Abstract
Rev Bras Ter Intensiva. 2022;34(4):524-528
DOI 10.5935/0103-507X.20220342-en
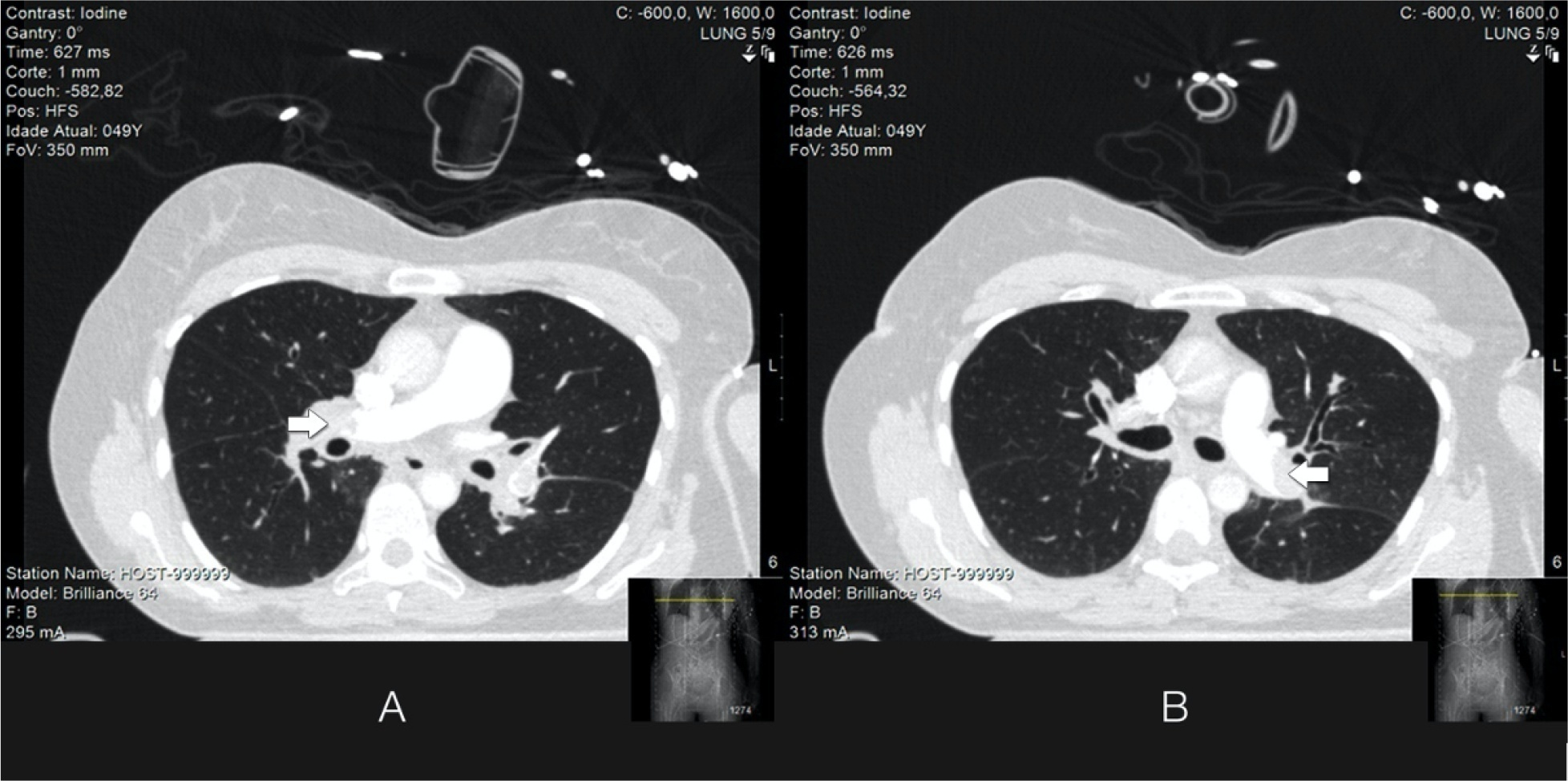
Acute massive pulmonary embolism is the most serious presentation of venous thromboembolism that can ultimately cause obstructive shock, leading to cardiac arrest and death. In this case report, the authors present a case of a 49-year-old female who successfully recovered from a massive pulmonary embolism with the combined use of venoarterial extracorporeal membrane oxygenation and pulmonary aspiration thrombectomy, with no complications from these procedures. Although evidence of benefit from mechanical support has not been established for patients with massive pulmonary embolism, the implementation of extracorporeal cardiocirculatory support during resuscitation may allow improvement of systemic organ perfusion and better chance of survival. Recent guidelines from the European Society of Cardiology state that venoarterial extracorporeal membrane oxygenation in combination with catheter-directed treatment may be considered for patients presenting with massive pulmonary embolism and refractory cardiac arrest. The use of extracorporeal membrane oxygenation as a stand-alone technique with anticoagulation remains controversial, and additional therapies, such as surgical or percutaneous embolectomy, must be considered. Since this intervention is not supported by high-quality studies, we believe it is important to report real-world successful cases. With this case report, we illustrate the benefit derived from resuscitation assisted by extracorporeal mechanical support and early aspiration thrombectomy in patients with massive pulmonary embolism. Additionally, it emphasizes the synergy that derives from integrated multidisciplinary systems for providing complex interventions, of which extracorporeal membrane oxygenation and Interventional Cardiology are clear examples.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):346-352
DOI 10.5935/0103-507X.20210053
To assess pulmonary embolism incidence, its relationship with D-dimer levels and other possible associated factors in addition to anticoagulation and contrast medium adverse effects.
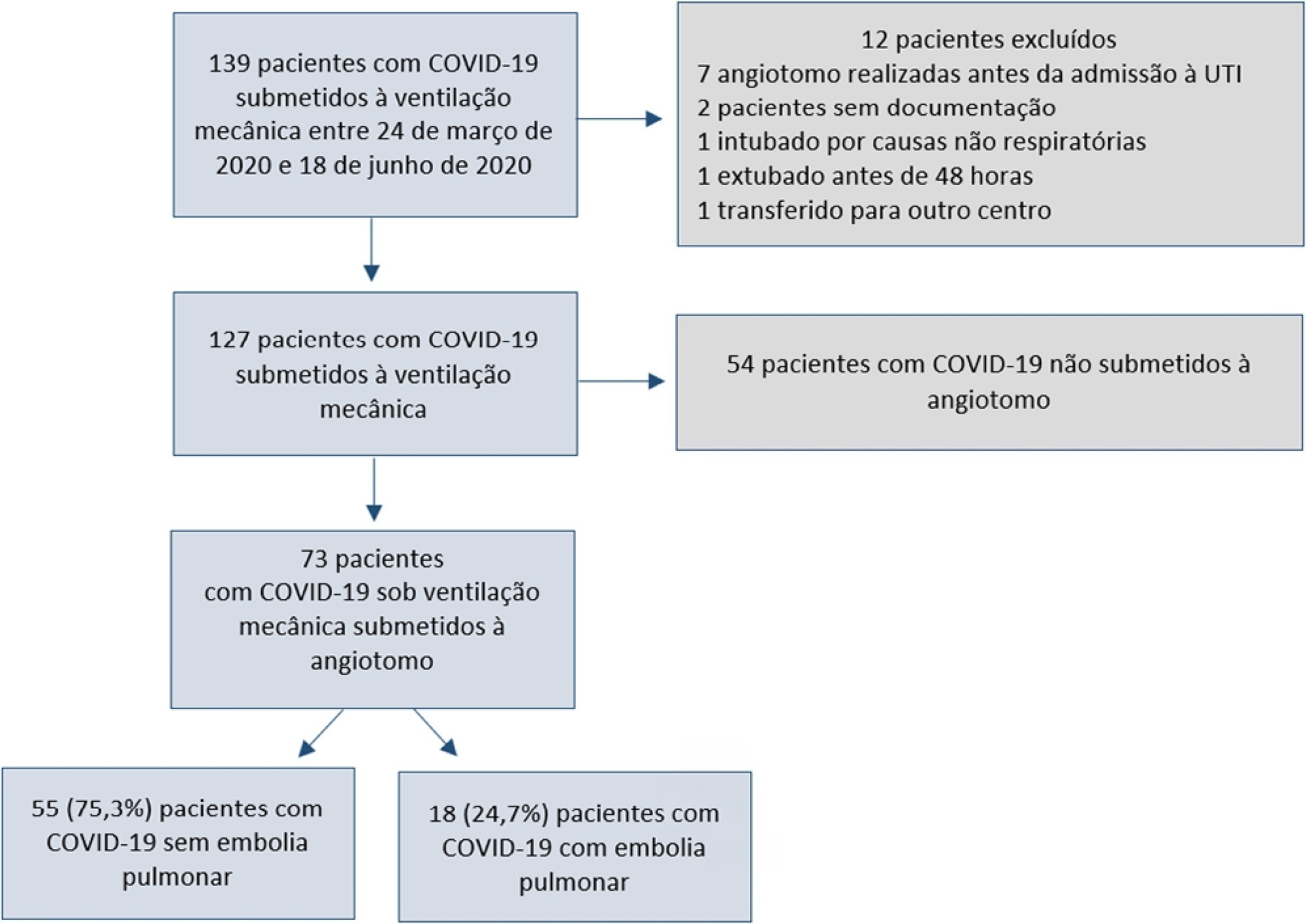
A retrospective observational cohort study at a Chilean public hospital was performed. Intensive care unit mechanically ventilated COVID-19 patients older than 18 years old between March and June 2020 were included. All patients received heparin thromboprophylaxis, which was increased to the anticoagulation dose with D-dimer greater than 3µg/mL.
A total of 127 patients were followed up, of whom 73 underwent pulmonary computed tomography angiography (mean age, 54 ± 12 years; 49 men). Sixty-two of the 73 patients (84.9%) received full anticoagulation before computed tomography angiography. In addition, 18 of the 73 patients had pulmonary embolism (24.7%). When comparing patients with and without pulmonary embolism, no significant differences were observed in age, sex, obesity, smoking, Wells and revised Geneva scores, D-dimer or mortality. Anticoagulant use was similar in both groups. Days from the start of anticoagulation until computed tomography angiography were significantly lower in the pulmonary embolism group (p = 0.002). Three patients presented post contrast-acute kidney injury (4.1%), and one patient had major bleeding.
Despite anticoagulation, one in four COVID-19 patients connected to mechanical ventilation and evaluated with pulmonary computed tomography angiography had pulmonary embolism. With a longer the delay in performing computed tomography angiography once empirical anticoagulation was started, significantly less pulmonary embolism was identified.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):237-246
DOI 10.1590/S0103-507X2009000300002
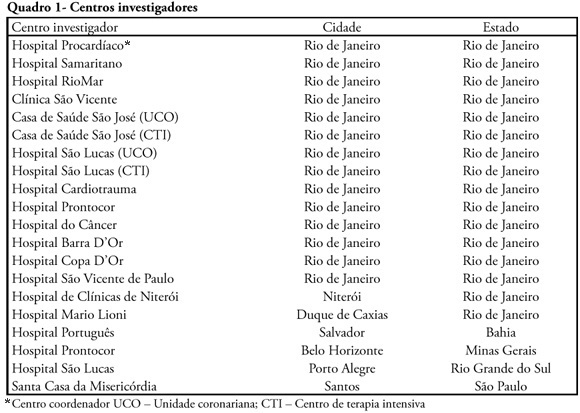
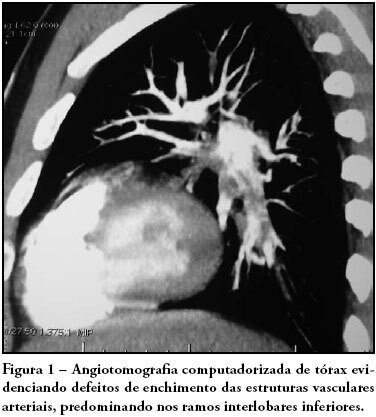
INTRODUCTION: The clinical profile as well as the therapeutic and diagnostic strategies for patients with pulmonary embolism, describes clinical practice in the approach of the disease. Such information, scarce in national studies, enables a better understanding of pulmonary embolism. METHODS: A multicenter trial included 727 patients with pulmonary embolism who were admitted in emergency or intensive care unit. Diagnostic criteria for inclusion were: 1. Visibility of thrombus in the pulmonary artery at pulmonary arteriography, helical computer tomography, magnetic resonance or echocardiogram. 2. High probability at pulmonary scintigraphy. 3. Venous duplex-scan with thrombus and clinical manifestations of pulmonary embolism. Clinical and complementary exams were analyzed. RESULTS: Mean age was 68 years, 42% were male. Most prevalent risk factors were: age>40 years, bed rest and neoplasm. More frequent signs and symptoms were: dyspnea, tachypnea, sinus tachycardia, and chest pain. Changes were observed at electrocardiogram in 30%, at chest X-ray in 45%, at venous duplex-scan in 67%, at transthoracic echocardiogram in 37%. . D-dimer, troponin I and CKMB were positive in, respectively, 93, 9 and 8%. Most frequently used methods to confirm diagnosis were helical computer tomography and non-fractioned heparin was the treatment most used. In-hospital mortality was 19.5%. CONCLUSIONS: It was observed that age>40 years, prolonged rest and neoplasms were the most prevalent risk factors and dyspnea and tachypnea were the more frequent clinical manifestations. Helical computer tomography was the most often used method to confirm diagnosis and non-fractioned heparin was the main form of treatment.
Abstract
Rev Bras Ter Intensiva. 2008;20(3):318-320
DOI 10.1590/S0103-507X2008000300016
Pulmonary thromboembolism is a major cause of morbidity and mortality of patients undergoing neurosurgical procedures. The purpose of this study was to present a case of intra-arterial pulmonary thrombolysis in recent neurosurgery postoperative period. Male patient, undergoing neurosurgery, presented as a complication on the seventh day of postoperative massive pulmonary embolism with hemodynamic instability and intraarterial pulmonary thrombolysis with alteplase was indicated. Evolution was satisfactory without bleeding complications and patient was discharged. Pulmonary thromboembolism is a high morbidity and mortality condition at neurosurgical postoperative period and thrombolysis should be an alternative therapy in cases refractory to clinical treatment.
Abstract
Rev Bras Ter Intensiva. 2006;18(3):316-319
DOI 10.1590/S0103-507X2006000300016
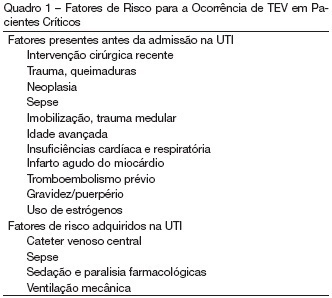
BACKGROUND AND OBJECTIVES: Venous thromboembolism (VTE), with includes deep vein thrombosis (DVT) and pulmonary embolism (PE), is a common complication in critically ill patients, resulting in high morbidity and mortality. CONTENTS: Most patients treated in intensive care units (ICU) face a high risk of thromboembolic complications. Despite these considerations, the prevention of VTE may not be as high a priority in ICU patients as it is in other high-risk patient groups. Low molecular weight heparin (LMWH) may be the optimal prophylaxis in most ICU patients, but there is a lack of sufficient data including the paucity of VTE consensus and guidelines documents pertaining to critically ill patients. CONCLUSIONS: This article reviews background, current options, and recommendations regarding VTE in intensive care population emphasizing special diagnostic and treatment considerations in the ICU setting.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (115) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)