Abstract
Rev Bras Ter Intensiva. 2019;31(1):27-33
DOI 10.5935/0103-507X.20190006
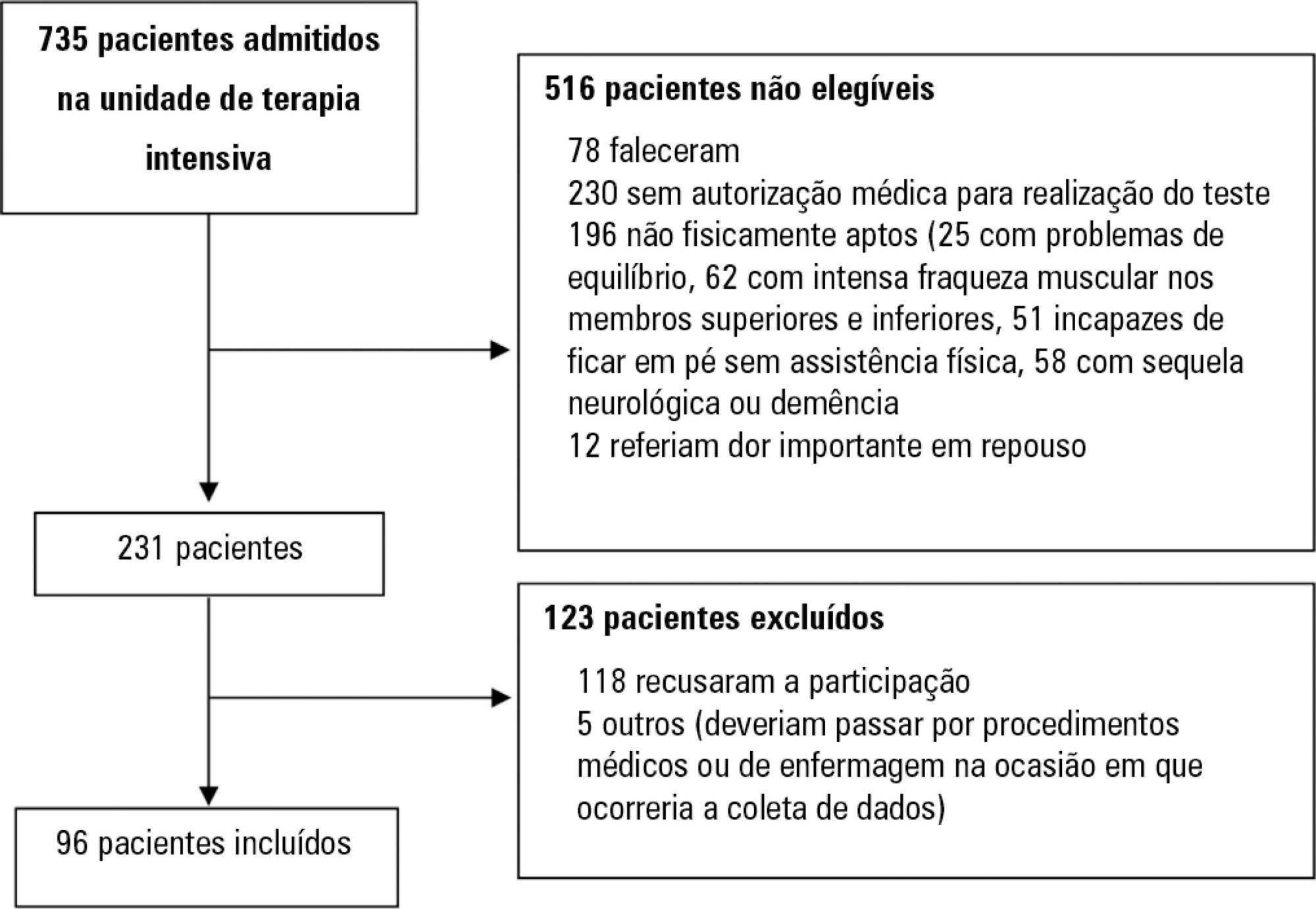
Assess the Five Times Sit-to-Stand Test safety and clinimetric properties in older patients hospitalized in an intensive care unit.
