You searched for:"Alberto Belenguer-Muncharaz"
We found (2) results for your search.-
Original Article
Protocol-directed weaning versus conventional weaning from mechanical ventilation for neurocritical patients in an intensive care unit: a nonrandomized quasi-experimental study
Crit Care Sci. 2023;35(1):44-56
Abstract
Original ArticleProtocol-directed weaning versus conventional weaning from mechanical ventilation for neurocritical patients in an intensive care unit: a nonrandomized quasi-experimental study
Crit Care Sci. 2023;35(1):44-56
DOI 10.5935/2965-2774.20230340-pt
Views8ABSTRACT
Objective:
To investigate whether protocol-directed weaning in neurocritical patients would reduce the rate of extubation failure (as a primary outcome) and the associated complications (as a secondary outcome) compared with conventional weaning.
Methods:
A quasi-experimental study was conducted in a medical-surgical intensive care unit from January 2016 to December 2018. Patients aged 18 years or older with an acute neurological disease who were on mechanical ventilation > 24 hours were included. All patients included in the study were ready to wean, with no or minimal sedation, Glasgow coma score ≥ 9, spontaneous ventilatory stimulus, noradrenaline ≤ 0.2μgr/kg/ minute, fraction of inspired oxygen ≤ 0.5, positive end-expiratory pressure ≤ 5cmH2O, maximal inspiratory pressure < -20cmH2O, and occlusion pressure < 6cmH2O.
Results:
Ninety-four of 314 patients admitted to the intensive care unit were included (50 in the Intervention Group and 44 in the Control Group). There was no significant difference in spontaneous breathing trial failure (18% in the Intervention Group versus 34% in the Control Group, p = 0.12). More patients in the Intervention Group were extubated than in the Control Group (100% versus 79%, p = 0.01). The rate of extubation failure was not signifiantly diffrent between the groups (18% in the Intervention Group versus 17% in the Control Group; relative risk 1.02; 95%CI 0.64 – 1.61; p = 1.00). The reintubation rate was lower in the Control Group (16% in the Intervention Group versus 11% in the Control Group; relative risk 1.15; 95%CI 0.74 – 1.82; p = 0.75). The need for tracheotomy was lower in the Intervention Group [4 (8%) versus 11 (25%) in the Control Group; relative risk 0.32; 95%CI 0.11 – 0.93; p = 0.04]. At Day 28, the patients in the Intervention Group had more ventilator-free days than those in the Control Group [28 (26 – 28) days versus 26 (19 – 28) days; p = 0.01]. The total duration of mechanical ventilation was shorter in the Intervention Group than in the Control Group [5 (2 – 13) days versus 9 (3 – 22) days; p = 0.01]. There were no diffrences in the length of intensive care unit stay, 28-day free from mechanical ventilation, hospital stay or 90-day mortality.
Conclusion:
Considering the limitations of our study, the application of a weaning protocol for neurocritical patients led to a high percentage of extubation, a reduced need for tracheotomy and a shortened duration of mechanical ventilation. However, there was no reduction in extubation failure or the 28-day free of from mechanical ventilation compared with the Control Group.
Keywords:Airway extubation, WeaningCritical illnessRespiration, artificialTracheotomyVentilator weaningSee more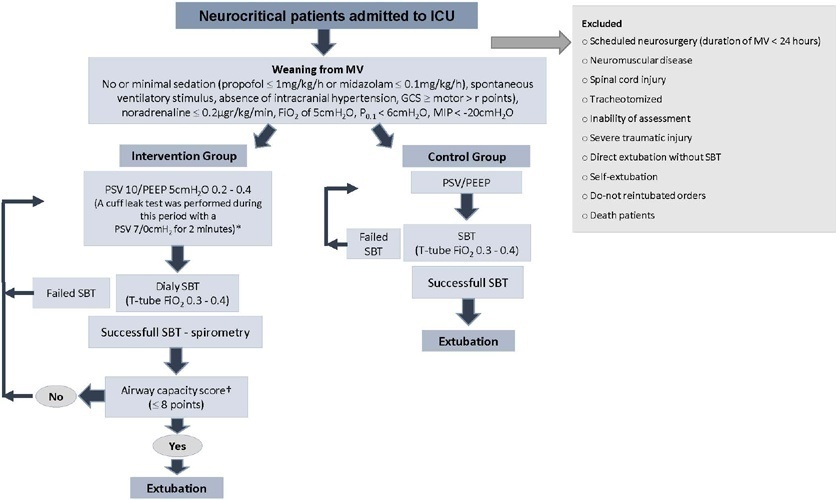
-
Original Article
Noninvasive ventilation versus conventional oxygen therapy after extubation failure in high-risk patients in an intensive care unit: a pragmatic clinical trial
Rev Bras Ter Intensiva. 2021;33(3):362-373
Abstract
Original ArticleNoninvasive ventilation versus conventional oxygen therapy after extubation failure in high-risk patients in an intensive care unit: a pragmatic clinical trial
Rev Bras Ter Intensiva. 2021;33(3):362-373
DOI 10.5935/0103-507X.20210059
Views1ABSTRACT
Objective:
To determine the effectiveness of noninvasive ventilation versus conventional oxygen therapy in patients with acute respiratory failure after extubation failure.
