Abstract
Crit Care Sci. 2023;35(1):44-56
DOI 10.5935/2965-2774.20230340-pt
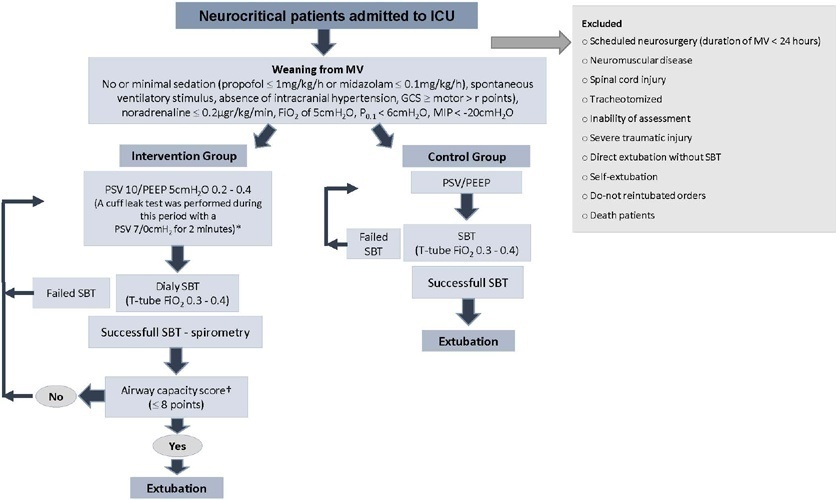
To investigate whether protocol-directed weaning in neurocritical patients would reduce the rate of extubation failure (as a primary outcome) and the associated complications (as a secondary outcome) compared with conventional weaning.
A quasi-experimental study was conducted in a medical-surgical intensive care unit from January 2016 to December 2018. Patients aged 18 years or older with an acute neurological disease who were on mechanical ventilation > 24 hours were included. All patients included in the study were ready to wean, with no or minimal sedation, Glasgow coma score ≥ 9, spontaneous ventilatory stimulus, noradrenaline ≤ 0.2μgr/kg/ minute, fraction of inspired oxygen ≤ 0.5, positive end-expiratory pressure ≤ 5cmH2O, maximal inspiratory pressure < -20cmH2O, and occlusion pressure < 6cmH2O.
Ninety-four of 314 patients admitted to the intensive care unit were included (50 in the Intervention Group and 44 in the Control Group). There was no significant difference in spontaneous breathing trial failure (18% in the Intervention Group versus 34% in the Control Group, p = 0.12). More patients in the Intervention Group were extubated than in the Control Group (100% versus 79%, p = 0.01). The rate of extubation failure was not signifiantly diffrent between the groups (18% in the Intervention Group versus 17% in the Control Group; relative risk 1.02; 95%CI 0.64 - 1.61; p = 1.00). The reintubation rate was lower in the Control Group (16% in the Intervention Group versus 11% in the Control Group; relative risk 1.15; 95%CI 0.74 - 1.82; p = 0.75). The need for tracheotomy was lower in the Intervention Group [4 (8%) versus 11 (25%) in the Control Group; relative risk 0.32; 95%CI 0.11 - 0.93; p = 0.04]. At Day 28, the patients in the Intervention Group had more ventilator-free days than those in the Control Group [28 (26 - 28) days versus 26 (19 - 28) days; p = 0.01]. The total duration of mechanical ventilation was shorter in the Intervention Group than in the Control Group [5 (2 - 13) days versus 9 (3 - 22) days; p = 0.01]. There were no diffrences in the length of intensive care unit stay, 28-day free from mechanical ventilation, hospital stay or 90-day mortality.
