Abstract
Rev Bras Ter Intensiva. 2021;33(3):346-352
DOI 10.5935/0103-507X.20210053
To assess pulmonary embolism incidence, its relationship with D-dimer levels and other possible associated factors in addition to anticoagulation and contrast medium adverse effects.
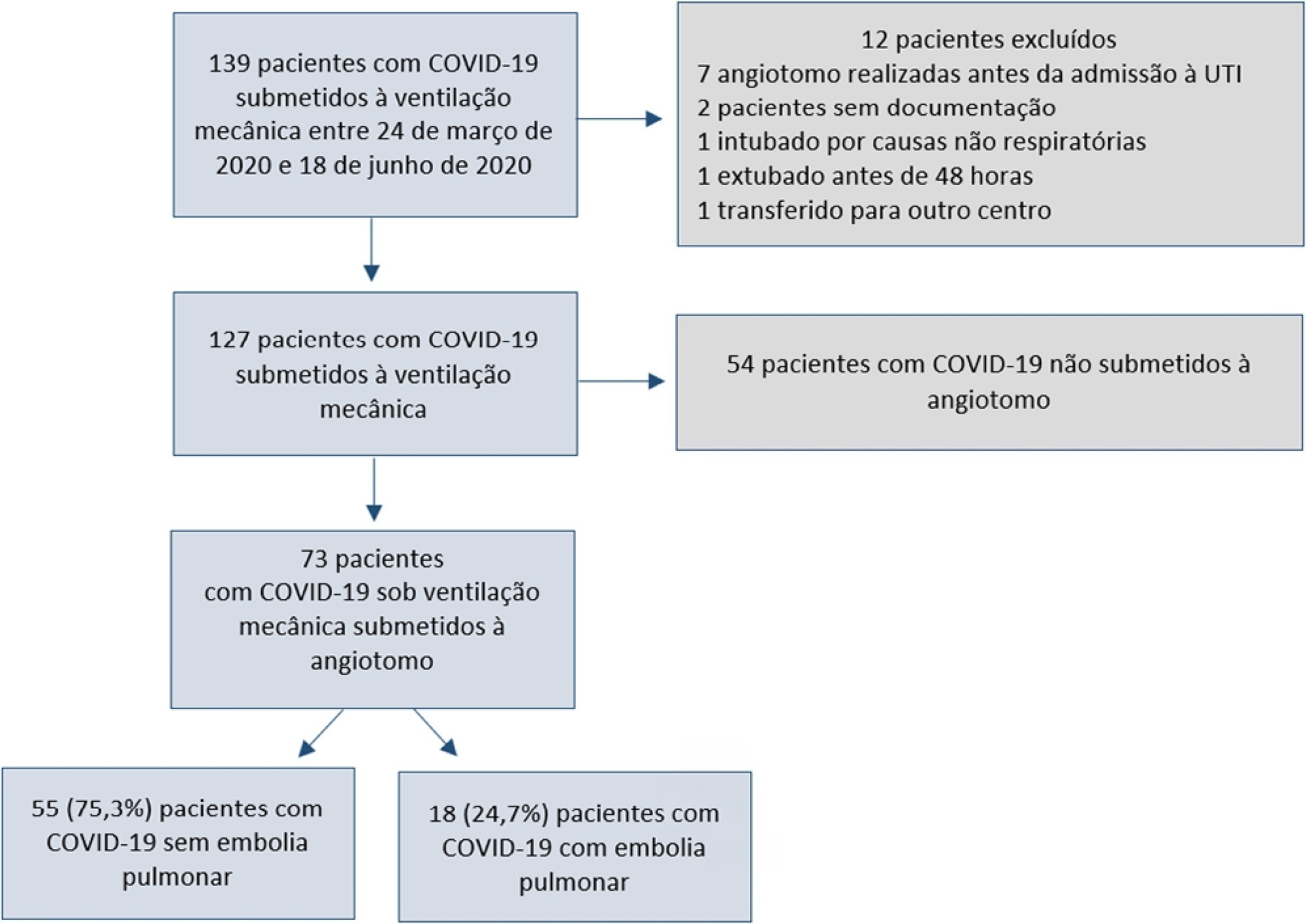
A retrospective observational cohort study at a Chilean public hospital was performed. Intensive care unit mechanically ventilated COVID-19 patients older than 18 years old between March and June 2020 were included. All patients received heparin thromboprophylaxis, which was increased to the anticoagulation dose with D-dimer greater than 3µg/mL.
A total of 127 patients were followed up, of whom 73 underwent pulmonary computed tomography angiography (mean age, 54 ± 12 years; 49 men). Sixty-two of the 73 patients (84.9%) received full anticoagulation before computed tomography angiography. In addition, 18 of the 73 patients had pulmonary embolism (24.7%). When comparing patients with and without pulmonary embolism, no significant differences were observed in age, sex, obesity, smoking, Wells and revised Geneva scores, D-dimer or mortality. Anticoagulant use was similar in both groups. Days from the start of anticoagulation until computed tomography angiography were significantly lower in the pulmonary embolism group (p = 0.002). Three patients presented post contrast-acute kidney injury (4.1%), and one patient had major bleeding.
