Abstract
Rev Bras Ter Intensiva. 2018;30(3):308-316
DOI 10.5935/0103-507X.20180042
To assess the effect of the implementation of a palliative care program on do-not-resuscitate orders and intensive care unit utilization during terminal hospitalizations.
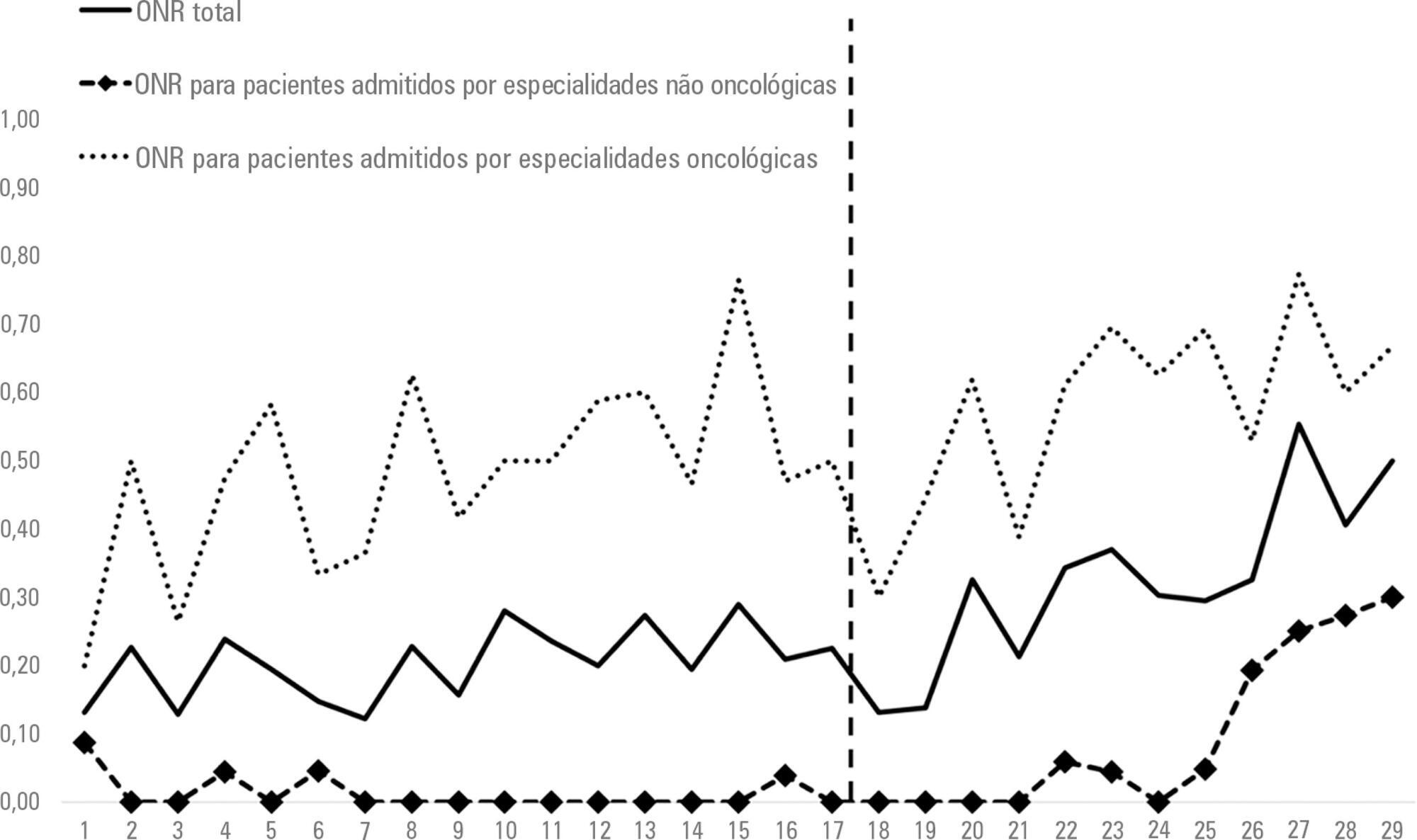
Data were retrospectively collected for all patients who died in a tertiary hospital in Brazil from May 2014 to September 2016. We analyzed the frequency of do-not-resuscitate orders and intensive care unit admissions among in-hospital deaths. Interrupted time series analyses were used to evaluate differences in trends of do-not-resuscitate orders and intensive care unit admissions before (17 months) and after (12 months) the implementation of a palliative care program.
We analyzed 48,372 hospital admissions and 1,071 in-hospital deaths. Deaths were preceded by do-not-resuscitate orders in 276 (25.8%) cases and admissions to the intensive care unit occurred in 814 (76%) cases. Do-not-resuscitate orders increased from 125 (20.4%) to 151 (33%) cases in the pre-implementation and post-implementation periods, respectively (p < 0.001). Intensive care unit admissions occurred in 469 (76.5%) and 345 (75.3%) cases in the pre-implementation and post-implementation periods, respectively (p = 0.654). Interrupted time series analyses confirmed a trend of increased do-not-resuscitate order registrations, from an increase of 0.5% per month pre-implementation to an increase of 2.9% per month post-implementation (p < 0.001), and demonstrated a trend of decreased intensive care unit utilization, from an increase of 0.6% per month pre-implementation to a decrease of -0.9% per month in the post-implementation period (p = 0.001).
The implementation of a palliative care program was associated with a trend of increased registration of do-not-resuscitate orders and a trend of decreased intensive care unit utilization during terminal hospitalizations.
Abstract
Rev Bras Ter Intensiva. 2007;19(2):137-143
DOI 10.1590/S0103-507X2007000200001
BACKGROUND AND OBJECTIVES: There is a growing tendency of looking for "dying with dignity", rather than to prolong death and suffering of terminal patients on intensive care units (ICU). This study aims to evaluate medical practices that suggest therapeutic limitation (TL) in patients who died in an adult ICU. METHODS: A retrospective exploratory study was carried out to evaluate medical records of patients who died in a general adult ICU of a private hospital in Salvador-BA, between January and August of 2003, after at least 24 hours from the admission. The patients were classified, in relation to their deaths, in: "not responding to cardiopulmonary resuscitation", "brain death", "decision not to resuscitate" (DNR) and "withhold or withdrawal life-support measures". RESULTS: Sixty seven patients were included, corresponding to 90.4% of the deaths occurred in this ICU during the referred period. The most of them (56.7%) were women and the patients’ mean age was 66.58 ± 17.86 years. Suggestive measures of TL were found in 59.7% of the patients, being "withhold of life-support measures" the most important (35.8%), followed by DNR (17.9%) and "withdrawal of life-support measures" (6%). The procedures most commonly omitted were use of vasoactive drugs and dialysis, while antibiotics were the most discontinued. The use of TL measures was more frequent in clinical patients. CONCLUSIONS: The results of the present study suggest high frequencies of medical conducts suggestive of TL in a general ICU in Northeast of Brazil. Therapeutic methods that could cause discomfort or suffering to the patients, as nutrition, sedation and analgesia, were rarely omitted or discontinued.