You searched for:"Oellen Stuani Franzosi"
We found (4) results for your search.-
Original Article
SAPS 3 in the modified NUTrition RIsk in the Critically ill score has comparable predictive accuracy to APACHE II as a severity marker
Rev Bras Ter Intensiva. 2021;33(3):394-400
Abstract
Original ArticleSAPS 3 in the modified NUTrition RIsk in the Critically ill score has comparable predictive accuracy to APACHE II as a severity marker
Rev Bras Ter Intensiva. 2021;33(3):394-400
DOI 10.5935/0103-507X.20210064
Views2ABSTRACT
Objective:
To evaluate the substitution of Acute Physiology and Chronic Health Evaluation II (APACHE II) by Simplified Acute Physiology Score 3 (SAPS 3) as a severity marker in the modified version of the NUTrition RIsk in the Critically ill score (mNUTRIC); without interleukin 6) based on an analysis of its discriminative ability for in-hospital mortality prediction.
Methods:
This retrospective cohort study evaluated 1,516 adult patients admitted to an intensive care unit of a private general hospital from April 2017 to January 2018. Performance evaluation included Fleiss’ Kappa and Pearson correlation analysis. The discriminative ability for estimating in-hospital mortality was assessed with the Receiver Operating Characteristic curve.
Results:
The sample was randomly divided into two-thirds for model development (n = 1,025; age 72 [57 – 83]; 52.4% male) and one-third for performance evaluation (n = 490; age 72 [57 – 83]; 50.8% male). The agreement with mNUTRIC was Kappa of 0.563 (p < 0.001), and the correlation between the instruments was Pearson correlation of 0.804 (p < 0.001). The tool showed good performance in predicting in-hospital mortality (area under the curve 0.825 [0.787 - 0.863] p < 0.001).
Conclusion:
The substitution of APACHE II by SAPS 3 as a severity marker in the mNUTRIC score showed good performance in predicting in-hospital mortality. These data provide the first evidence regarding the validity of the substitution of APACHE II by SAPS 3 in the mNUTRIC as a marker of severity. Multicentric studies and additional analyses of nutritional adequacy parameters are required.
Keywords:APACHECritical careMortalitynutritional assessmentSeverity of illness indexSimplified acute physiology scoreSee more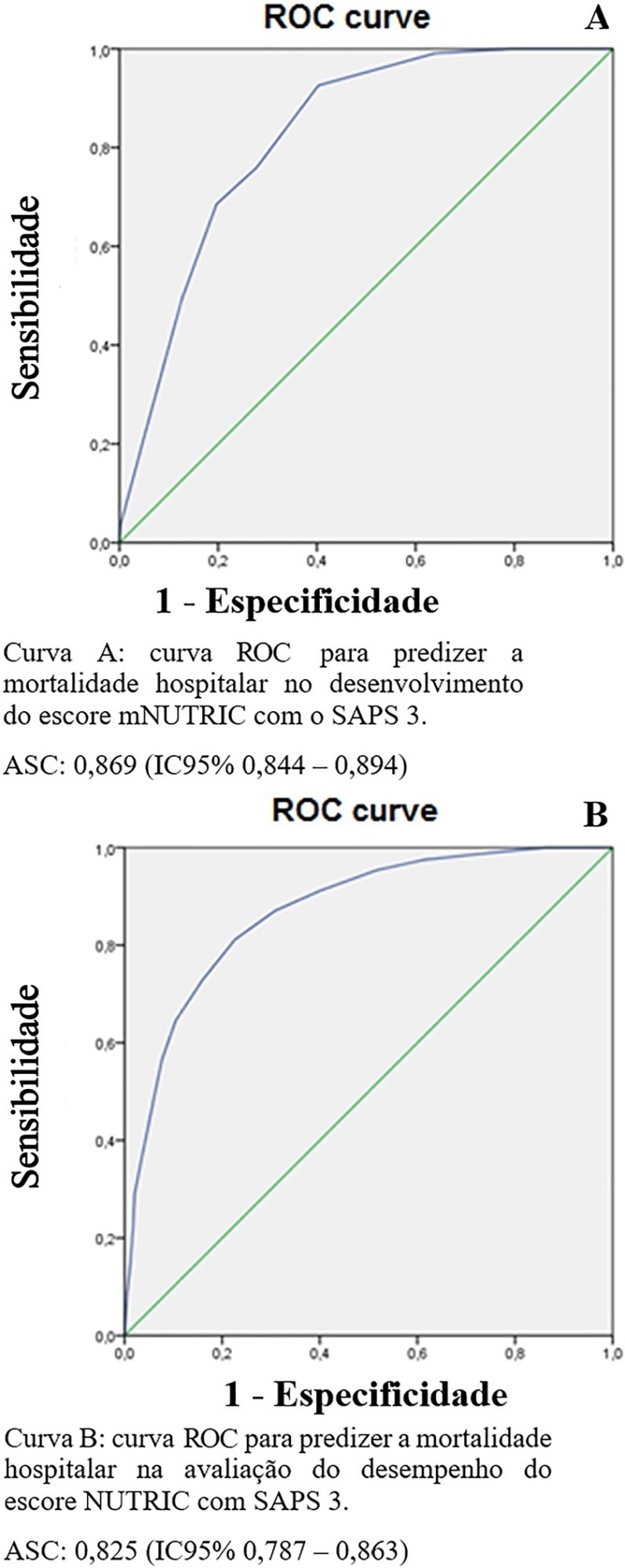
-
Original Articles
High nutritional risk is associated with unfavorable outcomes in patients admitted to an intensive care unit
Rev Bras Ter Intensiva. 2019;31(3):326-332
Abstract
Original ArticlesHigh nutritional risk is associated with unfavorable outcomes in patients admitted to an intensive care unit
Rev Bras Ter Intensiva. 2019;31(3):326-332
DOI 10.5935/0103-507X.20190041
Views1See moreABSTRACT
Objective:
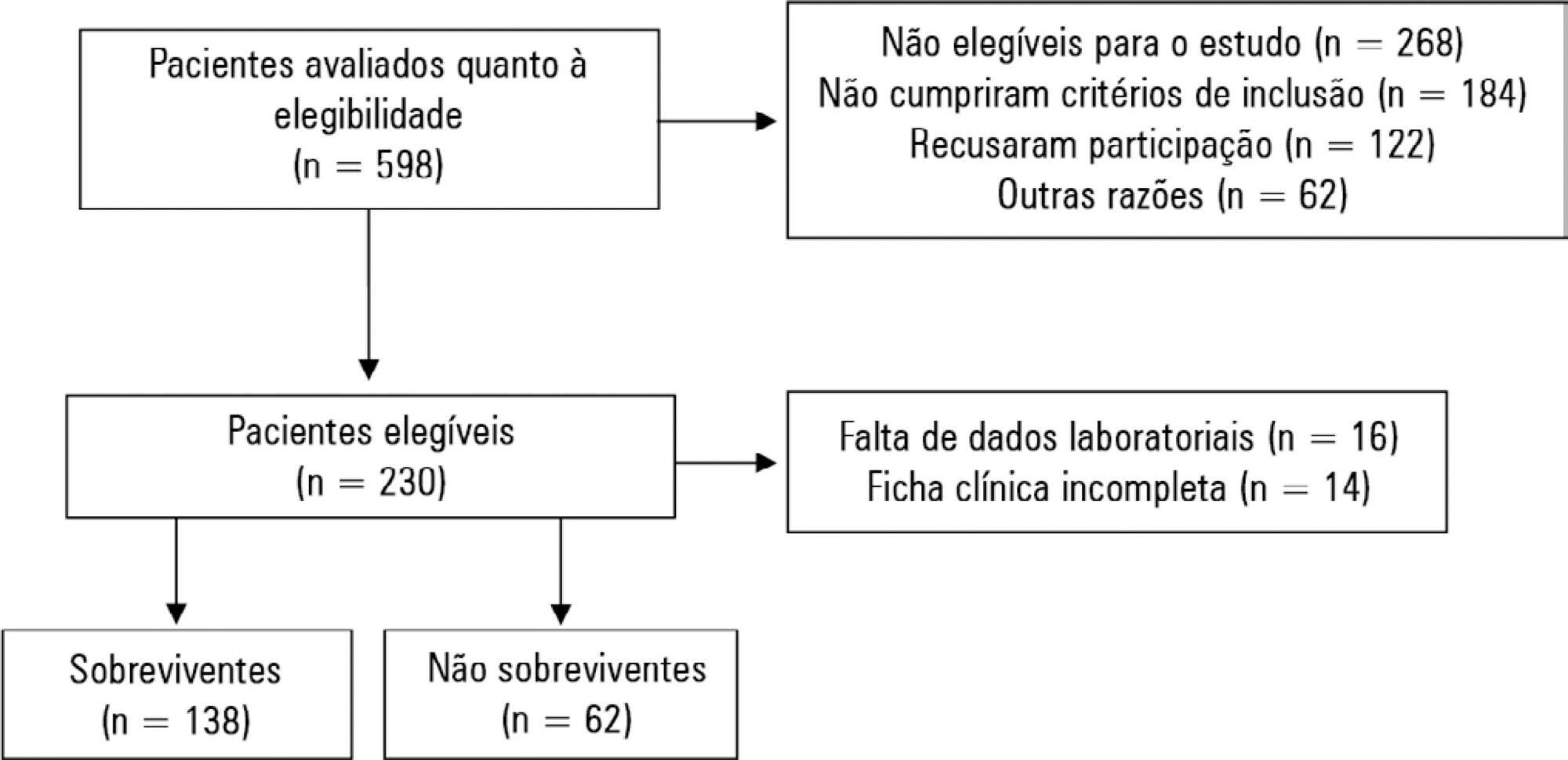
To evaluate possible associations between nutritional risk and the clinical outcomes of critical patients admitted to an intensive care unit.
