You searched for:"Marcelo Moock"
We found (6) results for your search.-
Editorial
COVID-19 pandemic
Rev Bras Ter Intensiva. 2020;32(1):1-1
Abstract
EditorialCOVID-19 pandemic
Rev Bras Ter Intensiva. 2020;32(1):1-1
DOI 10.5935/0103-507X.20200001
Views0Once again, a disease advances and worries everyone. Unlike other epidemics and thanks to advances in science, this flu was considered distinct, its etiological agent isolated and identified, and new detection tests were developed in record time. So far there are no effective vaccines or active antiviral drugs for SARS-2, the coronavirus responsible for the […]See more -
Original Articles
Impact of obesity on critical care treatment in adult patients
Rev Bras Ter Intensiva. 2010;22(2):133-137
Abstract
Original ArticlesImpact of obesity on critical care treatment in adult patients
Rev Bras Ter Intensiva. 2010;22(2):133-137
DOI 10.1590/S0103-507X2010000200006
Views0See moreSTUDY OBJECTIVE: Obese patients seem to have worse outcomes and more complications during intensive care unit (ICU) stay. This study describes the clinical course, complications and prognostic factors of obese patients admitted to an intensive care unit compared to a control group of nonobese patients. DESIGN: Retrospective observational study. SETTING: A 10-bed adult intensive care unit in a university-affiliated hospital. METHODS: All patients admitted to the intensive care unit over 52 months (April 01/2005 to November 30/2008) were included. Obese patients were defined as those with a body mass index (BMI) ≥ 30 Kg/M2. Demographic and intensive care unit related data were also collected. An clinical and demographical matching group of eutrophic patients selected from the data base as comparator for mortality and morbidity outcomes. The Mann-Whitney test was used for numeric data comparisons and the Chi Square test for categorical data comparisons. RESULTS: Two hundred nineteen patients were included. The obese group (n=73) was compared to the eutrophic group (n= 146). Most of this group BMI ranged between 30 – 35 Kg/M2. Only ten patients had body mass index ≥40 Kg/M2. Significant differences between the obese and eutrophic groups were observed in median APACHE II score (16 versus 12, respectively; p<0.05) and median intensive care unit length of stay (7 versus 5 days respectively; p<0,05). No significant differences were seen regarding risk of death, mortality rate, mechanical ventilation needs, days free of mechanical ventilation and tracheostomy rates. The observed mortality was higher than the APACHE II-predicted for both groups, but the larger differences were seen for morbid obese patients (BMI ≥40 Kg/M2). CONCLUSIONS: Obesity did not increase the mortality rate, but improved intensive care unit length of stay. The current prognostic scoring systems do not include BMI, possibly underestimating the risk of death, and other quality of care indexes in obese patients. New studies could be useful to clarify how body mass index impacts the mortality rate.
-
A comparative study between early and late tracheostomy in patients ongoing mechanical ventilation
Rev Bras Ter Intensiva. 2007;19(4):444-449
Abstract
A comparative study between early and late tracheostomy in patients ongoing mechanical ventilation
Rev Bras Ter Intensiva. 2007;19(4):444-449
DOI 10.1590/S0103-507X2007000400007
Views0See moreBACKGROUND AND OBJECTIVES: To assess the incidence of tracheostomy in patients submitted to mechanic ventilation (MV); to compare the length of stay (LOS), duration of MV, APACHE II and mortality among patients submitted to tracheostomy, according to the moment of its application (early or late). METHODS: A retrospective observation study type cohort was done from April thru October 2005 including 190 patients at the adult intensive care unit (ICU) of Hospital Estadual do Grajaú. RESULTS: Among the 190 patients, 32 (16.84%) were submitted to tracheostomy with a longer LOS (30.16 days) as compared to those that were not (p < 0.001). The mean time of the tracheostomy procedure was 13.5 days from the starting of the MV. It is known that there still is no guidance for defining an ideal period for the operation. On this study, the prevalence of early tracheostomy (<13 days) was 46.87% (n = 15) and the late tracheostomy (> 13 days) was 53.13% (n = 17). In a meaningful way, the patients with early tracheostomy obtained APACHE II superior to those with late tracheostomy (18.2 versus 13.47), however there was no difference regarding the mortality rate. There was no difference regarding the time of ICU LOS (28.9 versus 31.28 days) and the MV time (29.73 versus 32.23 days) for both groups. CONCLUSIONS: The incidence of tracheostomy was high, being associated to a smaller ICU mortality but with a longer LOS and more complications. There was no significant difference regarding the destination of the patients when submitted to early or late tracheostomy.
-
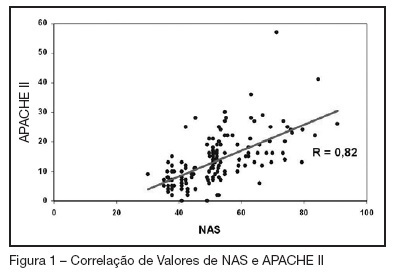
Nursing Activities Score: comparison among the Index APACHE II and the mortality in patients admitted in intensive care unit
Rev Bras Ter Intensiva. 2007;19(3):327-330
Abstract
Nursing Activities Score: comparison among the Index APACHE II and the mortality in patients admitted in intensive care unit
Rev Bras Ter Intensiva. 2007;19(3):327-330
DOI 10.1590/S0103-507X2007000300010
Views0See moreBACKGROUND AND OBJECTIVES: Searching the literature, we found no studies which correlate the NAS (Nursing Activities Score), who determines the real time of nursing evaluation and patient care, with mortality for prognostic index. The objectives this study were to know the values of the NAS score at ours service, try to find correlations between this values and the APACHE II index and to analyze the mortality rates with NAS scores. METHODS: This is a prospective ICU inpatient study from July to November/2005. Our data’s of the APACHE II score were recorded from the QuaTI system study. Qui-square test or equivalent was done to compare the proportions. For the analyses we utilized the EPI-INFO-6 software. RESULTS: The sample was 148 patients, mean age of 55.5 years with 59.4% males. The mean hospitalization time were 9.1 days, mortality rate of 29.7%, mean NAS score of 51.5% and mean APACHE II score of 13.4. There were a positive correlation ship between NAS and APACHE II index (R = 0.82). Selecting only the patients with NAS more than 51 we found that 41 in 83 died and 42 in 83 survived. Those whose NAS were under 51, only 3 in 65 died and 62 in 65 survived (p < 0.005), identifying an statistically significant group. CONCLUSIONS: In this study the mean value of NAS were 51.5%. There were good correlation with the APACHE II index and we shown that the mortality rate was high in the higher NAS values.
-
Critical analysis of hospital surgical patients in intensive care unit
Rev Bras Ter Intensiva. 2007;19(3):348-353
Abstract
Critical analysis of hospital surgical patients in intensive care unit
Rev Bras Ter Intensiva. 2007;19(3):348-353
DOI 10.1590/S0103-507X2007000300014
Views0BACKGROUND AND OBJECTIVES: Each intensive care units result has to be observed in the context of medical care, as well as the institution witch it belongs. There are many types of prognostic index in intensive care. The APACHE II was introduced by Knaus et al. in 1985, being a widely used system to evaluate the illness severity in intensive care patients. This objective was evaluated the prognostic index (APACHE II) in patients submitted to elective or emergency gastrointestinal surgery admitted to the ICU. METHODS: Medical school intensive care unit. It was collected the following data: age, sex, length of stay, intensive care indication, type of surgery (elective or emergency), body mass index (BMI) APACHE II and predicted mortality. RESULTS: A total of 38 patients data were collected during the period of April 2005 to April 2006. Eighteen patients died and twenty survived. The age of the non-survivors varied from 44 to 92 (mean age 66.6); while the age of the survivors varied from 28 to 78 (mean age 59. 1). The BMI of the non-survivors varied from 22 to 29 (mean body mass index 26) while in the other group the mean body mass index was 25. 6. No significant difference was noted in the age and body mass index of both groups. The length of stay varied from 2 to 52 days in the non-survivors group (mean 11.3 days), while in the survivors group varied from 1 to 30 days (mean 4.9). The APACHE II varied from 5 to 32 in the non-survivors group (mean 19.14). While in the survivors group varied from 1 to 18 (mean 8.6). The length of stay and APACHE II demonstrated a significant difference in both groups, being higher in the non-survivors group. The non-survivors predicted mortality varied from 3.1 to 84.9 (mean 38.8); while the survivors mean was 7.5. The Standardized Mortality Rate in this study was 1.22. CONCLUSIONS: Non-survivors patients APACHE II was higher than the survivors; the SMR was similar to others studies; the length of stay was longer in the non-survivors group; no statistic difference was noted in the body mass index.
Keywords:APACHE IIsurgical patientsSee more -
Mechanical ventilation in the acute lung injury/acute respiratory distress syndrome
Rev Bras Ter Intensiva. 2007;19(3):374-383
Abstract
Mechanical ventilation in the acute lung injury/acute respiratory distress syndrome
Rev Bras Ter Intensiva. 2007;19(3):374-383
DOI 10.1590/S0103-507X2007000300020
Views0See moreBACKGROUND AND OBJECTIVES: The II Brazilian Consensus Conference on Mechanical Ventilation was published in 2000. Knowledge on the field of mechanical ventilation evolved rapidly since then, with the publication of numerous clinical studies with potential impact on the ventilatory management of critically ill patients. Moreover, the evolving concept of evidence – based medicine determined the grading of clinical recommendations according to the methodological value of the studies on which they are based. This explicit approach has broadened the understanding and adoption of clinical recommendations. For these reasons, AMIB – Associação de Medicina Intensiva Brasileira and SBPT – Sociedade Brasileira de Pneumologia e Tisiologia – decided to update the recommendations of the II Brazilian Consensus. Acute Respiratory Distress Syndrome (ARDS) has been one of the updated topics. This objective was described the most important topics related to mechanical ventilation in patients with acute respiratory distress syndrome. METHODS: Systematic review of the published literature and gradation of the studies in levels of evidence, using the key words mechanical ventilation and acute respiratory distress syndrome. RESULTS: Recommendations on the use of lung protective strategies during mechanical ventilation based on reduced tidal volumes and limitation of plateau pressure. The state of the art of recruitment maneuvers and PEEP titration is also discussed. CONCLUSIONS: The mechanical ventilation of patients with ADRS changed in the last few years. We presented the role of lung protective strategies that could be applied to these patients.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




