Home » Psychiatric status rating scales
Abstract
Crit Care Sci. 2023;35(4):394-401
DOI 10.5935/2965-2774.20230170-pt
To investigate the impact of delirium severity in critically ill COVID-19 patients and its association with outcomes.
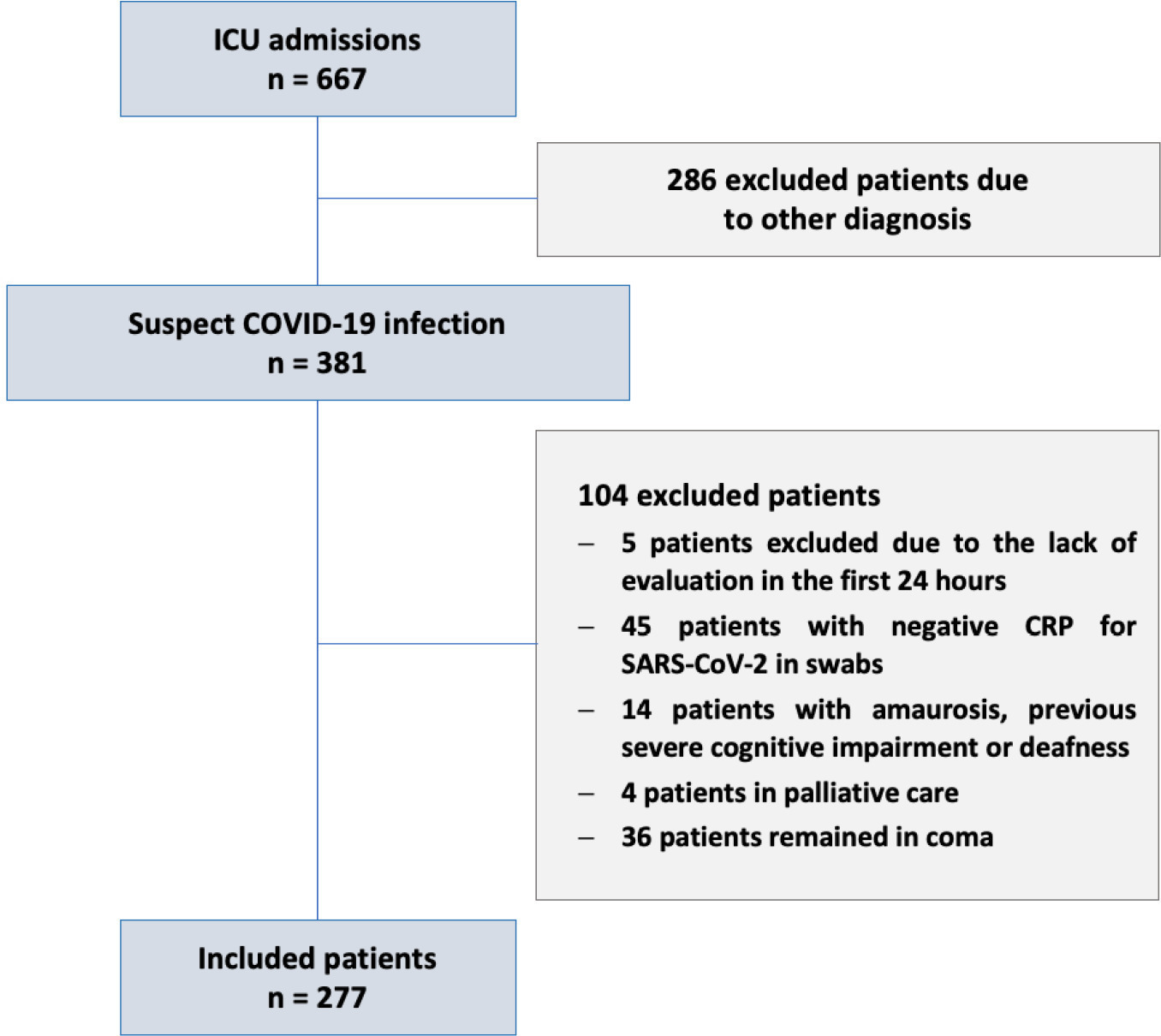
This prospective cohort study was performed in two tertiary intensive care units in Rio de Janeiro, Brazil. COVID-19 patients were evaluated daily during the first 7 days of intensive care unit stay using the Richmond Agitation Sedation Scale, Confusion Assessment Method for Intensive Care Unit (CAM-ICU) and Confusion Method Assessment for Intensive Care Unit-7 (CAM-ICU-7). Delirium severity was correlated with outcomes and one-year mortality.
Among the 277 COVID-19 patients included, delirium occurred in 101 (36.5%) during the first 7 days of intensive care unit stay, and it was associated with a higher length of intensive care unit stay in days (IQR 13 [7 - 25] versus 6 [4 - 12]; p < 0.001), higher hospital mortality (25.74% versus 5.11%; p < 0.001) and additional higher one-year mortality (5.3% versus 0.6%, p < 0.001). Delirium was classified by CAM-ICU-7 in terms of severity, and higher scores were associated with higher in-hospital mortality (17.86% versus 34.38% versus 38.46%, 95%CI, p value < 0.001). Severe delirium was associated with a higher risk of progression to coma (OR 7.1; 95%CI 1.9 - 31.0; p = 0.005) and to mechanical ventilation (OR 11.09; 95%CI 2.8 - 58.5; p = 0.002) in the multivariate analysis, adjusted by severity and frailty.
In patients admitted with COVID-19 in the intensive care unit, delirium was an independent risk factor for the worst prognosis, including mortality. The delirium severity assessed by the CAM-ICU-7 during the first week in the intensive care unit was associated with poor outcomes, including progression to coma and to mechanical ventilation.


Abstract
Crit Care Sci. 2023;35(4):394-401
DOI 10.5935/2965-2774.20230170-pt
To investigate the impact of delirium severity in critically ill COVID-19 patients and its association with outcomes.
This prospective cohort study was performed in two tertiary intensive care units in Rio de Janeiro, Brazil. COVID-19 patients were evaluated daily during the first 7 days of intensive care unit stay using the Richmond Agitation Sedation Scale, Confusion Assessment Method for Intensive Care Unit (CAM-ICU) and Confusion Method Assessment for Intensive Care Unit-7 (CAM-ICU-7). Delirium severity was correlated with outcomes and one-year mortality.
Among the 277 COVID-19 patients included, delirium occurred in 101 (36.5%) during the first 7 days of intensive care unit stay, and it was associated with a higher length of intensive care unit stay in days (IQR 13 [7 - 25] versus 6 [4 - 12]; p < 0.001), higher hospital mortality (25.74% versus 5.11%; p < 0.001) and additional higher one-year mortality (5.3% versus 0.6%, p < 0.001). Delirium was classified by CAM-ICU-7 in terms of severity, and higher scores were associated with higher in-hospital mortality (17.86% versus 34.38% versus 38.46%, 95%CI, p value < 0.001). Severe delirium was associated with a higher risk of progression to coma (OR 7.1; 95%CI 1.9 - 31.0; p = 0.005) and to mechanical ventilation (OR 11.09; 95%CI 2.8 - 58.5; p = 0.002) in the multivariate analysis, adjusted by severity and frailty.
In patients admitted with COVID-19 in the intensive care unit, delirium was an independent risk factor for the worst prognosis, including mortality. The delirium severity assessed by the CAM-ICU-7 during the first week in the intensive care unit was associated with poor outcomes, including progression to coma and to mechanical ventilation.


Abstract
Rev Bras Ter Intensiva. 2018;30(1):50-56
DOI 10.5935/0103-507X.20180010
To describe the incidence of and risk factors for delirium in the intensive care unit of a tertiary care teaching hospital in Argentina and to conduct the first non-European study exploring the performance of the PREdiction of DELIRium in ICu patients (PRE-DELIRIC) model.
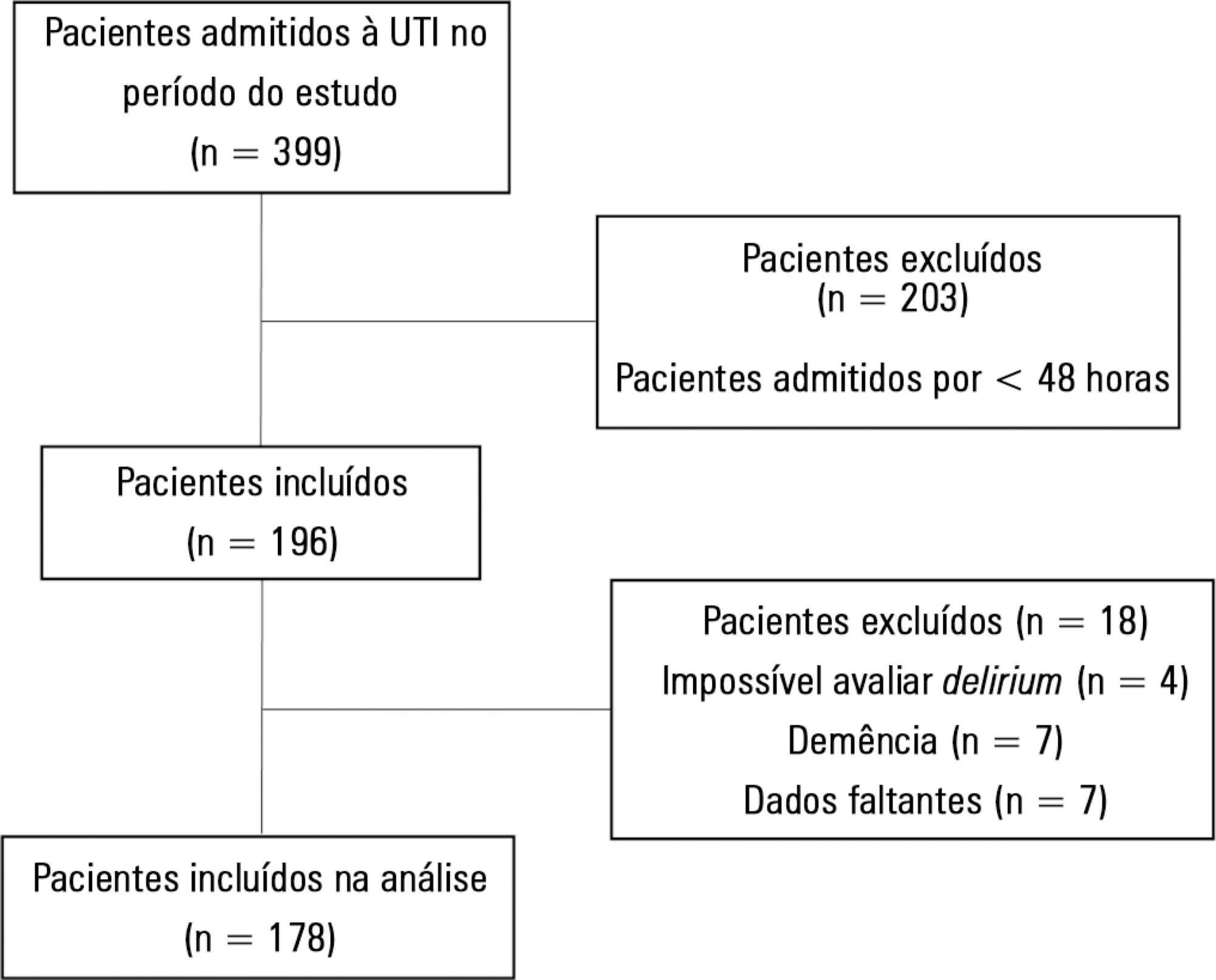
Prospective observational study in a 20-bed intensive care unit of a tertiary care teaching hospital in Buenos Aires, Argentina. The PRE-DELIRIC model was applied to 178 consecutive patients within 24 hours of admission to the intensive care unit; delirium was assessed with the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU).
The mean age was 64.3 ± 17.9 years. The median time of stay in the intensive care unit was 6 (range, 2 - 56) days. Of the total number of patients, 49/178 (27.5%) developed delirium, defined as a positive CAM-ICU assessment, during their stay in the intensive care unit. Patients in the delirium group were significantly older and had a significantly higher Acute Physiological and Chronic Health Evaluation II (APACHE II) score. The mortality rate in the intensive care unit was 14.6%; no significant difference was observed between the two groups. Predictive factors for the development of delirium were increased age, prolonged intensive care unit stay, and opioid use. The area under the curve for the PRE-DELIRIC model was 0.83 (95%CI; 0.77 - 0.90).
The observed incidence of delirium highlights the importance of this problem in the intensive care unit setting. In this first study conducted outside Europe, PRE-DELIRIC accurately predicted the development of delirium.


Abstract
Rev Bras Ter Intensiva. 2018;30(1):50-56
DOI 10.5935/0103-507X.20180010
To describe the incidence of and risk factors for delirium in the intensive care unit of a tertiary care teaching hospital in Argentina and to conduct the first non-European study exploring the performance of the PREdiction of DELIRium in ICu patients (PRE-DELIRIC) model.
Prospective observational study in a 20-bed intensive care unit of a tertiary care teaching hospital in Buenos Aires, Argentina. The PRE-DELIRIC model was applied to 178 consecutive patients within 24 hours of admission to the intensive care unit; delirium was assessed with the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU).
The mean age was 64.3 ± 17.9 years. The median time of stay in the intensive care unit was 6 (range, 2 - 56) days. Of the total number of patients, 49/178 (27.5%) developed delirium, defined as a positive CAM-ICU assessment, during their stay in the intensive care unit. Patients in the delirium group were significantly older and had a significantly higher Acute Physiological and Chronic Health Evaluation II (APACHE II) score. The mortality rate in the intensive care unit was 14.6%; no significant difference was observed between the two groups. Predictive factors for the development of delirium were increased age, prolonged intensive care unit stay, and opioid use. The area under the curve for the PRE-DELIRIC model was 0.83 (95%CI; 0.77 - 0.90).
The observed incidence of delirium highlights the importance of this problem in the intensive care unit setting. In this first study conducted outside Europe, PRE-DELIRIC accurately predicted the development of delirium.


Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)


