Abstract
Rev Bras Ter Intensiva. 2020;32(1):66-71
DOI 10.5935/0103-507X.20200011
To temporally assess a painful stimulus in premature infants using 3 neonatal pain scales.
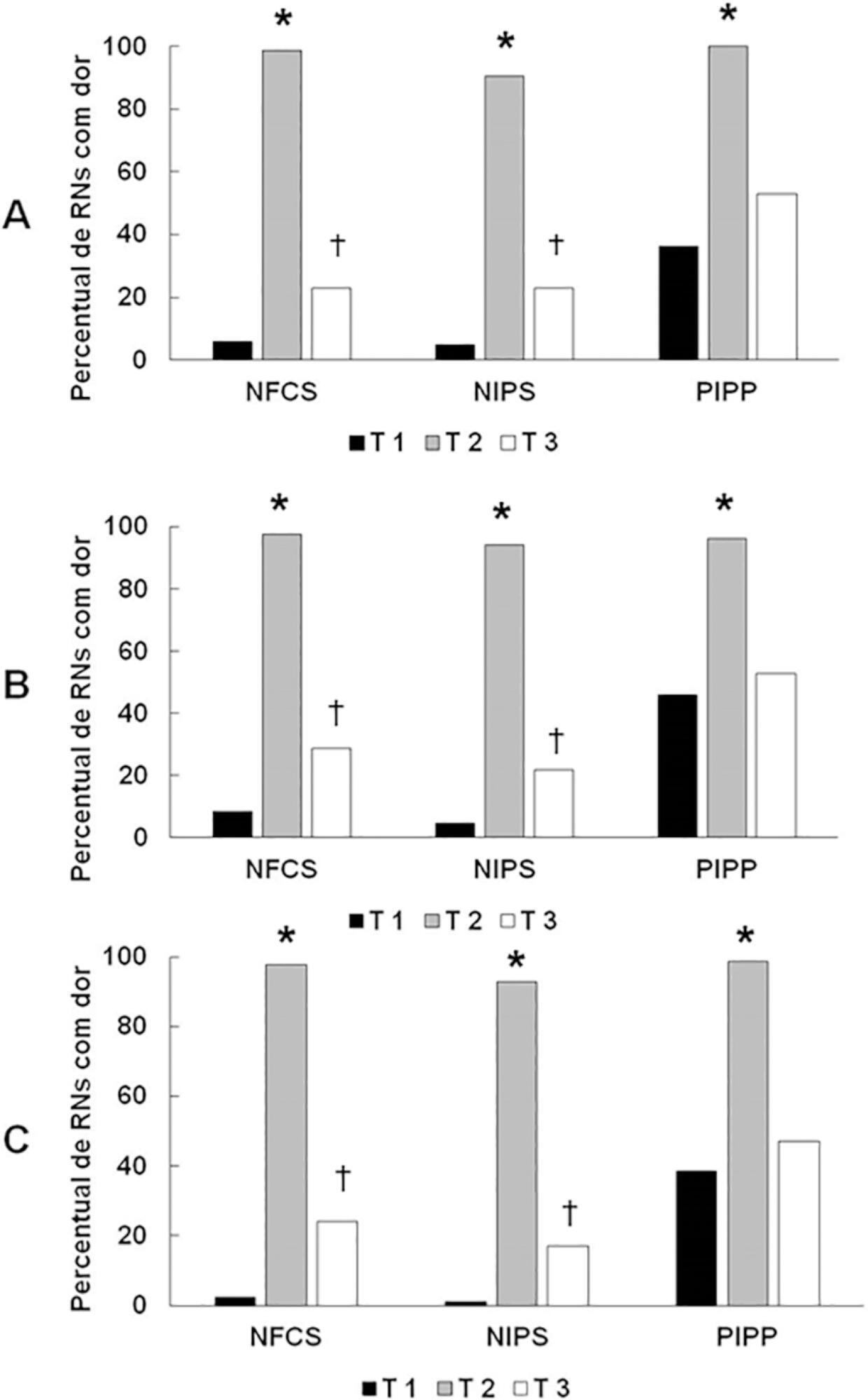
A total of 83 premature infants were observed during airway aspiration by 3 evaluators (E1, E2 and E3) using 3 pain assessment scales (Neonatal Facial Coding System - NFCS; Neonatal Infant Pain Scale - NIPS; and Premature Infant Pain Profile - PIPP) at 5 time points: T1 (before airway aspiration), T2 (during airway aspiration), T3 (1 minute after airway aspiration), T4 (3 minutes after airway aspiration), and T5 (5 minutes after airway aspiration). Light’s Kappa (agreement among examiners and among scales at each time point) and the McNemar test (comparison among time points) were used considering p < 0.05.