Test safety was assessed according to the incidence of adverse events and through hemodynamic and respiratory data. Additionally, reliability properties were investigated using the intraclass correlation coefficients, standard error of measurement, standard error percentage change, Altman-Bland plot and a survival agreement plot.
The overall suitability of the Five Times Sit-to-Stand Test was found to be low, with 29.8% meeting the inclusion criteria. Only 44% of the hospitalized patients who met the inclusion criteria performed the test, with no need for discontinuation in any patient. Heart rate (79.7 ± 10.2bpm/86.6 ± 9.7bpm; p = 0.001) and systolic blood pressure (118 ± 21.4mmHg/129 ± 21.5mmHg; p = 0.031) were the only variables that presented a significant statistical increase, with no evidence of exacerbated response to the test. Additionally, no adverse events were reported from participating and both test-retest and interrater reliability were high (intraclass correlation coefficient ≥ 0.99).
The Five Times Sit-to-Stand Test was proven to be safe and to have excellent reliability. Its clinical use, however, may be restricted to high-functioning older adults in hospital settings.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):293-302
DOI 10.5935/0103-507X.20170055
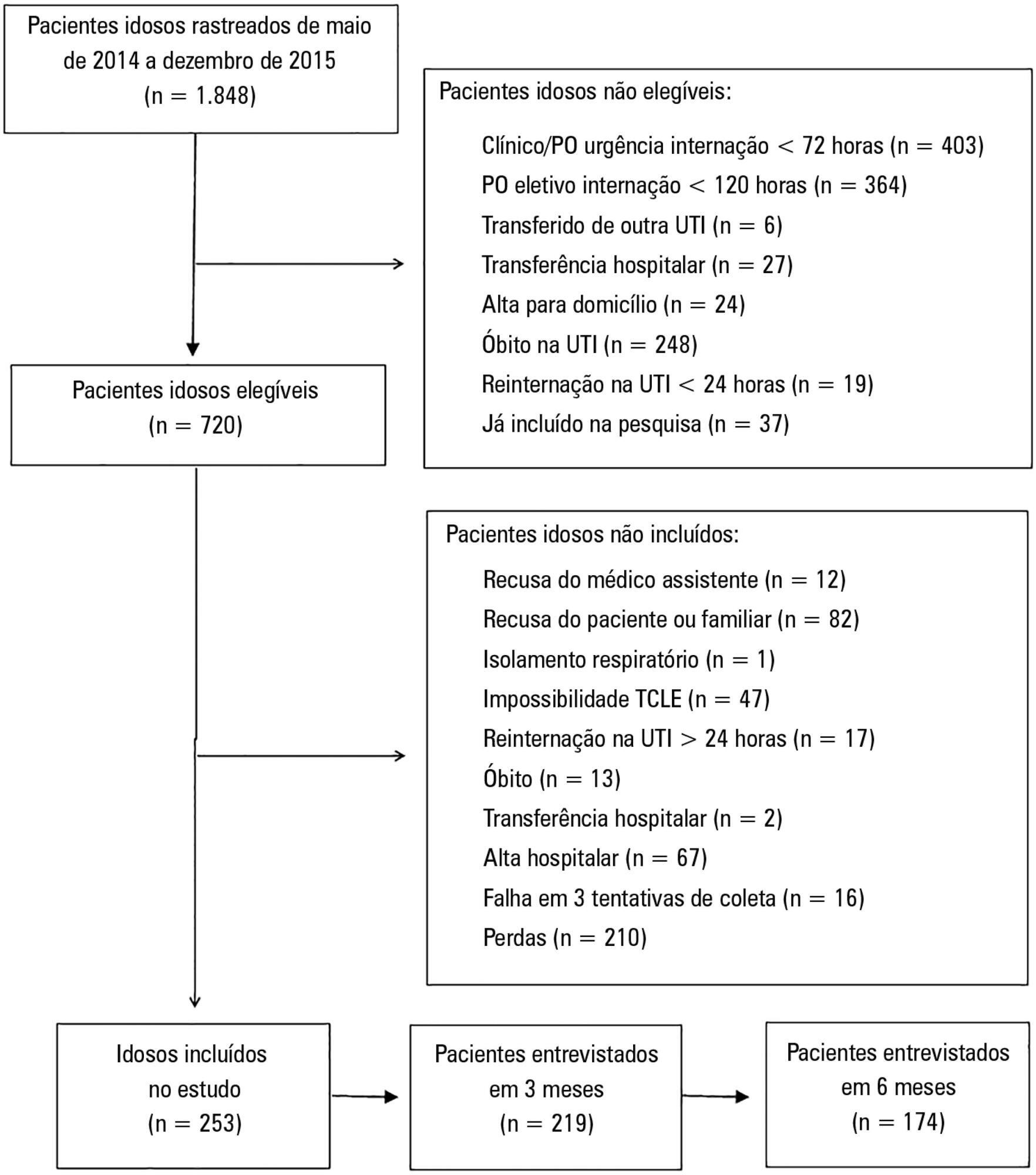
To compare the functional capacity of younger elderly individuals (60 to 79 years old) with that of older elderly individuals (≥ 80 years old) during the first 6 months after discharge from the intensive care unit.
A multicenter prospective cohort study was conducted, in which data on intensive care unit admission and outcomes after hospital discharge (immediate post-discharge, after 3 months and after 6 months) were collected. Muscle strength was evaluated through the protocol of the Medical Research Council and dynamometry (handgrip); the ability to perform activities of daily life and functional independence were assessed by the Barthel index and the usual level of physical activity (International Physical Activity Questionnaire); and quality of life was assessed by the 12-Item Short-Form Health Survey Version 2.