Despite anticoagulation, one in four COVID-19 patients connected to mechanical ventilation and evaluated with pulmonary computed tomography angiography had pulmonary embolism. With a longer the delay in performing computed tomography angiography once empirical anticoagulation was started, significantly less pulmonary embolism was identified.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):331-335
DOI 10.5935/0103-507X.20210043
A 37-year-old woman (35 weeks pregnant) was admitted to a local hospital due to severe epistaxis resulting in shock and the need for emergency cesarean section. After failure to tamponade the bleeding, angiographic treatment was provided. After the procedure, she was admitted to the neurocritical intensive care unit and was confused and agitated, requiring sedation and endotracheal intubation. In the intensive care unit, diagnostic investigations included brain magnetic resonance imaging, lumbar puncture with viral panel, electroencephalogram, tests for autoimmunity, and hydroelectrolytic and metabolic evaluations. Magnetic resonance imaging showed a puntiform restricted diffusion area on the left corona radiata on diffusion weighted imaging and mild cortical posterior edema (without restricted diffusion), and an electroencephalogram showed moderate diffuse slow activity and fronto-temporal slow activity of the left hemisphere with associated scarce paroxysmal components. The other exams did not show any relevant alterations. Due to the temporal relationship, the clinical history and the magnetic resonance imaging results, a diagnosis of contrast-induced encephalopathy was made. After 2 days in the intensive care unit, sedation was withdrawn, the patient was extubated, and total neurological recovery was verified within the next 24 hours.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):303-309
DOI 10.5935/0103-507X.20170041
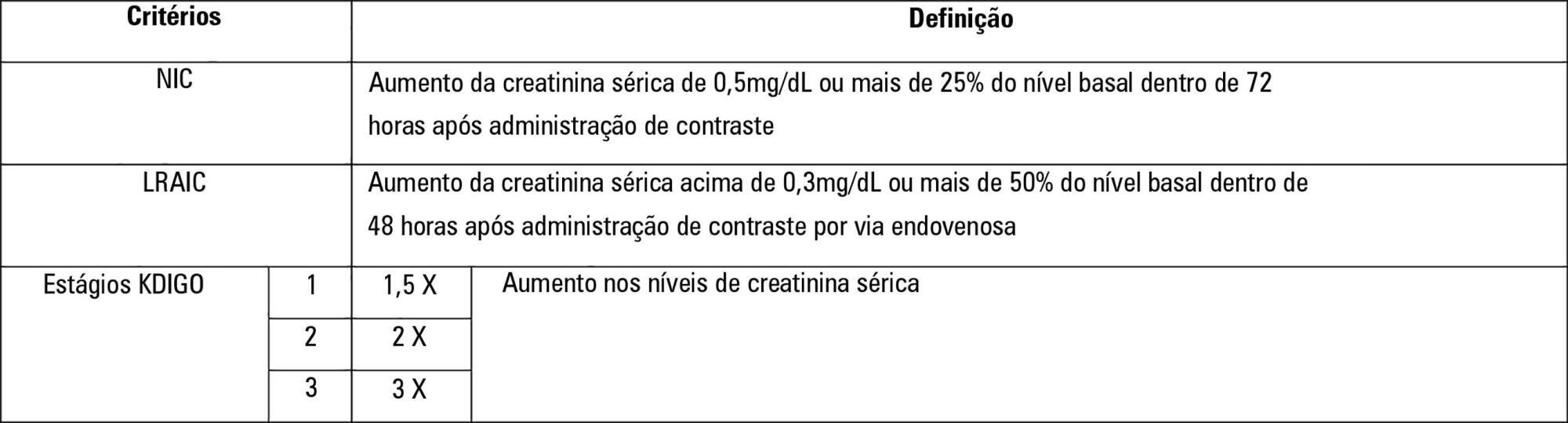
To establish whether there is superiority between contrast-induced acute kidney injury and contrast-induced nephropathy criteria as predictors of unfavorable clinical outcomes.
Retrospective study carried out in a tertiary hospital with 157 patients undergoing radiocontrast infusion for propaedeutic purposes.
One hundred forty patients fulfilled the inclusion criteria: patients who met the criteria for contrast-induced acute kidney injury (59) also met the criteria for contrast-induced nephropathy (76), 44.3% met the criteria for KDIGO staging, 6.4% of the patients required renal replacement therapy, and 10.7% died.
The diagnosis of contrast-induced nephropathy was the most sensitive criterion for renal replacement therapy and death, whereas KDIGO showed the highest specificity; there was no correlation between contrast volume and progression to contrast-induced acute kidney injury, contrast-induced nephropathy, support dialysis or death in the assessed population.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)