Abstract
Rev Bras Ter Intensiva. 2021;33(3):394-400
DOI 10.5935/0103-507X.20210064
To evaluate the substitution of Acute Physiology and Chronic Health Evaluation II (APACHE II) by Simplified Acute Physiology Score 3 (SAPS 3) as a severity marker in the modified version of the NUTrition RIsk in the Critically ill score (mNUTRIC); without interleukin 6) based on an analysis of its discriminative ability for in-hospital mortality prediction.
This retrospective cohort study evaluated 1,516 adult patients admitted to an intensive care unit of a private general hospital from April 2017 to January 2018. Performance evaluation included Fleiss’ Kappa and Pearson correlation analysis. The discriminative ability for estimating in-hospital mortality was assessed with the Receiver Operating Characteristic curve.
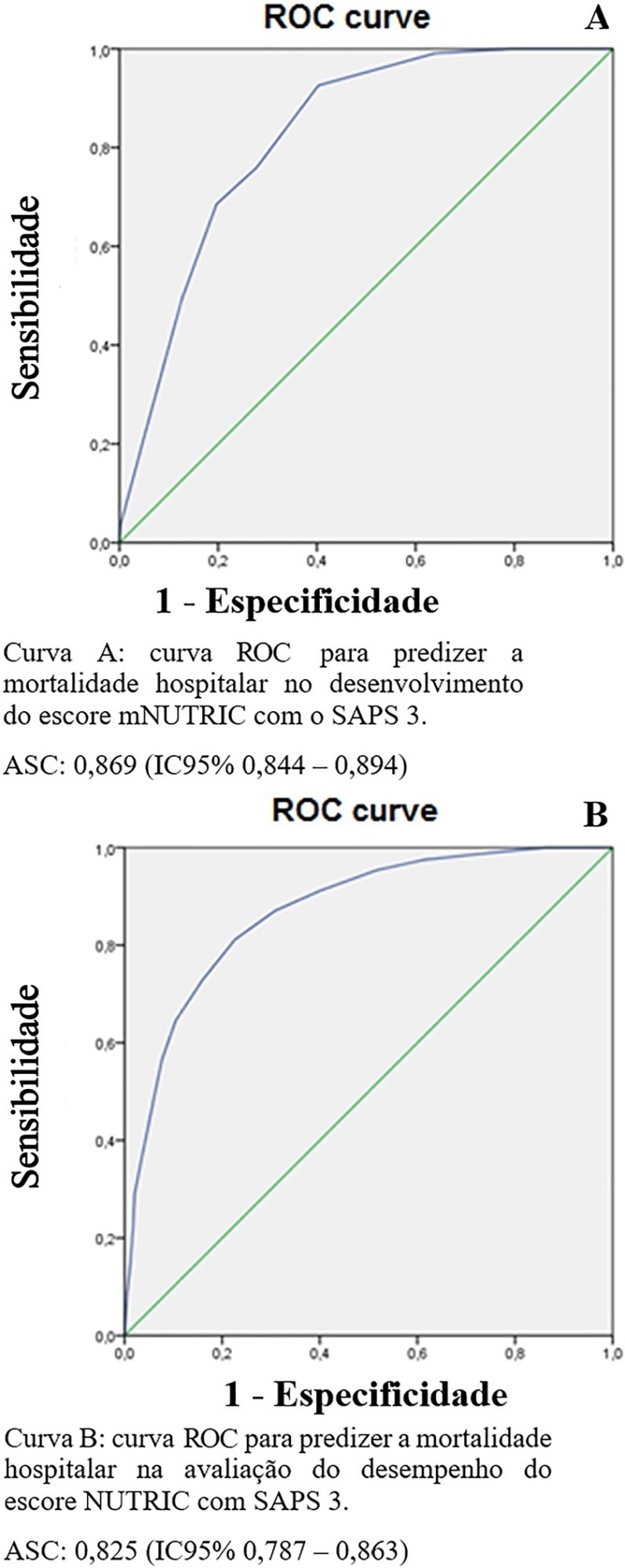
The sample was randomly divided into two-thirds for model development (n = 1,025; age 72 [57 - 83]; 52.4% male) and one-third for performance evaluation (n = 490; age 72 [57 - 83]; 50.8% male). The agreement with mNUTRIC was Kappa of 0.563 (p < 0.001), and the correlation between the instruments was Pearson correlation of 0.804 (p < 0.001). The tool showed good performance in predicting in-hospital mortality (area under the curve 0.825 [0.787 - 0.863] p < 0.001).
The substitution of APACHE II by SAPS 3 as a severity marker in the mNUTRIC score showed good performance in predicting in-hospital mortality. These data provide the first evidence regarding the validity of the substitution of APACHE II by SAPS 3 in the mNUTRIC as a marker of severity. Multicentric studies and additional analyses of nutritional adequacy parameters are required.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):133-137
DOI 10.1590/S0103-507X2010000200006
STUDY OBJECTIVE: Obese patients seem to have worse outcomes and more complications during intensive care unit (ICU) stay. This study describes the clinical course, complications and prognostic factors of obese patients admitted to an intensive care unit compared to a control group of nonobese patients. DESIGN: Retrospective observational study. SETTING: A 10-bed adult intensive care unit in a university-affiliated hospital. METHODS: All patients admitted to the intensive care unit over 52 months (April 01/2005 to November 30/2008) were included. Obese patients were defined as those with a body mass index (BMI) ≥ 30 Kg/M2. Demographic and intensive care unit related data were also collected. An clinical and demographical matching group of eutrophic patients selected from the data base as comparator for mortality and morbidity outcomes. The Mann-Whitney test was used for numeric data comparisons and the Chi Square test for categorical data comparisons. RESULTS: Two hundred nineteen patients were included. The obese group (n=73) was compared to the eutrophic group (n= 146). Most of this group BMI ranged between 30 - 35 Kg/M2. Only ten patients had body mass index ≥40 Kg/M2. Significant differences between the obese and eutrophic groups were observed in median APACHE II score (16 versus 12, respectively; p<0.05) and median intensive care unit length of stay (7 versus 5 days respectively; p<0,05). No significant differences were seen regarding risk of death, mortality rate, mechanical ventilation needs, days free of mechanical ventilation and tracheostomy rates. The observed mortality was higher than the APACHE II-predicted for both groups, but the larger differences were seen for morbid obese patients (BMI ≥40 Kg/M2). CONCLUSIONS: Obesity did not increase the mortality rate, but improved intensive care unit length of stay. The current prognostic scoring systems do not include BMI, possibly underestimating the risk of death, and other quality of care indexes in obese patients. New studies could be useful to clarify how body mass index impacts the mortality rate.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):359-368
DOI 10.1590/S0103-507X2009000400005
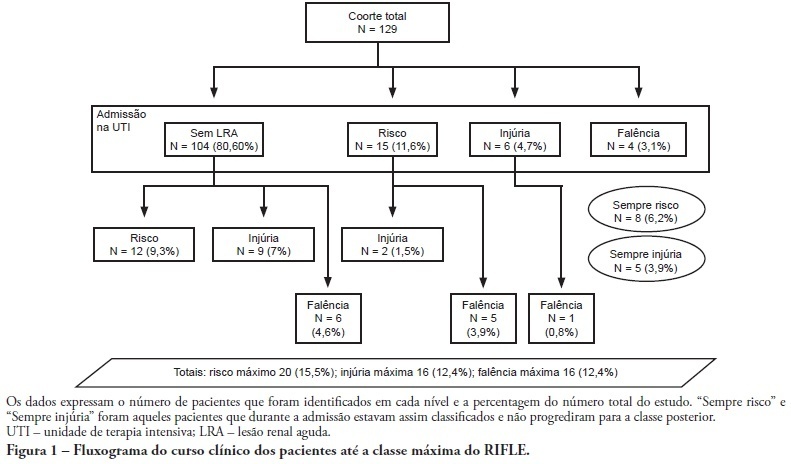
OBJECTIVE: To correlate the RIFLE classification with mortality and length of stay both in the intensive care unit and hospital. METHODS: A prospective, observational, longitudinal cohort study, approved by the Institution's Ethics Committee. Data were collected for all patients staying longer than 24 hours in the intensive care unit of Hospital Universitário Polydoro Ernani de São Thiago - Universidade Federal de Santa Catarina from September 2007 to March 2008, followed-up either until discharge or death. Patients were divided in two groups: with or without acute kidney injury. The acute kidney injury group was additionally divided according to the RIFLE and sub-divided according to the maximal score in Risk, Injury of Failure. Loss and End-stage classes were not included in the study. APACHE II and SOFA were also evaluated. The t Student and Chi-Square tests were used. A P<0.05 was considered statistically significant. RESULTS: The sample included 129 patients, 52 (40.3%) with acute kidney injury according to RIFLE. Patients were more severely ill in this group, with higher APACHE and SOFA scores (P<0.05). Compared to the without kidney injury group, the kidney injury severity caused increased intensive care unity (Risk 25%; Injury 37.5%; Failure 62.5%) and in-hospital (Risk 50%; Injury 37.5%; Failure 62.5%) mortality, and longer intensive care unit stay (P<0.05). CONCLUSION: The RIFLE system, according to the severity class, was a marker for risk of increased intensive care unit and in-hospital mortality, and longer intensive care unit stay. No relationship with in-hospital length of stay was found.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)