There was a significant difference between the 3 examiners for T1 and T2 using the 3 scales. In T3, pain was observed in 22.9%/E1, 28.9%/E2, and 24.1%/E3 according to the NFCS; 22.9%/E1, 21.7%/E2, and 16.9%/E3 according to the NIPS; and 49.4%/E1, 53.9%/E2, and 47%/E3 according to the PIPP. There was a difference between T1 and T3 using the 3 scales, except for 2 examiners for the PIPP (E2: p = 0.15/E3: p = 0.17). Comparing T4 and T5 to T1, there was no difference in the 3 scales.
Premature infants required at least 3 minutes to return to their initial state of rest (no pain).
Abstract
Rev Bras Ter Intensiva. 2016;28(1):27-32
DOI 10.5935/0103-507X.20160010
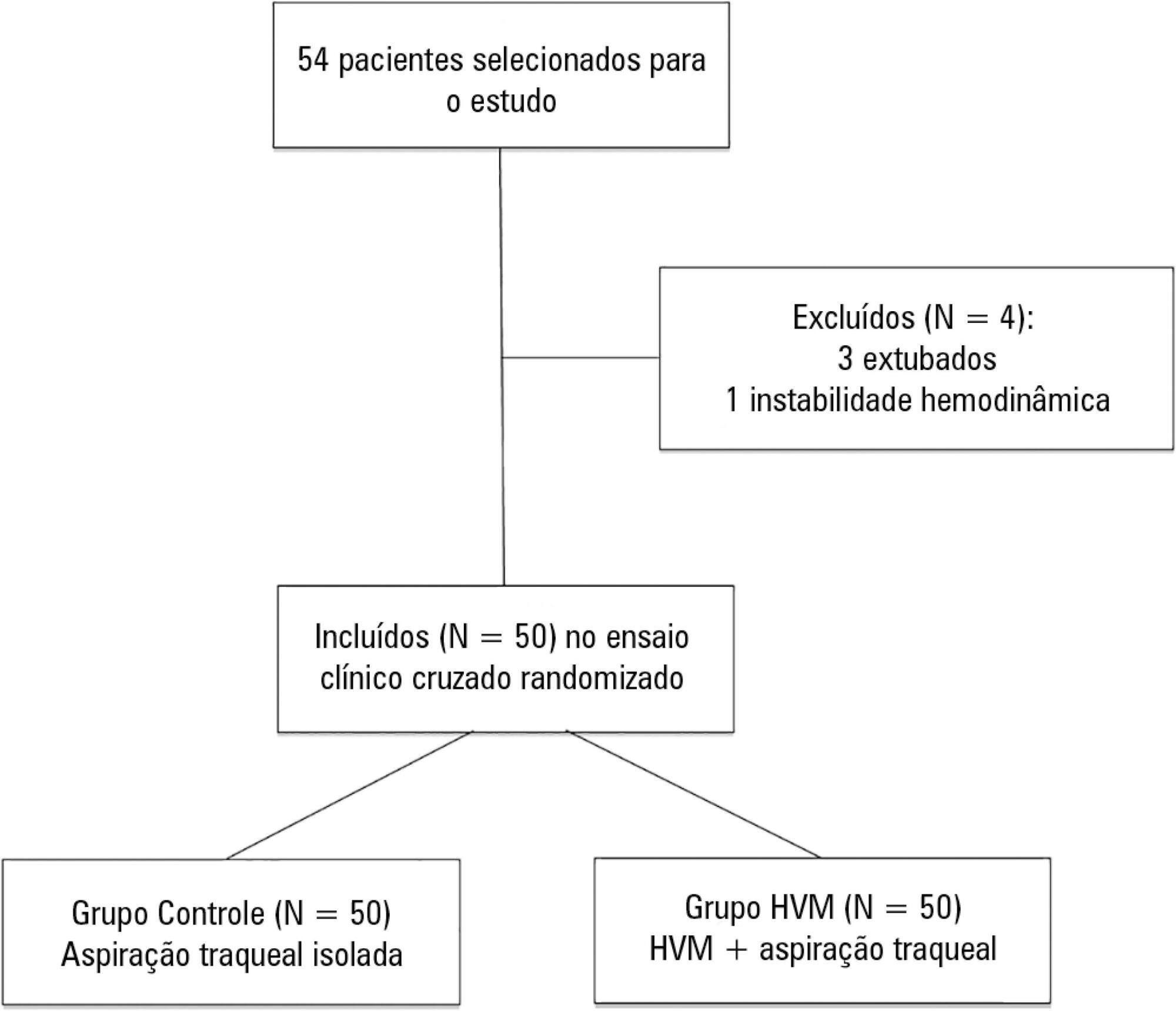
To determine the efficacy of lung hyperinflation maneuvers via a mechanical ventilator compared to isolated tracheal aspiration for removing secretions, normalizing hemodynamics and improving lung mechanics in patients on mechanical ventilation.
This was a randomized crossover clinical trial including patients admitted to the intensive care unit and on mechanical ventilation for more than 48 hours. Patients were randomized to receive either isolated tracheal aspiration (Control Group) or lung hyperinflation by mechanical ventilator (MVH Group). Hemodynamic and mechanical respiratory parameters were measured along with the amount of aspirated secretions.
A total of 50 patients were included. The mean age of the patients was 44.7 ± 21.6 years, and 31 were male. Compared to the Control Group, the MVH Group showed greater aspirated secretion amount (3.9g versus 6.4g, p = 0.0001), variation in mean dynamic compliance (-1.3 ± 2.3 versus -2.9 ± 2.3; p = 0.008), and expired tidal volume (-0.7 ± 0.0 versus -54.1 ± 38.8, p = 0.0001) as well as a significant decrease in peak inspiratory pressure (0.2 ± 0.1 versus 2.5 ± 0.1; p = 0.001).
In the studied sample, the MVH technique led to a greater amount of aspirated secretions, significant increases in dynamic compliance and expired tidal volume and a significant reduction in peak inspiratory pressure.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):115-122
DOI 10.5935/0103-507X.20130022
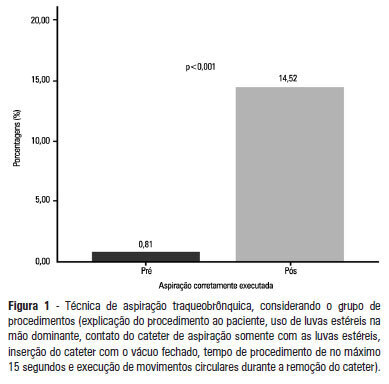
OBJECTIVE: To evaluate the effectiveness of an educational intervention on healthcare professionals' adherence to the technical recommendations for tracheobronchial aspiration in intensive care unit patients. METHODS: A quasi-experimental study was performed to evaluate intensive care unit professionals' adherence to the tracheobronchial aspiration technical recommendations in intensive care unit patients both before and after a theoretical and practical educational intervention. Comparisons were performed using the chi-square test, and the significance level was set to p<0.05. RESULTS: A total of 124 procedures, pre- and post-intervention, were observed. Increased adherence was observed in the following actions: the use of personal protective equipment (p=0.01); precaution when opening the catheter package (p<0.001); the use of a sterile glove on the dominant hand to remove the catheter (p=0.003); the contact of the sterile glove with the catheter only (p<0.001); the execution of circular movements during the catheter removal (p<0.001); wrapping the catheter in the sterile glove at the end of the procedure (p=0.003); the use of distilled water, opened at the start of the procedure, to wash the connection latex (p=0.002); the disposal of the leftover distilled water at the end of the procedure (p<0.001); and the performance of the aspiration technique procedures (p<0.001). CONCLUSION: There was a low adherence by health professionals to the preventive measures against hospital infection, indicating the need to implement educational strategies. The educational intervention used was shown to be effective in increasing adherence to the technical recommendations for tracheobronchial aspiration.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):401-406
DOI 10.1590/S0103-507X2012000400018
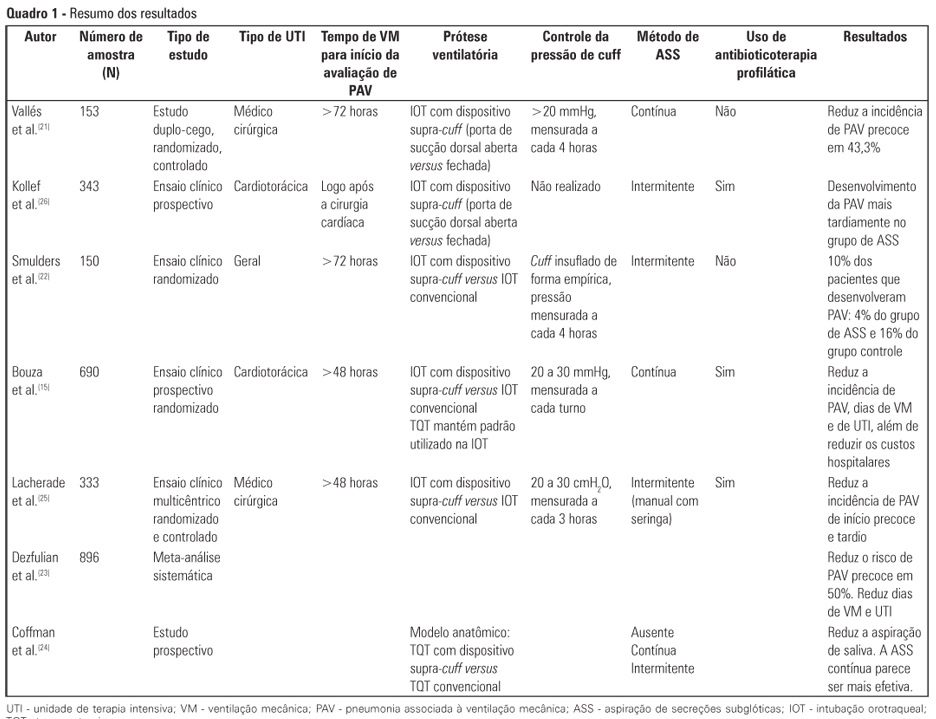
Critically ill patients are intubated or tracheostomized because, in most cases, these individuals require invasive mechanical ventilation. The cannulae that are used include the cuff, which can act as a reservoir for oropharyngeal secretions, predisposing to ventilator-associated pneumonia. Studies have revealed that the suction of subglottic secretions through the dorsal suction lumen above the endotracheal tube cuff delays the onset and reduces the incidence of ventilator-associated pneumonia. The aim of this review is to assess published studies regarding the significance of using suction with a supra-cuff device for the prevention of ventilator-associated pneumonia in critically ill patients treated with orotracheal intubation or tracheostomy. Therefore, by searching national and international databases, a literature review was undertaken of studies published between the years 1986 and 2011. Few results were found relating the suction of subglottic secretions to decreased duration of mechanical ventilation and length of stay in the intensive care unit. The suction of subglottic secretions is ineffective in decreasing mortality but is effective in reducing the incidence of early-onset ventilator-associated pneumonia and hospital costs. Techniques involving continuous suction of subglottic secretions may be particularly efficient in removing secretions; however, intermittent suction appears to be the least harmful method. In conclusion, cannulae with a supra-cuff suction device enable the aspiration of subglottic secretions, providing benefits to critically ill patients by reducing the incidence of ventilator-associated pneumonia and, consequently, hospital costs - with no large-scale adverse effects.