Among the 253 patients included, 167 were younger elderly (between 61 and 79 years old), and 86 were older elderly (≥ 80 years old). During the sixth month of evaluation, the older elderlies presented a higher need for a caregiver (69.0% versus 49, 5%, p = 0.002). Functional capacity prior to intensive care unit admission and in the third month after discharge was lower in older elderlies than in younger ones (Barthel prior to the intensive care unit: 73.0 ± 30.0 versus 86.5 ± 22.6; p <0.001, Barthel in the third month: 63.5 ± 34.0 versus 71.5 ± 35.5, p = 0.03), as was the usual level of physical activity (International Physical Activity Questionnaire in the third month: active/very active 3.4% versus 18.3%, no physical activity 64.4% versus 39.7%, p < 0.001, and International Physical Activity Questionnaire in the sixth month: active/very active 5.8% versus 20.8%, no physical activity 69.2% versus 43.4%, p = 0.005). Older elderlies had lower muscle strength when assessed according to handgrip in both the dominant (14.5 ± 7.7 versus 19.9 ± 9.6, p = 0.008) and non-dominant limb (13.1 ± 6.7 versus 17.5 ± 9.1, p = 0.02). There were no differences in functional capacity loss or reported quality of life between the age groups.
Although there were great functional capacity losses after discharge from the intensive care unit in both age groups, there was no difference in the magnitude of functional capacity loss between younger (60 to 79 years) and older elderly individuals (≥ 80 years old) during the first 6 months after discharge from the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2015;27(4):333-339
DOI 10.5935/0103-507X.20150057
To evaluate the prevalence of myocardial dysfunction and its prognostic value in patients with severe sepsis and septic shock.
Adult septic patients admitted to an intensive care unit were prospectively studied using transthoracic echocardiography within the first 48 hours after admission and thereafter on the 7th-10th days. Echocardiographic variables of biventricular function, including the E/e' ratio, were compared between survivors and non-survivors.
A total of 99 echocardiograms (53 at admission and 46 between days 7 - 10) were performed on 53 patients with a mean age of 74 (SD 13) years. Systolic and diastolic dysfunction was present in 14 (26%) and 42 (83%) patients, respectively, and both types of dysfunction were present in 12 (23%) patients. The E/e' ratio, an index of diastolic dysfunction, was the best predictor of hospital mortality according to the area under the ROC curve (0.71) and was an independent predictor of outcome, as determined by multivariate analysis (OR = 1.36 [1.05 - 1.76], p = 0.02).
