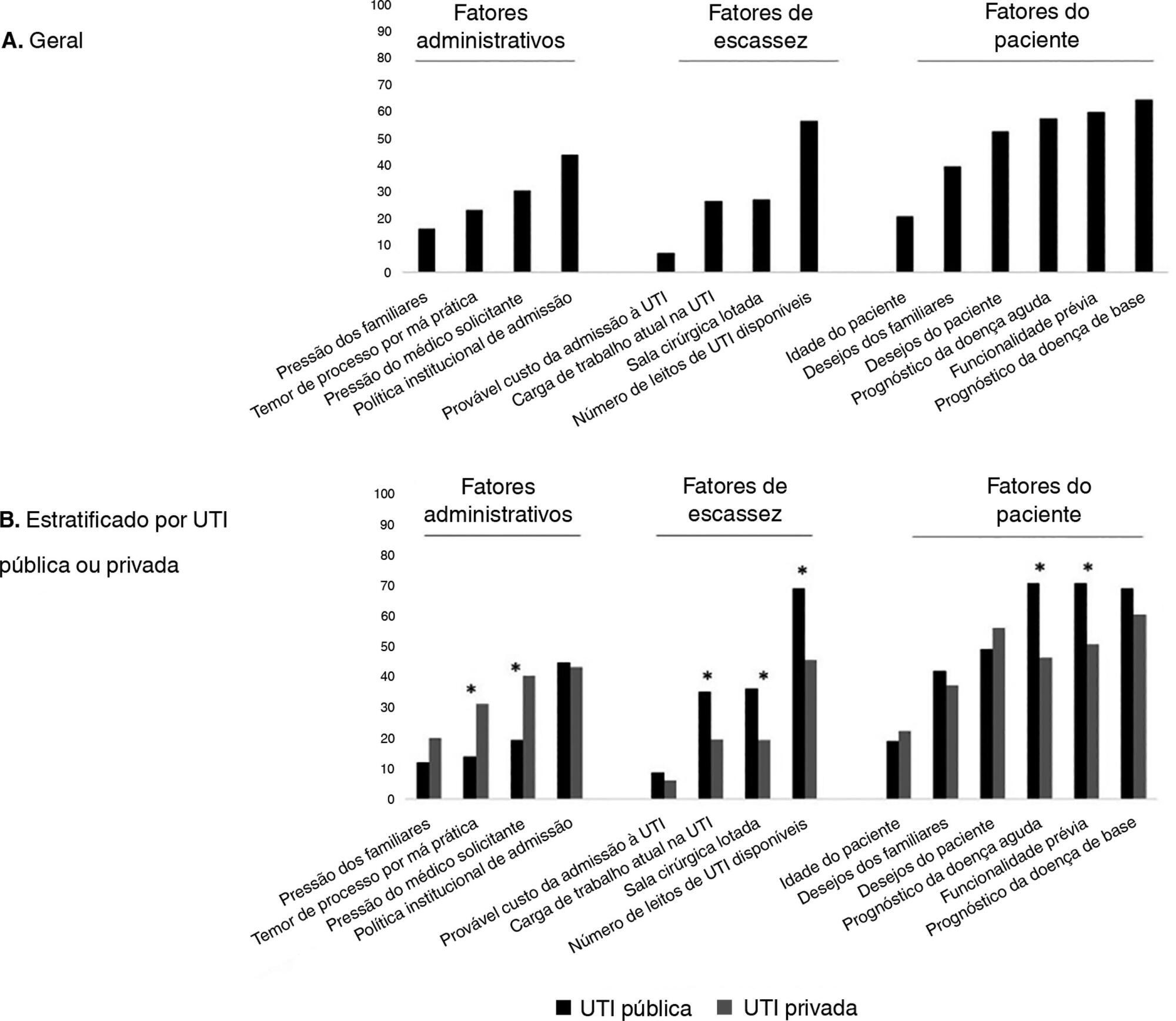
An electronic survey of Brazilian physicians working in intensive care units. Fourteen variables that were potentially associated with the decision of admission to the intensive care unit were rated as important (from 1 to 5) by the respondents and were later grouped as “patient-related,” “scarcity-related” and “administrative-related” factors. The workplace and physician characteristics were evaluated for correlation with the factor ratings.
Results:
During the study period, 125 physicians completed the survey. The scores on patient-related factors were rated higher on their potential to affect decisions than scarcity-related or administrative-related factors, with a mean ± SD of 3.42 ± 0.7, 2.75 ± 0.7 and 2.87 ± 0.7, respectively (p < 0.001). The patient's underlying illness prognosis was rated by 64.5% of the physicians as always or frequently affecting decisions, followed by acute illness prognosis (57%), number of intensive care unit beds available (56%) and patient's wishes (53%). After controlling for confounders, receiving specific training on intensive care unit triage was associated with higher ratings of the patient-related factors and scarcity-related factors, while working in a public intensive care unit (as opposed to a private intensive care unit) was associated with higher ratings of the scarcity-related factors.
Conclusions:
Patient-related factors were more frequently rated as potentially affecting intensive care unit admission decisions than scarcity-related or administrative-related factors. Physician and workplace characteristics were associated with different factor ratings.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis