Abstract
Rev Bras Ter Intensiva. 2022;34(4):452-460
DOI 10.5935/0103-507X.20220087-en
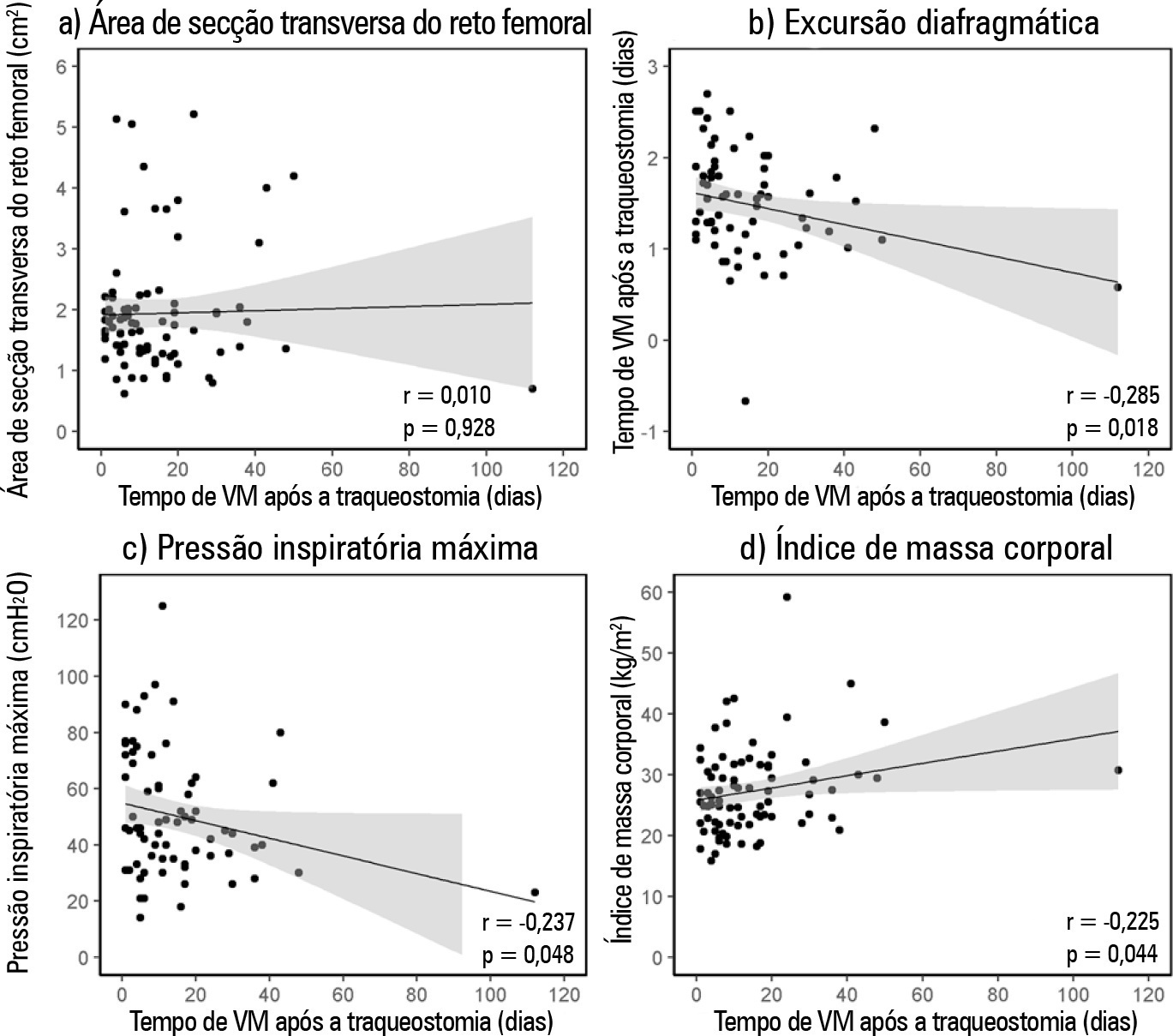
To verify the relationship between the rectus femoris cross-sectional area and diaphragmatic excursion with successful weaning from mechanical ventilation in chronic critically tracheostomized patients.
This was a prospective observational cohort study. We included chronic critically ill patients (those who underwent tracheostomy placement after 10 days under mechanical ventilation). The rectus femoris cross-sectional area and diaphragmatic excursion were obtained by ultrasonography performed within the first 48 hours after tracheostomy. We measured rectus femoris cross-sectional area and diaphragmatic excursion to assess their association with weaning from mechanical ventilation, including their potential to predict successful weaning and survival throughout the intensive care unit stay.
Eighty-one patients were included. Forty-five patients (55%) were weaned from mechanical ventilation. The mortality rates were 42% and 61.7% in the intensive care unit and hospital, respectively. The fail group in relation to the success group at weaning presented a lower rectus femoris cross-sectional area (1.4 [0.8] versus 1.84 [0.76]cm2, p = 0.014) and lower diaphragmatic excursion (1.29 ± 0.62 versus 1.62 ± 0.51cm, p = 0.019). When rectus femoris cross-sectional area ≥ 1.80cm2 and diaphragmatic excursion ≥ 1.25cm was a combined condition, it had a strong association with successful weaning (adjusted OR = 20.81, 95%CI 2.38 - 182.28; p = 0.006) but not with intensive care unit survival (adjusted OR = 0.19, 95%CI 0.03 - 1.08; p = 0.061).
Successful weaning from mechanical ventilation in chronic critically ill patients was associated with higher measurements of rectus femoris cross-sectional area and diaphragmatic excursion.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):64-71
DOI 10.5935/0103-507X.20150011
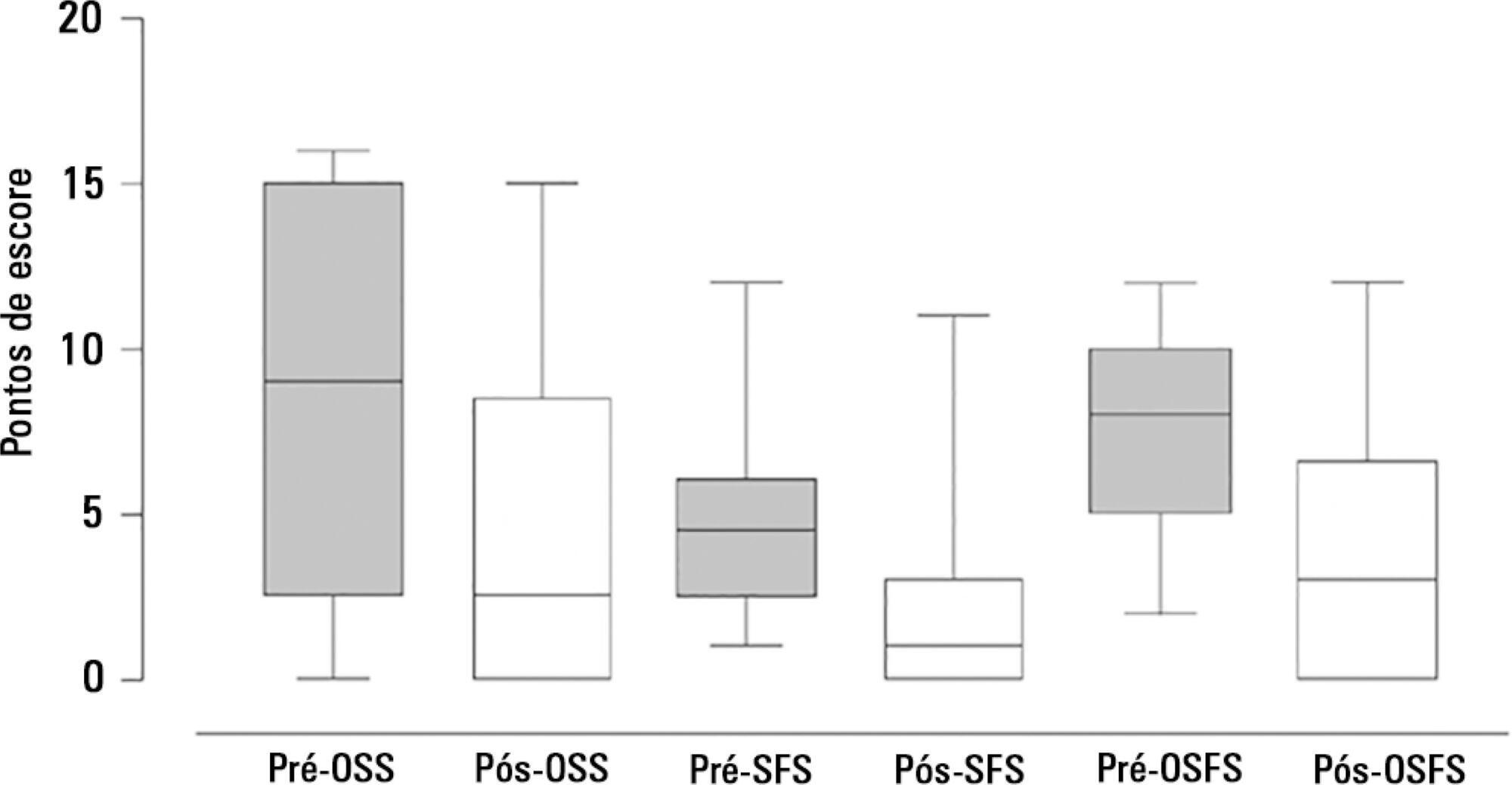
The aim of the present study was to assess the feasibility of the early implementation of a swallowing rehabilitation program in tracheostomized patients under mechanical ventilation with dysphagia.
This prospective study was conducted in the intensive care units of a university hospital. We included hemodynamically stable patients under mechanical ventilation for at least 48 hours following 48 hours of tracheostomy and with an appropriate level of consciousness. The exclusion criteria were previous surgery in the oral cavity, pharynx, larynx and/or esophagus, the presence of degenerative diseases or a past history of oropharyngeal dysphagia. All patients were submitted to a swallowing rehabilitation program. An oropharyngeal structural score, a swallowing functional score and an otorhinolaryngological structural and functional score were determined before and after swallowing therapy.
We included 14 patients. The mean duration of the rehabilitation program was 12.4 ± 9.4 days, with 5.0 ± 5.2 days under mechanical ventilation. Eleven patients could receive oral feeding while still in the intensive care unit after 4 (2 - 13) days of therapy. All scores significantly improved after therapy.
In this small group of patients, we demonstrated that the early implementation of a swallowing rehabilitation program is feasible even in patients under mechanical ventilation.
Abstract
Rev Bras Ter Intensiva. 2011;23(1):56-61
DOI 10.1590/S0103-507X2011000100010
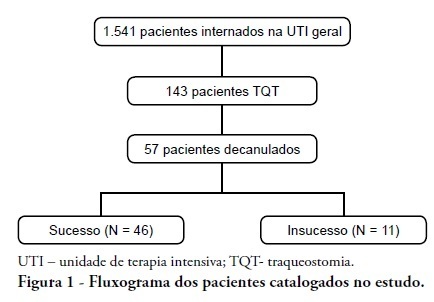
INTRODUCTION: Tracheostomy is probably the most common surgical procedure in critically ill patients and is generally performed to facilitate mechanical ventilation weaning. Evidence-based guidelines have confirmed the benefits of tracheostomy weaning protocols and of the physiotherapists engagement in this process; however, no consensus decannulation criteria are currently available. Therefore, this study aimed to evaluate the influence of peripheral muscle strength and other indicators on decannulation success. METHODS: This was an observational retrospective study that analyzed the medical records of patients admitted to the medical and surgical intensive care unit of Hospital Agamenon Magalhães between March 2007 and August 2009. Respiratory and peripheral muscle strengths were evaluated in decannulated patients. RESULTS: Overall, 1,541 patients were evaluated, 143 of which had been tracheostomized, and only 57 of which had been decannulated. Forty-six patients had a satisfactory decannulation outcome, while 11 had decannulation failure, requiring the return to an artificial airway within 2 weeks. The calculated Medical Research Council peripheral muscle strength score was significantly lower for the failure group than for the successful decannulation group (28.33 ± 15.31 vs. 41.11 ± 11.52; P = 0.04). Scores above or equal 26 had 94.4% sensitivity and 50.0% specificity for the decannulation outcome, with an area under the ROC curve of 0.7593. In addition, white blood cell counts were higher in decannulation failure group patients (14,070 ± 3,073 vs. 10,520 ± 3,402 cells/μL; P = 0.00). CONCLUSION: This study has shown that peripheral muscle strength and blood leucocyte counts evaluated on the day of decannulation may influence the tracheostomy decannulation success rate.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):192-195
DOI 10.1590/S0103-507X2010000200014
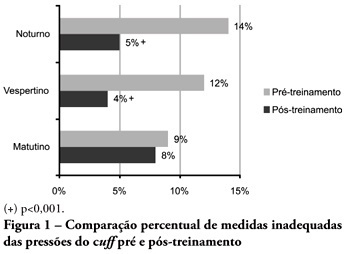
OBJECTIVES: Direct cuff pressure to the tracheal wall can cause damage. This paper aimed to verify the effectiveness of nursing team training on cuff pressure control. METHODS: A retrospective survey was initially made on the records of cuff pressure measurements from January 2007 to June 2008 and the inadequacy percent was verified. Next, a nursing team training program was provided involving all nursing shift teams during June 2008, and after the training the appropriate cuff pressures proportion was prospectively recorded between June and December 2008. The proportion of inappropriate cuff pressure was compared between the work shifts (morning, afternoon and evening-night) and between pre- and post-training, using the qualitative Chi-square test. The 5% limit (p<0.05) was considered for significant differences. RESULTS: For the pre-training period, inappropriate cuff pressure measures (over 30cmH2O) during morning, afternoon and evening-night shifts were 9.2%, 11.9% and 13.7%, respectively. For the post-training phase, 7.6%, 4.1% and 5.2% inappropriate cuff-pressures were identified for the morning, afternoon and evening-night shifts, respectively, with a significant reduction for the afternoon and evening-night shifts, respectively (p<0.001). CONCLUSION: Nursing team training was effective for inadequate cuff pressure harms awareness improvement, and resulted in safer pressure levels.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):47-52
DOI 10.1590/S0103-507X2010000100009
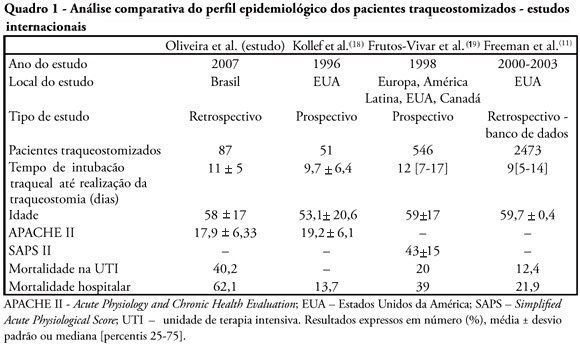
OBJECTIVES: Tracheostomy is a common procedure in intensive care unit to promote mechanical ventilation weaning. Despite tracheostomy is increasingly used there is no agreement of actual clinical practice of tracheostomy in different groups of patients in our environment. Objective of this study was to evaluate the epidemiological profile and outcomes of patients with tracheostomy at a clinical-surgical intensive care unit and compare this profile with the current literature. METHODS: Retrospective descriptive study through review of medical records and quality control database of "QuaTI" (Qualidade em Terapia Intensiva) of 87 patients with tracheostomy at Santa Casa de Belo Horizonte intensive care unit in 2007. We studied variables related to evolution aspects. RESULTS: The clinical and epidemiological analysis of the 87 patients showed: mean age 58 ± 17 years, mean Acute Physiology and Chronic Health Evaluation - APACHE II 18 ± 6, mean time of orotracheal intubation before tracheostomy of 11.17 ± 4.78 days. Intensive care unit mortality was 40.2% (35/87 patients), ward mortality was 36.5% (19/52) and overall hospital mortality 62.1% (54/87). Mean age of patients who died at intensive care unit (65 + 17 years) was greater than who were discharged to ward (53 ± 16 years) p = 0.003. Mean age of who died in hospital (intensive care unit and ward) (62 ± 17 years) was also higher than survivors (52 ± 16 years) p = 0.008. Old age (> 65 years) was related to intensive care unit mortality (OR 2.874, CI 1.165 a 7.088 p = 0.020) and also related to the overall hospital mortality (OR 3.202, CI 1.188 a 8.628 p = 0.019). There were not others variables related to mortality in this sample. CONCLUSIONS: The epidemiological profile of patients who underwent tracheotomy in the intensive care unit showed high mortality rate when compared to international series. Senility was related to worse outcome in these patients. Other issues were not related mortality in this group.
Abstract
Rev Bras Ter Intensiva. 2009;21(2):169-172
DOI 10.1590/S0103-507X2009000200009
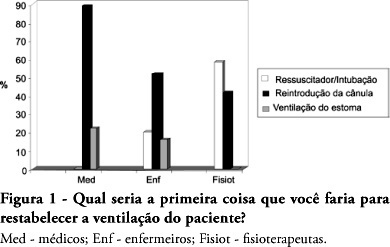
OBJECTIVES: The aim of this study was to evaluate the level of knowledge of health care professionals in an emergency situation related to tracheostomy tube displacement METHODS: a descriptive and exploratory study was carried out with the intensive care unit health professionals of a university hospital in Salvador, Brazil, from July to September 2007. For this purpose, a questionnaire was translated and adapted from a previous study. Questions were: 1- Have you dealt with this emergency? 2 - What is the first thing you do? 3- Do you know what the stay sutures are for? 4 - How are they used in an emergency setting? 5 -Do you know what to do with the introducer? RESULTS: the sample comprised 41 professionals (nine physicians, 20 nurses and 12 physiotherapists). A descriptive analysis showed that 63% of professionals had never experienced such complications. Analysis of a subgroup showed that 42% of physiotherapists, 56% of physicians and 69% of nurses would act inappropriately. Analyzing the level of knowledge about the importance of stay sutures, the study showed that 78% of the sample did not know what they were or how to use them, and 63.4% did not know how to use the introducer correctly. CONCLUSIONS: , regarding the use of a tracheostomy tube in a situation of emergency, the level of knowledge of the professionals evaluated was insufficient. The greatest shortcoming was detected in the level of knowledge about stay sutures.
Abstract
Rev Bras Ter Intensiva. 2008;20(3):220-225
DOI 10.1590/S0103-507X2008000300003
OBJECTIVES: Correct cuff inflation allows appropriate ventilation, and prevents aspiration pneumonia as well as several tracheal complications. The objective of this study was to evaluate endotracheal cuff pressure and/or tracheotomy tubes at zero, 30 and 60 degrees inclination of the patient's bed head section in adult intensive care units. METHODS: A cross sectional study was carried out evaluating the cuff pressure, the expiratory tidal volume (VT) and the peak airway pressure (PP) at inclinations zero, 30 and 60 degree of the head section of the patients' bed. The 30 degree inclination was considered the standard position used as control to analyze values in the zero and 60 degree positions, which were randomly ordered. The Student's t test was used and was considered significant when p < 0.05. RESULTS: A sample of 12 women and 12 men with a mean age of 51.29 ± 19.55 years was surveyed. When inclination of the bed head section was changed from 30 to zero degrees, there was a 16.9% mean reduction of the cuff pressure and 11.8% mean increase of the PP. On the other hand, changing the position from 30 to 60 degrees caused a mean reduction of 18.8% in the cuff pressure and a mean increase of 13.3% in the PP. Findings were significant when p < 0.05. CONCLUSIONS: To prevent air leak and risk of aspiration pneumonia, adequate adjustments and monitoring of the patients cuff pressure are necessary when inclination of the bed head section is changed.
Abstract
Rev Bras Ter Intensiva. 2007;19(4):444-449
DOI 10.1590/S0103-507X2007000400007
BACKGROUND AND OBJECTIVES: To assess the incidence of tracheostomy in patients submitted to mechanic ventilation (MV); to compare the length of stay (LOS), duration of MV, APACHE II and mortality among patients submitted to tracheostomy, according to the moment of its application (early or late). METHODS: A retrospective observation study type cohort was done from April thru October 2005 including 190 patients at the adult intensive care unit (ICU) of Hospital Estadual do Grajaú. RESULTS: Among the 190 patients, 32 (16.84%) were submitted to tracheostomy with a longer LOS (30.16 days) as compared to those that were not (p < 0.001). The mean time of the tracheostomy procedure was 13.5 days from the starting of the MV. It is known that there still is no guidance for defining an ideal period for the operation. On this study, the prevalence of early tracheostomy (<13 days) was 46.87% (n = 15) and the late tracheostomy (> 13 days) was 53.13% (n = 17). In a meaningful way, the patients with early tracheostomy obtained APACHE II superior to those with late tracheostomy (18.2 versus 13.47), however there was no difference regarding the mortality rate. There was no difference regarding the time of ICU LOS (28.9 versus 31.28 days) and the MV time (29.73 versus 32.23 days) for both groups. CONCLUSIONS: The incidence of tracheostomy was high, being associated to a smaller ICU mortality but with a longer LOS and more complications. There was no significant difference regarding the destination of the patients when submitted to early or late tracheostomy.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)