In septic patients admitted to an intensive care unit, echocardiographic systolic dysfunction is not associated with increased mortality. In contrast, diastolic dysfunction is an independent predictor of outcome.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):197-206
DOI 10.1590/S0103-507X2012000200017
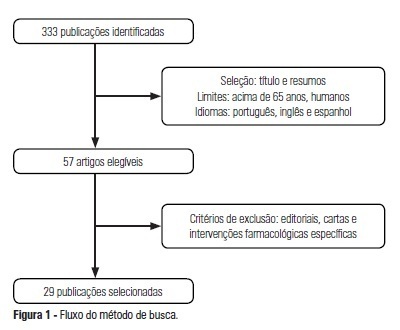
OBJECTIVE: The use of interventionist medical technology in terminal elderly patients must be associated with palliative care as a measure of clinical support in intensive care units. Palliative care is an important component of end-of-life care, and the assistance provided by the healthcare team should be guided by decisions made by patients and their family members. Prolongation of life not accompanied by therapies aimed at relieving symptoms, such as pain and dyspnea, contributes to patient and family member stress suffering. The aim of the present study was to survey advances made in the application of palliative care in intensive care units. METHODS: Medline and Bireme were used to perform a systematic literature review of intensive care units-based palliative care for elderly patients. RESULTS: A total of 29 articles describing palliative care in intensive care units were analyzed according to the variables "satisfaction of relatives when they participate in the discussions on palliative care" and "difficulties to implement such type of care due to lack of technical skills of the health caregivers." CONCLUSION: Palliative care for elderly patients in intensive care units must be more thoroughly investigated to improve the relationships and communication among patients, their relatives, and the healthcare team. As greater numbers of elderly patients are admitted to intensive care units, the skills of health caregivers must improve to meet the challenges posed by the end-of-life care.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):138-143
DOI 10.1590/S0103-507X2010000200007
BACKGROUND: The elderly population is increasing all over the world. The need of intensive care by the elderly is also increasing. There is a lack of studies investigating the risk factors for death among critically ill elderly patients. This study aims to investigate the factors associated with death in a population of critically ill elderly patients admitted to an intensive care unit in Brazil. METHODS: This is a retrospective cohort study including all elderly patients (>60 years) admitted to an intensive care unit in Fortaleza, Brazil, from January to December 2007. A comparison between survivors and nonsurvivors was done and the risk factors for death were investigated through univariate and multivariate analysis. RESULTS: A total of 84 patients were included, with an average age of 73 ± 7.6 years; 59% were female. Mortality was 62.8%. The main cause of death was multiple organ dysfunction (42.3%), followed by septic shock (36.5%) and cardiogenic shock (9.7%). Complications during intensive care unit ICU stay associated with death were respiratory failure (OR=61, p<0.001), acute kidney injury (OR=23, p<0.001), sepsis (OR=12, p<0.001), metabolic acidosis (OR=17, p<0.001), anemia (OR=8.6, p<0.005), coagulation disturbance (OR=5.9, p<0.001) and atrial fibrillation (OR=4.8, p<0.041). Independent risk factors for death were age (OR=1.15, p<0.005), coma (OR=7.51, p<0.003), hypotension (OR=21.75, p=0.003), respiratory failure (OR=9.93, p<0.0001) and acute kidney injury (OR=16.28, p<0.014). CONCLUSION: Mortality is high among critically ill elderly patients. Factors associated with death were age, coma, hypotension, respiratory failure and acute kidney injury.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):432-436
DOI 10.1590/S0103-507X2009000400014
The world is aging. In Brazil, and in several other countries in the world, changes in population's age composition have been accompanied by an increase in demand for types of health care whose cost is high. Actually, some moral conflicts are arising from allocation of public resources for health, because the magnitude of social inequalities in health and limited resources require that priorities for public management are based on knowledge of the health situation and the impact of policies, programs, projects and actions on health. In this context, the intensive medicine, managers and physicians in intensive care are subject to moral conflicts, especially at the fair micro allocation resources for the elderly in the intensive care unit level. This paper attempts to review the situation of conflicts in the light of the tools of bioethics.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):262-268
DOI 10.1590/S0103-507X2009000300005
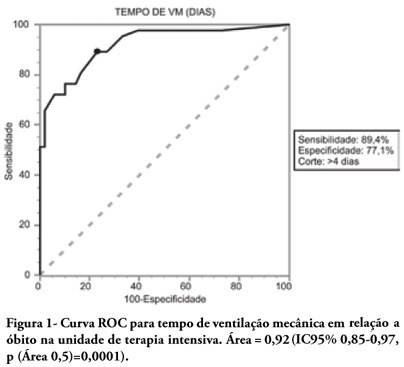
OBJECTIVES: To describe the population of aged as compared to young patients under mechanical ventilation and to analyze the mortality risk factors of this group in an intensive care unit. METHODS: This was a prospective observational trial in patients over 18 years of age, admitted in an intensive care unit and under mechanical ventilation, during one year. Patients were divided into two groups according to age: Group 1 - patients over 65 years old; and Group 2, 65 years old or younger. RESULTS: eighty one mechanic ventilation patients were included, 62 aged and 18 younger, mean ages from aged was 76 years, while in the younger it was 56 years. As compared to the control, aged patients had longer mechanic ventilation time , higher intensive care unit and hospital mortality: 63.1% versus 26.3% and 74.2% versus 47.4% (P<0.05), respectively. In addition, the aged under mechanic ventilation had increased desintubation failures, difficult ventilatory weaning and deaths directly related to respiratory dysfunction. The mechanic ventilation time was an independent risk factor for death in the intensive care unit in aged patients (OR= 2.7, p=0.02). The area under the ROC curve of mechanic ventilation about intensive care unit death was 0.92 (95% CI 0.85-0.97, p (area 0.5)=0.0001), cutoff point of 4 days, sensitivity 89.4% and specificity 77.1%. CONCLUSIONS: Mechanic ventilation patients over 65years of age have a worse prognosis than the younger, and the longer the mechanic ventilation time, the higher will be intensive care mortality.
Abstract
Rev Bras Ter Intensiva. 2009;21(1):1-8
DOI 10.1590/S0103-507X2009000100001
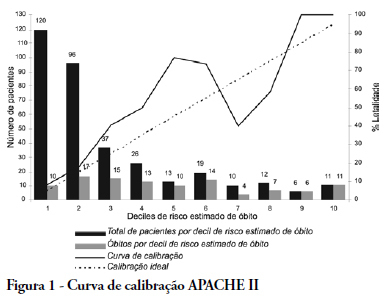
OBJECTIVE: The elderly constitute a population with their own features and frequent admissions in intensive care units. This study has the objective to evaluate the ability to predict the survival of these patients through the APACHE II, UNICAMP II, SAPS II and SAPS 3 indexes, global and Central America/South equations. METHODS: Elderly patients admitted from 01/01/2006 to 12/3/2006, defined as age > 60 years, were included in this study. Those who were readmitted were excluded. The rate of lethality standardized, calibration and discrimination for each index in the remaining patients were analysed. The outcome were death or hospital discharge. RESULTS: Three hundred eighty six elderly patients were included in this study, being 36 excluded by readmission, remaining 350 for analysis. The rate of lethality standardized came near to the unit in all indexes, except the SAPS II (TLP=1.5455) which underestimated the lethality. The calibration, via Hosmer-Lemeshow tests was inadequate (p < 0.05), except for the UNICAMP II (p > 0.5). On the calibration curve, the models have distanced themselves from the pattern line. All of them presented an excellent discrimination via receiver operating characteristics curves (> 0.8). CONCLUSIONS: In the studied population, the models presented an excellent discrimination and inadequate calibration. SAPS II underestimated the lethality.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)