Abstract
Rev Bras Ter Intensiva. 2022;34(2):220-226
DOI 10.5935/0103-507X.20220019-en
To compare the predictive performance of residents, senior intensive care unit physicians and surrogates early during intensive care unit stays and to evaluate whether different presentations of prognostic data (probability of survival versus probability of death) influenced their performance.
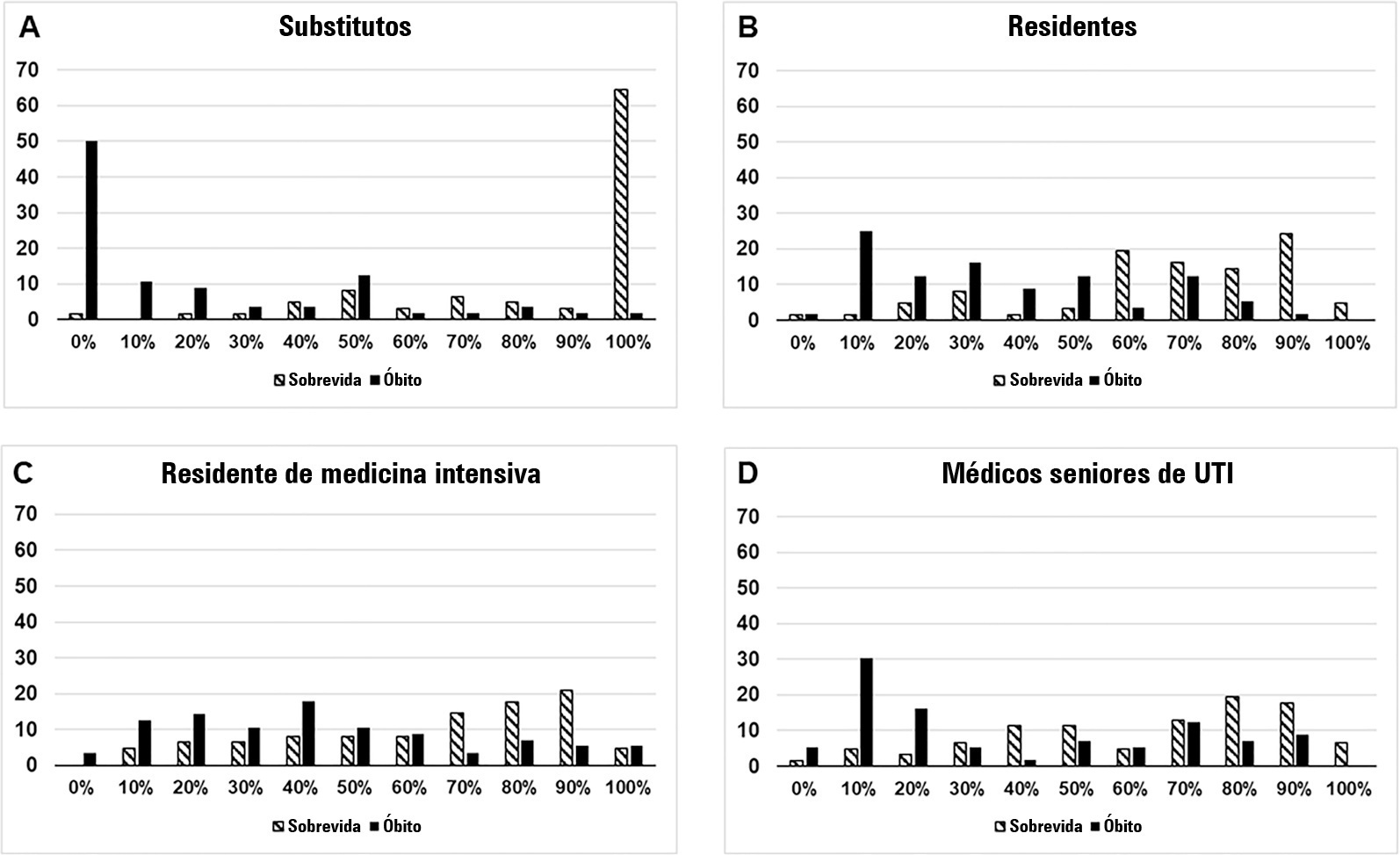
We questioned surrogates and physicians in charge of critically ill patients during the first 48 hours of intensive care unit admission on the patient’s probability of hospital outcome. The question framing (i.e., probability of survival versus probability of death during hospitalization) was randomized. To evaluate the predictive performance, we compared the areas under the ROC curves (AUCs) for hospital outcome between surrogates and physicians’ categories. We also stratified the results according to randomized question framing.
We interviewed surrogates and physicians on the hospital outcomes of 118 patients. The predictive performance of surrogate decisionmakers was significantly lower than that of physicians (AUC of 0.63 for surrogates, 0.82 for residents, 0.80 for intensive care unit fellows and 0.81 for intensive care unit senior physicians). There was no increase in predictive performance related to physicians’ experience (i.e., senior physicians did not predict outcomes better than junior physicians). Surrogate decisionmakers worsened their prediction performance when they were asked about probability of death instead of probability of survival, but there was no difference for physicians.
Different predictive performance was observed when comparing surrogate decision-makers and physicians, with no effect of experience on health care professionals’ prediction. Question framing affected the predictive performance of surrogates but not of physicians.
Abstract
Rev Bras Ter Intensiva. 2009;21(2):135-140
DOI 10.1590/S0103-507X2009000200004
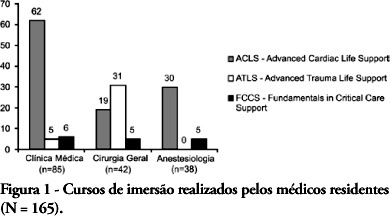
OBJECTIVES: Critical Care Medicine is a relatively new specialty, which in recent years has made significant progress in Brazil. However, few physicians are willing to acquire this specialization. The main objective of this study was to describe the factors associated with choice of Critical Care Medicine as a specialty by medical residents of Salvador-BA. METHODS: A cross-sectional and descriptive study, in which a questionnaire was submitted to all residents of the specialties that are a prerequisite for Critical Care Medicine (Clinical Medicine, General Surgery and Anesthesiology), between October and December 2007. RESULTS: The study included 165 residents (89.7% of the total), in which 51.5% were clinical medicine residents, 25.5% were general surgery residents, and 23.0% were anesthesiology residents. Of the respondents, 14 (9.1%) intended to enter Critical Care Medicine residency, although 90 (54.5%) were willing to become intensive care unit physicians after their regular residency. The main reason stated to specialize in critical care medicine was to like work with critically ill patients (92.9%). The main reasons stated not to specialize in critical care medicine, however were related with the poorer quality of life and work. Residents who did intensive care unit initernship during medical studies were more likely to work in an intensive care units after residency. CONCLUSIONS: This population showed little interest to specialize in critical care medicine. The main reasons given for this limited interest were factors related to quality of life and intensive care unit environment. A national survey is required to identify the interventions needed to favor this specialization.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)