Considering the limitations of our study, the application of a weaning protocol for neurocritical patients led to a high percentage of extubation, a reduced need for tracheotomy and a shortened duration of mechanical ventilation. However, there was no reduction in extubation failure or the 28-day free of from mechanical ventilation compared with the Control Group.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):87-95
DOI 10.5935/0103-507X.20170013
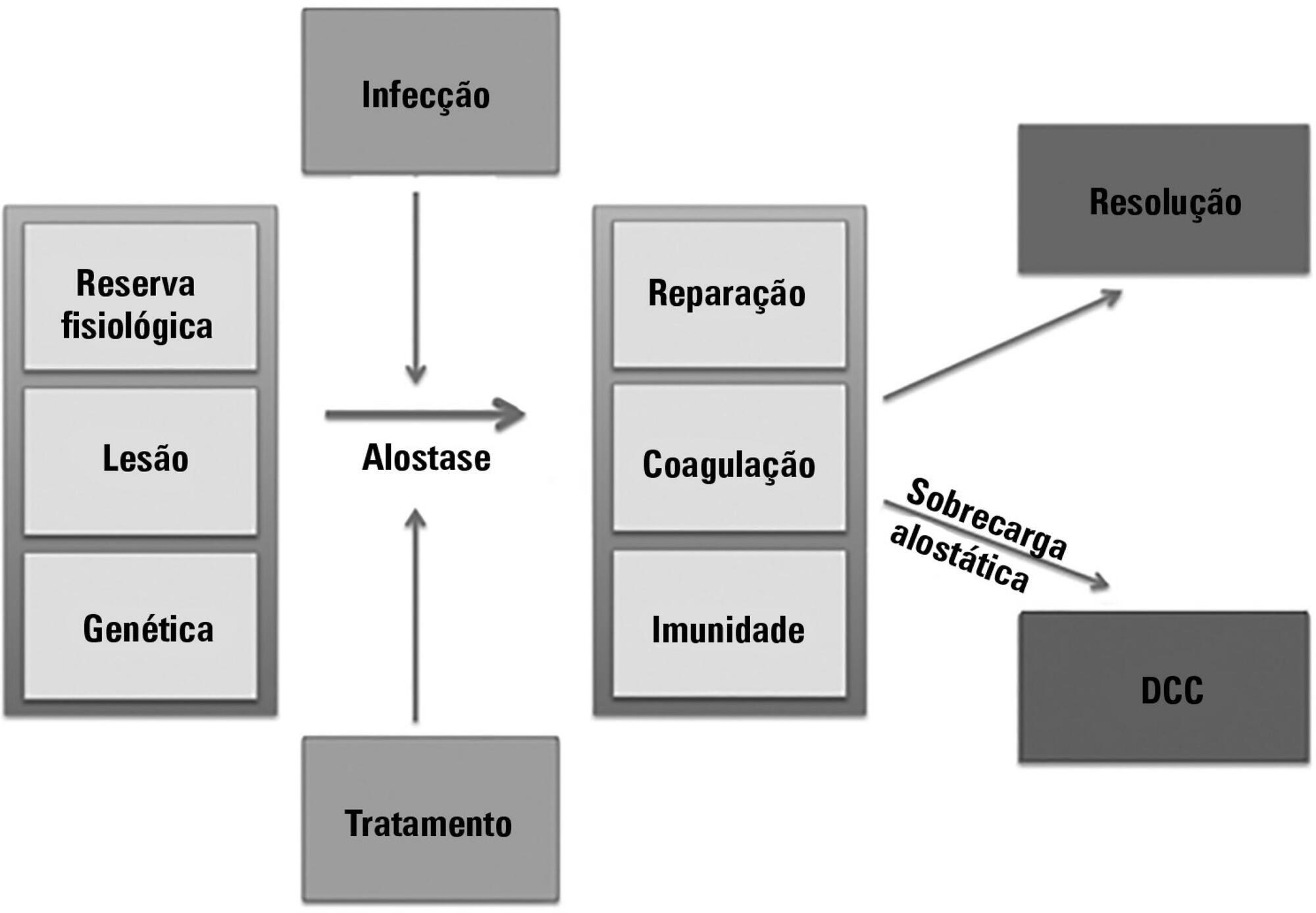
The technological advancements that allow support for organ dysfunction have led to an increase in survival rates for the most critically ill patients. Some of these patients survive the initial acute critical condition but continue to suffer from organ dysfunction and remain in an inflammatory state for long periods of time. This group of critically ill patients has been described since the 1980s and has had different diagnostic criteria over the years. These patients are known to have lengthy hospital stays, undergo significant alterations in muscle and bone metabolism, show immunodeficiency, consume substantial health resources, have reduced functional and cognitive capacity after discharge, create a sizable workload for caregivers, and present high long-term mortality rates. The aim of this review is to report on the most current evidence in terms of the definition, pathophysiology, clinical manifestations, treatment, and prognosis of persistent critical illness.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):167-172
DOI 10.1590/S0103-507X2012000200012
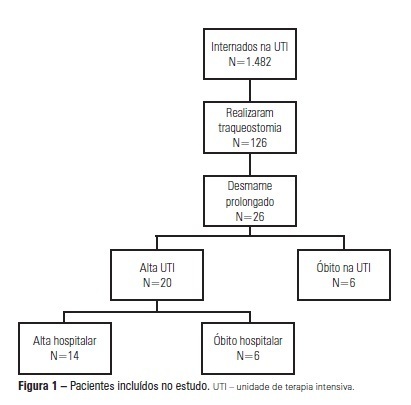
OBJECTIVE: We aimed to assess the use of noninvasive ventilation devices in patients with prolonged weaning following tracheotomy. METHODS: We performed a retrospective observational study using data collected from the clinical records of tracheotomized patients diagnosed with prolonged weaning. The participants were hospitalized in the adult intensive care unit of Moinhos de Vento Hospital, Porto Alegre (RS) between December 2007 and December 2008. RESULTS: In the data collection period, 1,482 patients were admitted to the intensive care unit. In total, 126 patients underwent tracheotomies, and 26 of these patients met the inclusion criteria for participating in the study. The average age of the patients in our sample was 73 ± 12 years. In our sample, 57.7% of the participants were female, and 80.8% were admitted as a result of acute hypoxemic respiratory failure. After the tracheotomy, the patients remained under mechanical