Abstract
Rev Bras Ter Intensiva. 2019;31(1):34-38
DOI 10.5935/0103-507X.20190004
To correlate short-term (duration of mechanical ventilation and length of intensive care unit stay) and long-term (functional capacity) clinical outcomes of patients who reached nutritional adequacy ≥ 70% of predicted in the first 72 hours of hospitalization in the intensive care unit.
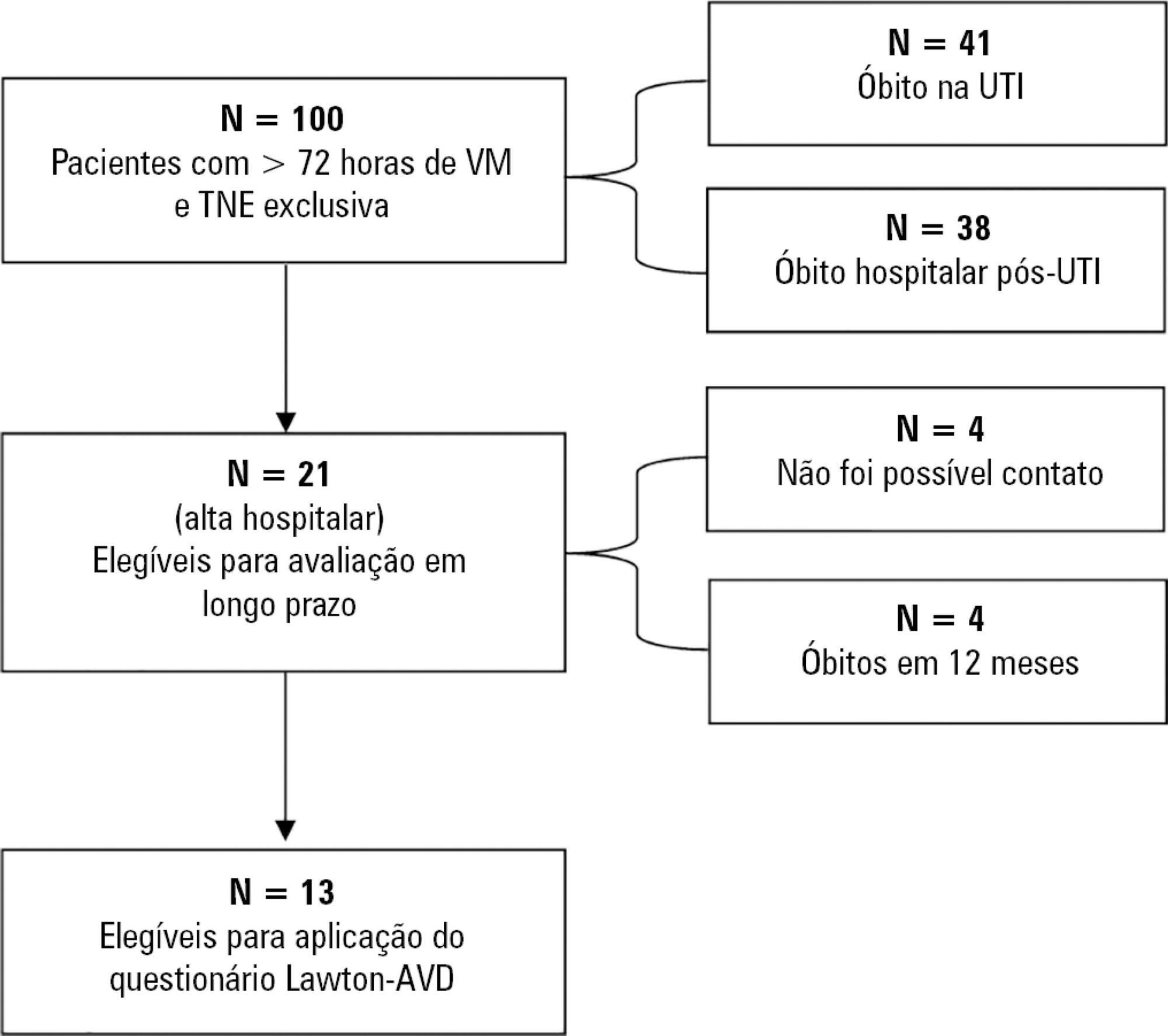
This was a prospective observational pilot study conducted in an 18-bed intensive care unit. A total of 100 mechanically ventilated patients receiving exclusive enteral nutritional support and receiving intensive care for more than 72 hours were included. Patients who never received enteral nutrition, those with spinal cord trauma, pregnant women, organ donors and cases of family refusal were excluded. The variables studied were nutritional adequacy ≥ 70% of predicted in the first 72 hours of hospitalization, length of intensive care unit stay, duration of mechanical ventilation and the ability to perform activities of daily living after 12 months, assessed via telephone contact using the Lawton Activities of Daily Living Scale.