Methods:
A pragmatic clinical trial was conducted in an intensive care unit from March 2009 to September 2016. Patients on mechanical ventilation > 24 hours who developed acute respiratory failure after scheduled extubation were included and were assigned to noninvasive ventilation or conventional oxygen therapy. The primary objective was to reduce the reintubation rate. The secondary objectives were to improve respiratory parameters and reduce complications, the duration of mechanical ventilation, the intensive care unit stay, the hospital stay, and mortality in the intensive care unit, in the hospital, and 90 days after discharge. Factors correlated with reintubation were also analyzed.
Results:
Of a total of 2,574 patients, 77 were analyzed (38 in the noninvasive ventilation group and 39 in the conventional oxygen therapy group). Noninvasive ventilation reduced the respiratory and cardiac rates more rapidly than conventional oxygen therapy. Reintubation was less common in the noninvasive ventilation group [12 (32%) versus 22 (56%) in the conventional oxygen therapy group, relative risk 0.58 (95%CI 0.34 – 0.97), p = 0.039]. The rest of the parameters did not show significant differences. In the multivariate analysis, noninvasive ventilation protected against reintubation [OR 0.17 (95%CI 0.05 – 0.56), p = 0.004], while liver failure before extubation and the inability to maintain airway patency predisposed patients to reintubation.
Conclusion:
The use of noninvasive ventilation in patients who failed extubation could be beneficial compared to conventional oxygen therapy.
Keywords:extubationNoninvasive ventilationOxygen inhalation therapyRespiration, artificialRespiratory insufficiencyWeaningSee more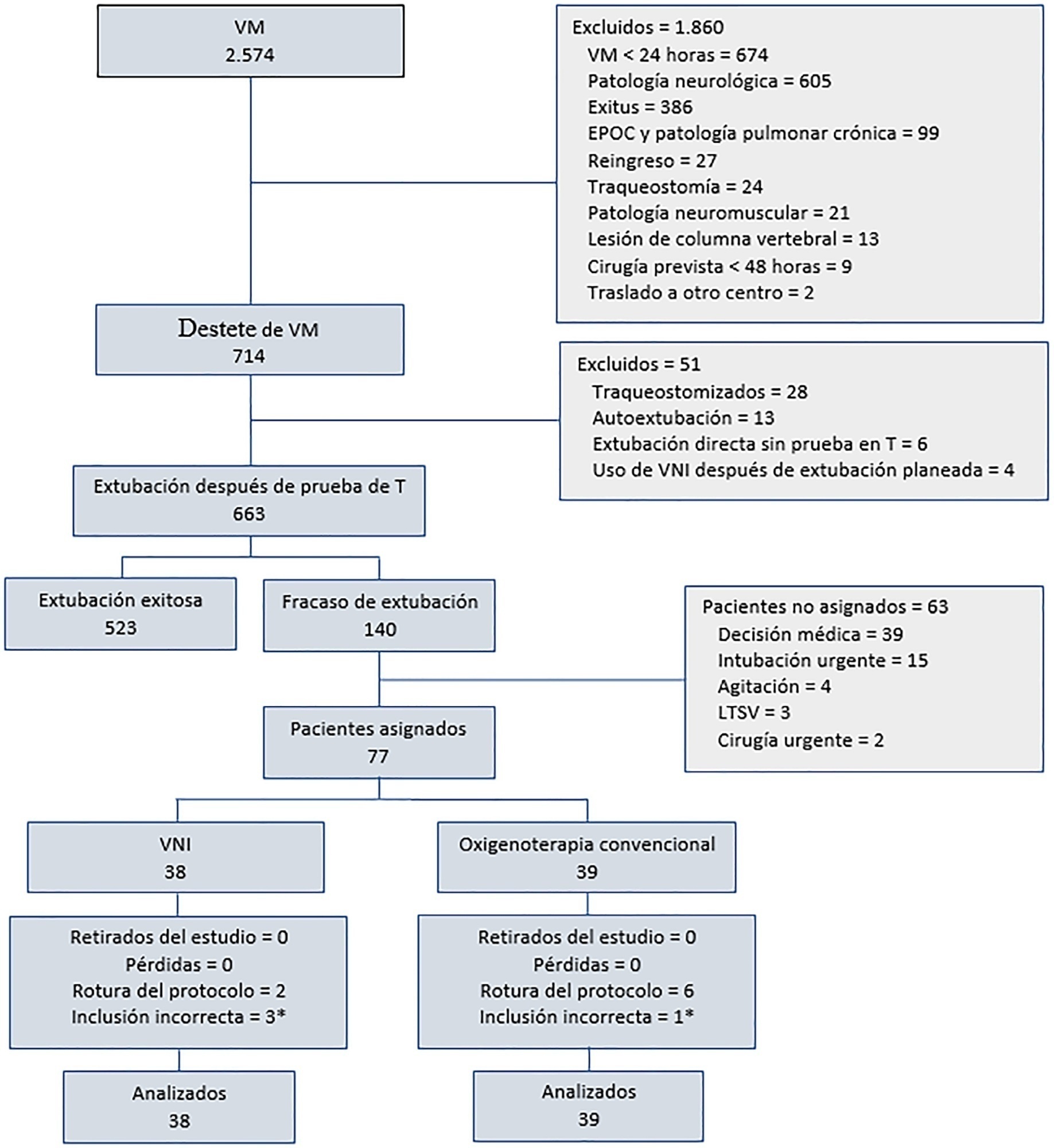
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