ventilation for an average of 29.8 days. After the initiation of the experimental protocol, the tracheotomized patients remained under ventilation for an average of 53.5 days on a portable noninvasive device connected to the tracheotomy. There were three possible outcomes for the patients. They were discharged, were weaned from the noninvasive ventilation, or died in the intensive care unit or hospital ward. In total, 76.9% (20/26) of the patients were discharged from the intensive care unit, and 53.8% (14/26) of the patients were discharged from the hospital. CONCLUSION: The use of noninvasive portable ventilators connected to the tracheotomy may represent an alternative for discontinuing ventilationand discharging tracheotomized patients with prolonged ventilatory weaning from intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2007;19(3):317-321
DOI 10.1590/S0103-507X2007000300008
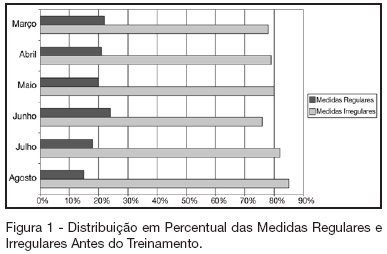
BACKGROUND AND OBJECTIVES: The tube cuff pressure directly transmitted on the tracheal wall in an irregular form can cause injuries and lead to bronchoaspiration. The aim of this study was to demonstrate that the implementation of routine tube cuff pressure measurements result in a reliable control to maintain the measurements within the parameters considered safe, thus preventing the described complications. METHODS: A total of 3,195 tube cuff measurements were obtained from 1,194 male and female patients admitted at the Intensive Care Unit (ICU) and Coronary Unit (CU), who were undergoing mechanical ventilation with endotracheal prosthesis and tracheotomy cannula, during the morning and afternoon periods. RESULTS: From March to August 2005 the follow-up of the measurements obtained by the physical therapy professionals was carried out and it was observed that the measurements were irregular, on average, in 80% of the cases. Thus, a training program was established, which was focused on the Nursing Teams of the ICU and CU, consisting in providing directions for the adequate procedures performed at the bedside (in loco training). The training procedures were carried out at two different periods (morning and afternoon) in order to include the whole team. CONCLUSIONS: It is suggested that it is necessary to monitor tube cuff pressure through the implementation of routine measurements in the morning, afternoon and evening periods as a prophylactic measure, in order to prevent the possible complications of tracheal prosthesis balloon pressure.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)