The mean duration of mechanical ventilation was 18 ± 9 days, and the mean intensive care unit length of stay was 19 ± 8 days. Only 45% of the patients received more than 70% of the target nutrition in 72 hours. There was no association between nutritional adequacy and short-term (duration of mechanical ventilation, length of stay in the intensive care unit and mortality) or long-term (functional capacity and mortality) clinical outcomes.
Critically ill patients receiving caloric intake ≥ 70% in the first 72 hours of hospitalization did not present better outcomes in the short term or after 1 year.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):155-162
DOI 10.5935/0103-507X.20140023
To determine the factors that influence the adequacy of enteral nutritional therapy in an intensive care unit.
This prospective observational study was conducted in an intensive care unit between 2010 and 2012. Patients >18 years of age underwent exclusive enteral nutritional therapy for ≥72 hours. The energy and protein requirements were calculated according to the ICU protocols. The data regarding enteral nutrition, the causes of non-compliance, and the biochemical test results were collected daily.
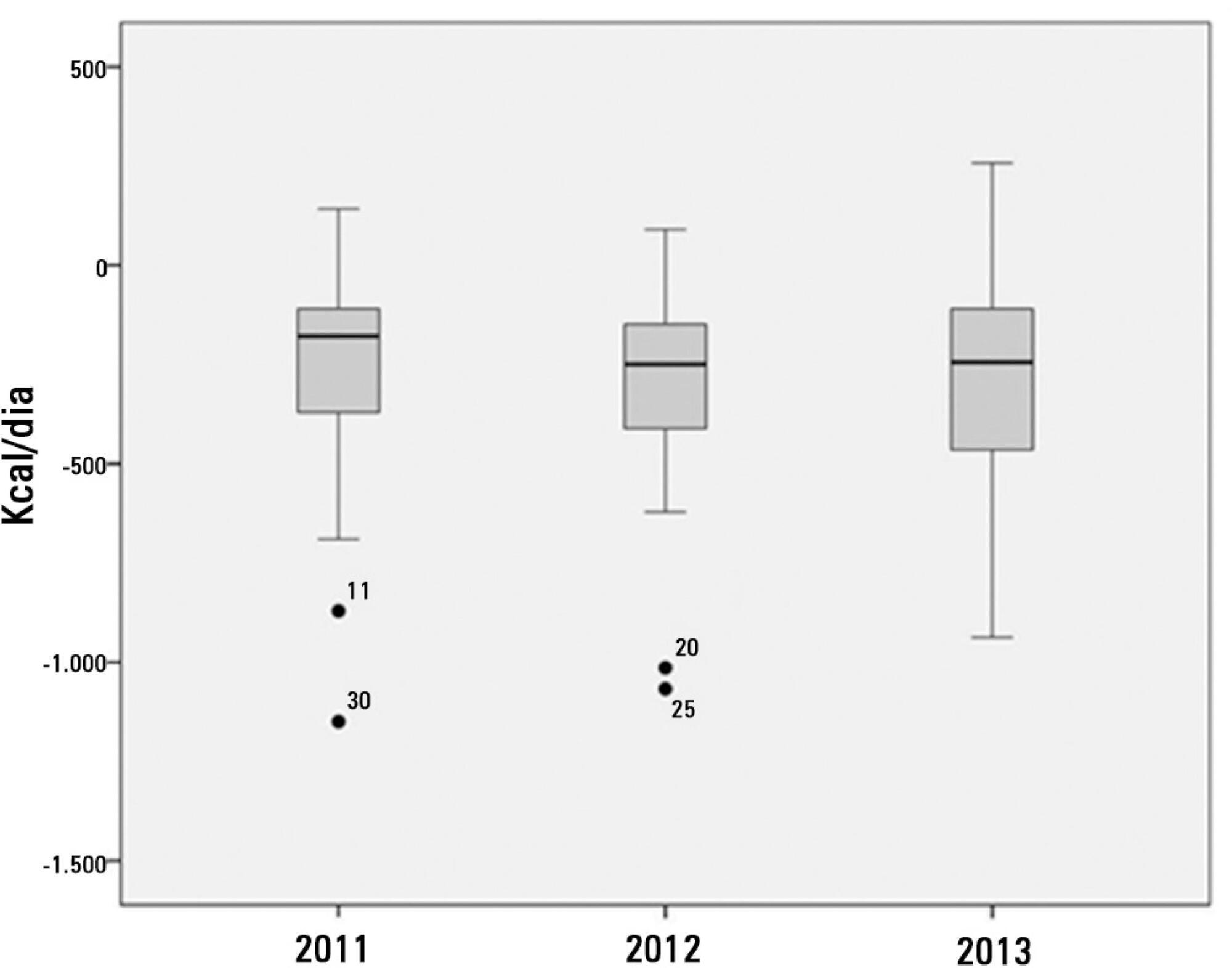
Ninety-three patients admitted to the intensive care unit were evaluated. Among these patients, 82% underwent early enteral nutritional therapy, and 80% reached the nutritional goal in <36 hours. In addition, 81.6%±15.4% of the enteral nutrition volume was infused, with an adequacy of 82.2%±16.0% for calories, 82.2%±15.9% for proteins, and a mean energy balance of -289.9±277.1kcal/day. A negative correlation of C-reactive protein with the volume infused and the energy and protein balance was observed. In contrast, a positive correlation was found between C-reactive protein and the time required to reach nutritional goals. Extubation was the main cause for interrupting the enteral nutritional therapy (29.9% of the interruption hours), and the patients >60 years of age exhibited a lower percentage of recovery of the oral route compared with the younger patients (p=0.014).
Early enteral nutritional therapy and the adequacy for both energy and protein of the nutritional volume infused were in accordance with the established guidelines. Possible inadequacies of energy and protein balance appeared to be associated with an acute inflammatory response, which was characterized by elevated C-reactive protein levels. The main cause of interruption of the enteral nutritional therapy was the time spent in extubation.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):97-105
DOI 10.1590/S0103-507X2012000100015
