To investigate the impact of delirium severity in critically ill COVID-19 patients and its association with outcomes.
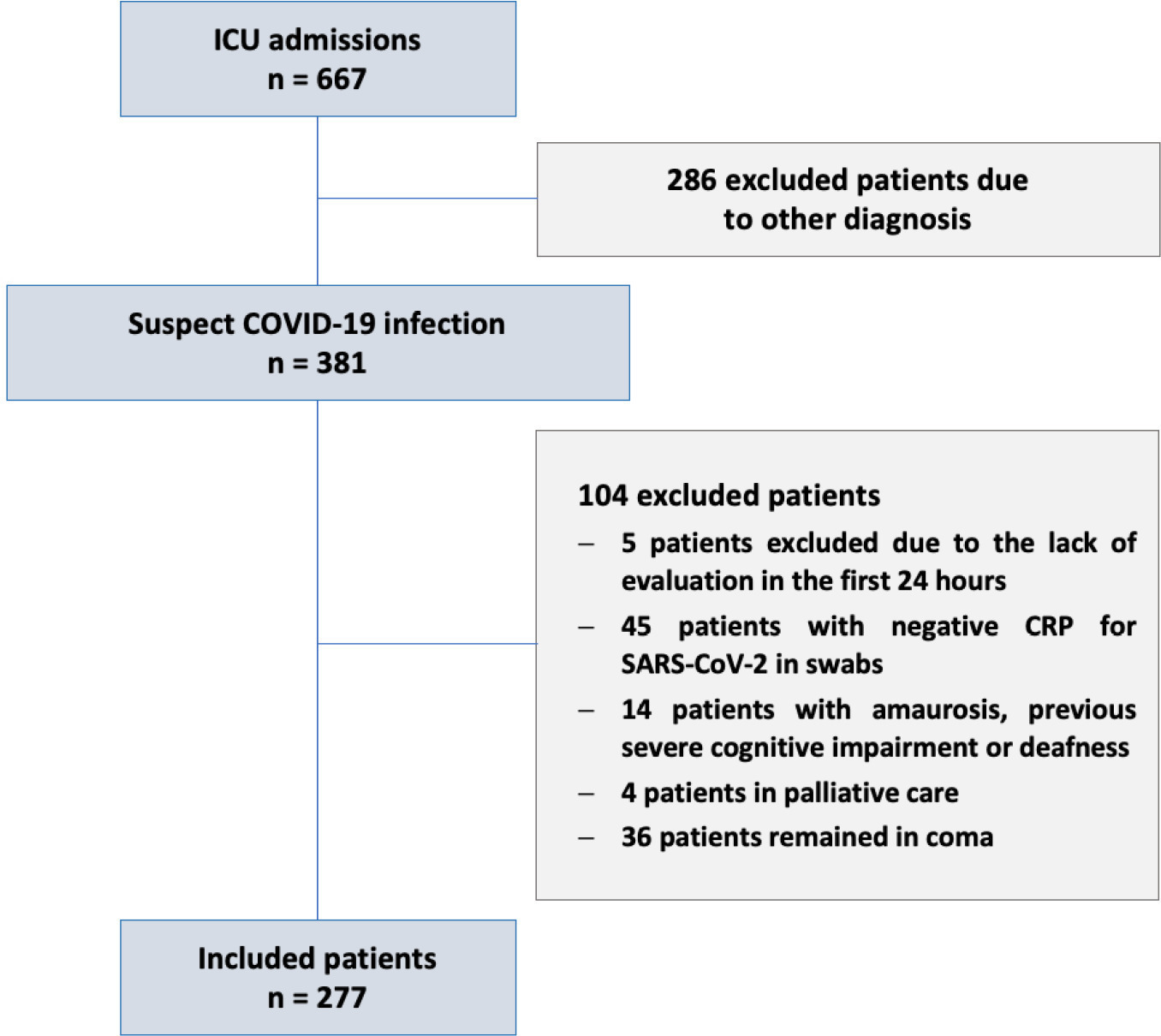
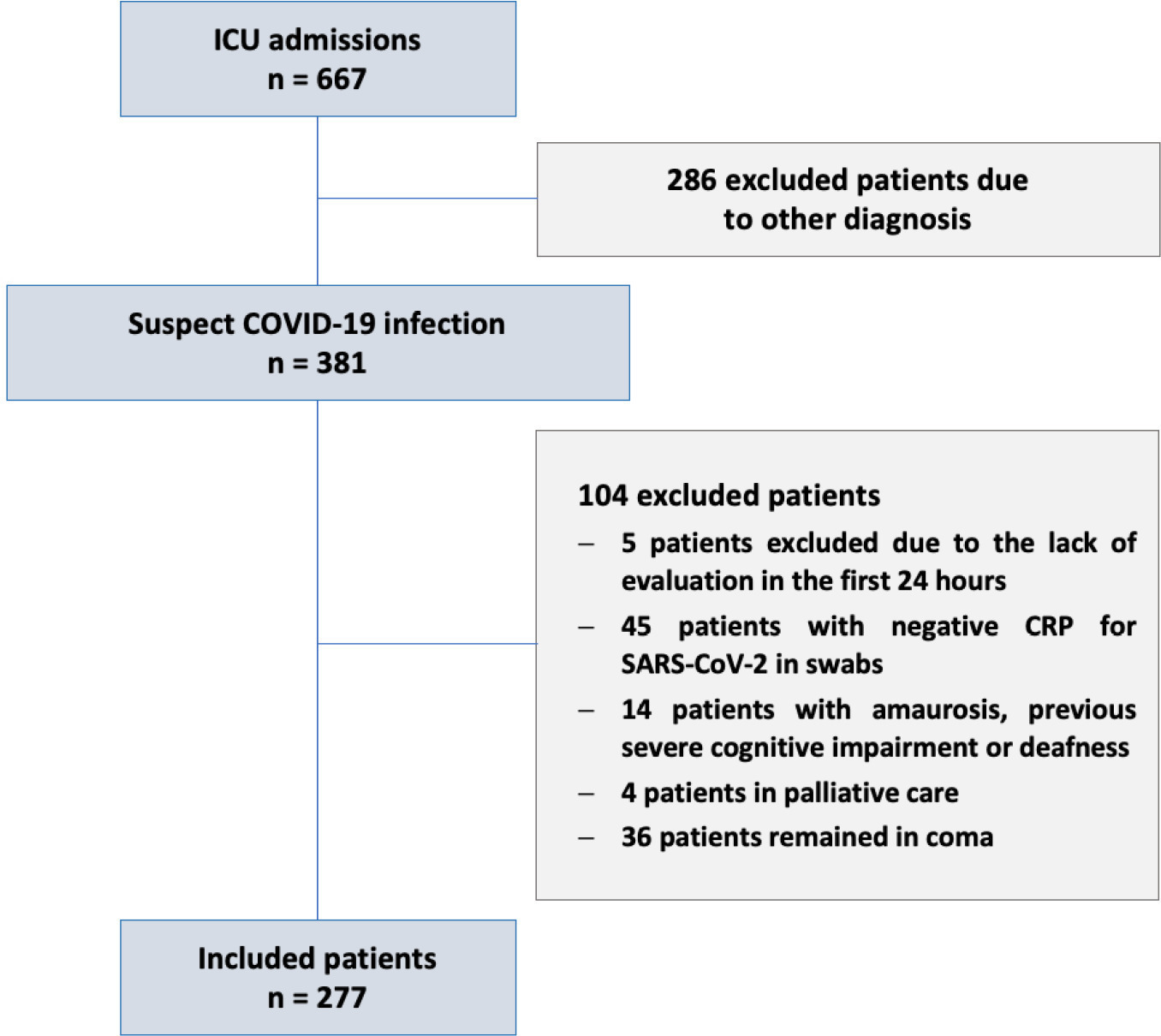
This prospective cohort study was performed in two tertiary intensive care units in Rio de Janeiro, Brazil. COVID-19 patients were evaluated daily during the first 7 days of intensive care unit stay using the Richmond Agitation Sedation Scale, Confusion Assessment Method for Intensive Care Unit (CAM-ICU) and Confusion Method Assessment for Intensive Care Unit-7 (CAM-ICU-7). Delirium severity was correlated with outcomes and one-year mortality.
Among the 277 COVID-19 patients included, delirium occurred in 101 (36.5%) during the first 7 days of intensive care unit stay, and it was associated with a higher length of intensive care unit stay in days (IQR 13 [7 – 25] versus 6 [4 – 12]; p < 0.001), higher hospital mortality (25.74% versus 5.11%; p < 0.001) and additional higher one-year mortality (5.3% versus 0.6%, p < 0.001). Delirium was classified by CAM-ICU-7 in terms of severity, and higher scores were associated with higher in-hospital mortality (17.86% versus 34.38% versus 38.46%, 95%CI, p value < 0.001). Severe delirium was associated with a higher risk of progression to coma (OR 7.1; 95%CI 1.9 – 31.0; p = 0.005) and to mechanical ventilation (OR 11.09; 95%CI 2.8 – 58.5; p = 0.002) in the multivariate analysis, adjusted by severity and frailty.
In patients admitted with COVID-19 in the intensive care unit, delirium was an independent risk factor for the worst prognosis, including mortality. The delirium severity assessed by the CAM-ICU-7 during the first week in the intensive care unit was associated with poor outcomes, including progression to coma and to mechanical ventilation.
Search
Search in:

Comments