Methods:
A prospective study was carried out with a cohort comprising 200 patients admitted to a university hospital intensive care unit. Nutritional risk was assessed with the NRS-2002 and NUTRIC scores. Patients with scores ≥ 5 were considered at high nutritional risk. Clinical data and outcome measures were obtained from patients’ medical records. Multiple logistic regression analysis was used to calculate odds ratios and their respective 95% confidence intervals (for clinical outcomes).
Results:
This sample of critical patients had a mean age of 59.4 ± 16.5 years and 53.5% were female. The proportions at high nutritional risk according to NRS-2002 and NUTRIC were 55% and 36.5%, respectively. Multiple logistic regression models adjusted for gender and type of admission indicated that high nutritional risk assessed by the NRS-2002 was positively associated with use of mechanical ventilation (OR = 2.34; 95%CI 1.31 – 4.19; p = 0.004); presence of infection (OR = 2.21; 95%CI 1.24 – 3.94; p = 0.007), and death (OR = 1.86; 95%CI 1.01 – 3.41; p = 0.045). When evaluated by NUTRIC, nutritional risk was associated with renal replacement therapy (OR = 2.10; 95%CI 1.02 – 4.15; p = 0.040) and death (OR = 3.48; 95%CI 1.88 – 6.44; p < 0.001).
Conclusion:
In critically ill patients, high nutritional risk was positively associated with an increased risk of clinical outcomes including hospital death.
-
Review Articles
Chronic critical illness: are we saving patients or creating victims?
Rev Bras Ter Intensiva. 2017;29(1):87-95
Abstract
Review ArticlesChronic critical illness: are we saving patients or creating victims?
Rev Bras Ter Intensiva. 2017;29(1):87-95
DOI 10.5935/0103-507X.20170013
Views1See moreABSTRACT
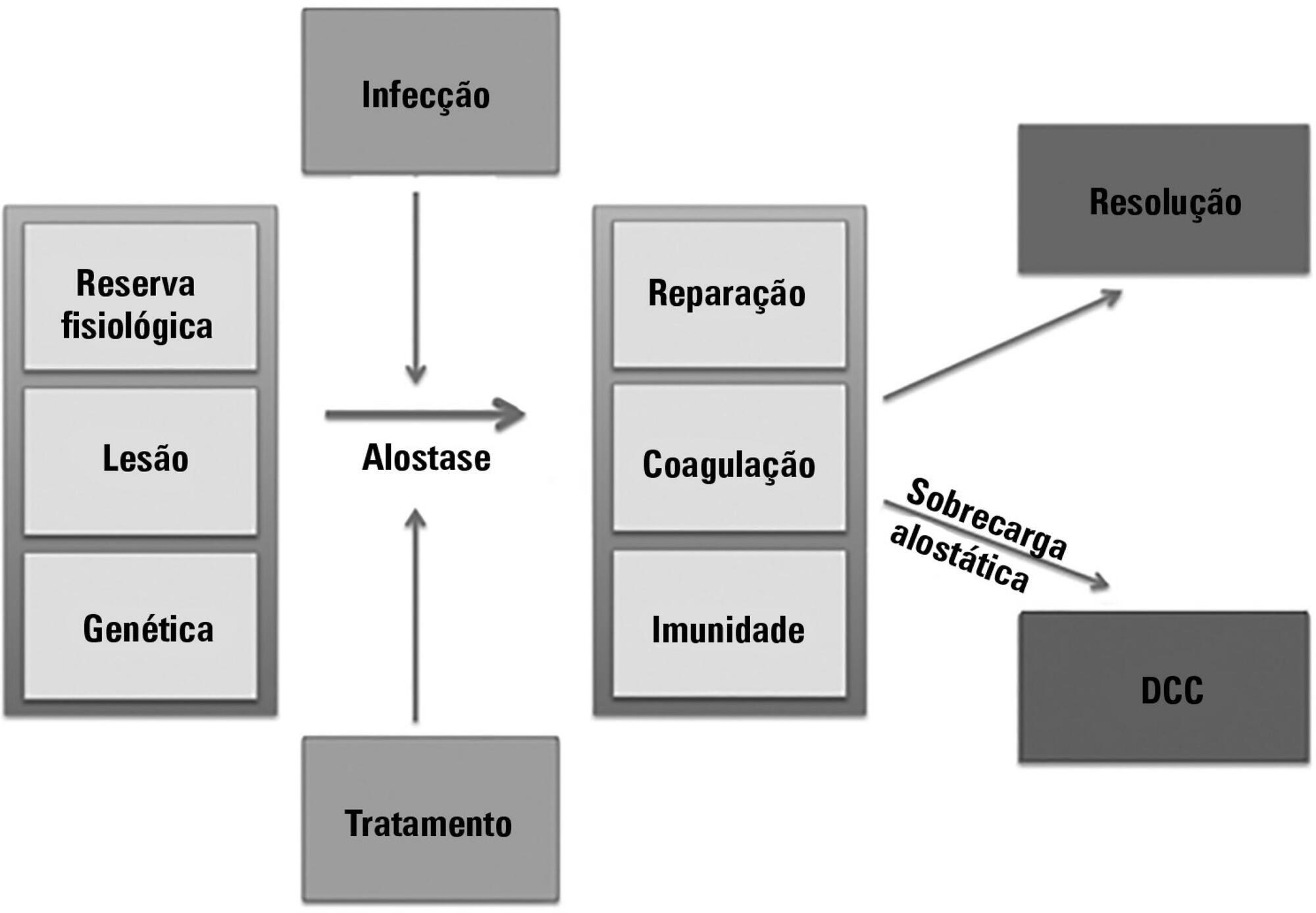
The technological advancements that allow support for organ dysfunction have led to an increase in survival rates for the most critically ill patients. Some of these patients survive the initial acute critical condition but continue to suffer from organ dysfunction and remain in an inflammatory state for long periods of time. This group of critically ill patients has been described since the 1980s and has had different diagnostic criteria over the years. These patients are known to have lengthy hospital stays, undergo significant alterations in muscle and bone metabolism, show immunodeficiency, consume substantial health resources, have reduced functional and cognitive capacity after discharge, create a sizable workload for caregivers, and present high long-term mortality rates. The aim of this review is to report on the most current evidence in terms of the definition, pathophysiology, clinical manifestations, treatment, and prognosis of persistent critical illness.
-
Original Articles – Clinical Research
Nutritional support and outcomes in critically ill patients after one week in the intensive care unit
Rev Bras Ter Intensiva. 2012;24(3):263-269
Abstract
Original Articles – Clinical ResearchNutritional support and outcomes in critically ill patients after one week in the intensive care unit
Rev Bras Ter Intensiva. 2012;24(3):263-269
DOI 10.1590/S0103-507X2012000300010
Views1OBJECTIVE: This study evaluated the relationship between nutritional intake and protein and caloric requirements and observed clinical outcomes on the 7th day of intensive care unit stay. METHODS: This was a retrospective cohort study of 126 patients who were admitted to the intensive care unit for >7 days. The patients were categorized according to the adequacy of energy and protein intake in relation to requirements (a >60% Adequate Intake Group and a <60% Inadequate Intake Group). The length of stay, ventilator free time and mortality in the intensive care unit and hospital were evaluated. RESULTS: Enteral nutrition was used in 95.6% of the 126 included patients, and nutrition was initiated 41 hours after admission to the intensive care unit. The adequacy of intake was 84% for energy and 72.5% for protein. No differences in the length of stay [16 (11-23) versus 15 (11-21) days, p=0.862], ventilator free time [2 (0-7) versus 3 (0-6) days, p=0.985] or mortality in the intensive care unit [12 (41.4%) versus 38 (39.1%), p=0.831] and hospital [15 (51.7%) versus 44 (45.4%), p=0.348] were observed between the adequate and inadequate energy intake groups, respectively. Similar results in protein intake and the length of hospital stay [15 (12-21) versus 15 (11-21) days, p=0.996], ventilator free time [2 (0-7) versus 3 (0-6) days, p=0.846], and mortality in the intensive care unit [15 (28.3%) versus 35 (47.9%), p=0.536)] and hospital [18 (52.9%) versus 41 (44.6%), p=0.262] were observed between groups. CONCLUSION: The results did not establish that energy and protein intakes of greater or less than 60% of nutritional requirements were reliable dividers of clinical outcomes.
Keywords:Energy requirementIntensive care unitsLength of stayMortalitynutrition therapyRespiration, artificialSee more
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