This article reviews the literature, organizes the major findings, and generates the best evidence-based recommendations on nutrition therapy for head trauma patients. Despite recent advances in head trauma diagnosis and therapy, the mortality associated with this condition remains high. Few therapeutic interventions have been proven to effectively improve this condition. Head trauma causes multiple metabolic and electrolytic disorders; it is characterized by a hypermetabolic state that is associated with intensive catabolism, leading to specific nutritional needs. The current literature lacks specific guidelines for nutrition therapy in severe head trauma patients, although a substantial amount of data has been reported and relevant issues are currently being studied; these data may allow better nutrition therapy guidelines for these patients. In addition to a well-trained multi-disciplinary team, the following recommendations appear to improve outcomes: introducing nutrition therapy early; preferred enteral administration; appropriate energy intake; formulations that are tailored to specific patients, including appropriate nutrients; and strict electrolytic and metabolic monitoring. Understanding the pathophysiology and the consequences of therapy is fundamental.
Abstract
Rev Bras Ter Intensiva. 2008;20(3):286-295
DOI 10.1590/S0103-507X2008000300012
Considering the importance and the difficulties inherent to nutritional state assessment, as well as the results interpretation and the inexistence of specific and validated guidelines related to applied methods to the severely ill patient, the present revision aims to contribute to the analysis and recommendation of efficient methods, which are suitable to use and reliable in terms of interpretation in the context of the severely ill patient. The presence of edema and unspecific alterations in the plasmatic concentrations of proteins; altered anthropometrics variables reflecting more the rearrangement of the total body water than the nutritional state changes; inconclusive studies with electric bioimpedance; absence of data related to the application of the global subjective assessment to severely ill patients; altered biochemical markers as a consequence of the metabolic changes that, among others, indicate several method limitations to these patients. Notwithstanding the lack of studies to validate the various methods, recommendations based on clinical evidences, observation and physiopathology alterations are available. Independent from the methods, clinical observation by the health staff at all stages is mandatory. It is crucial to dedicate more efforts to identify methods and their specificity to detection, risk assessment or monitoring.