Abstract
Rev Bras Ter Intensiva. 2011;23(2):190-198
DOI 10.1590/S0103-507X2011000200012
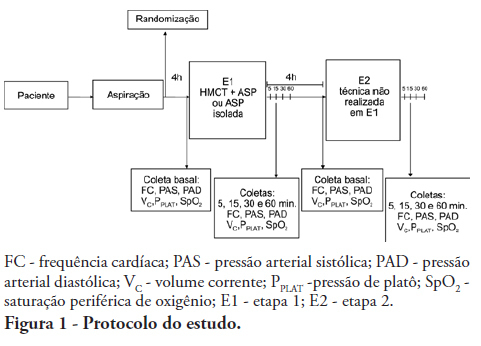
OBJECTIVES: To evaluate the effects of the manual hyperinflation with thoracic compression (MHTC) maneuver on the clearance of secretions, pulmonary mechanics, hemodynamics and oxygenation in mechanically ventilated patients. METHODS: This was a controlled, crossover study that included twenty patients who were under invasive ventilation for more than 48 hours. Four hours after the last airway suctioning procedure, the patients underwent the study interventions, Suction alone or MHTC plus Suction, in sequence at four hour intervals. The sequence order for the procedures was established by randomization. Data were collected before, during and 5, 15, 30 and 60 minutes after each intervention. The suctioned secretions were collected and weighed. RESULTS: No significant differences between the procedures were found regarding tidal volume, plateau pressure and pulmonary compliance (p>0.05). The hemodynamic variables showed increased pressures and heart rate during the procedures and returned to baseline values five minutes after the end of the procedure (p≤0.001). No significant hemodynamic differences were seen between the interventions (p>0.05). For the duration of the study, oxygen saturation was 99% with only two exceptions during the MHTC + Suction procedure, where saturation was 98% (p<0.05). No significant differences were observed between the techniques regarding the weight of the suctioned secretion. CONCLUSION: The results suggest that MHTC, as performed in this study, adds no benefit with respect to oxygenation optimization, pulmonary mechanics and clearance of secretions. However, the MHTC maneuver did not result in hemodynamic changes when compared to the suctioning procedure alone.
Abstract
Rev Bras Ter Intensiva. 2009;21(1):80-88
DOI 10.1590/S0103-507X2009000100012
Pneumonia is the most common nosocominal infection in intensive care units and mechanical ventilation is a significant factor associated to its development. The objective of this study was to describe the impact of the open and closed tracheal suction systems on the incidence of ventilation-associated pneumonia. A search in the Pubmed database was performed to identify randomized controlled trials, published from 1990 to November 2008. Nine studies were included. Of the studies reviewed, seven did not disclose any significant advantages of using the closed system when compared to th e open, whereas two reported that use of the closed system increased colonization rates but not incidence of ventilation-associated pneumonia and one observed that use of the closed system did not increase colonization of the respiratory tract but reduced the spread of infection resulting in decreased sepsis rates. Only two studies found a reduction in the incidence of ventilation-associated pneumonia with use of the closed system, and one revealed a 3.5 times greater risk of developing this infection with the open system. Results suggest that the impact of the open and closed tracheal suction system is similar on development of ventilation-associated pneumonia, choice of the suction system should therefore be based on other parameters. While the closed system increases risk of colonization of the respiratory tract, but has the advantages of continuing mechanical ventilation and lessening hemodynamic impairment.
Abstract
Rev Bras Ter Intensiva. 2008;20(4):331-338
DOI 10.1590/S0103-507X2008000400003
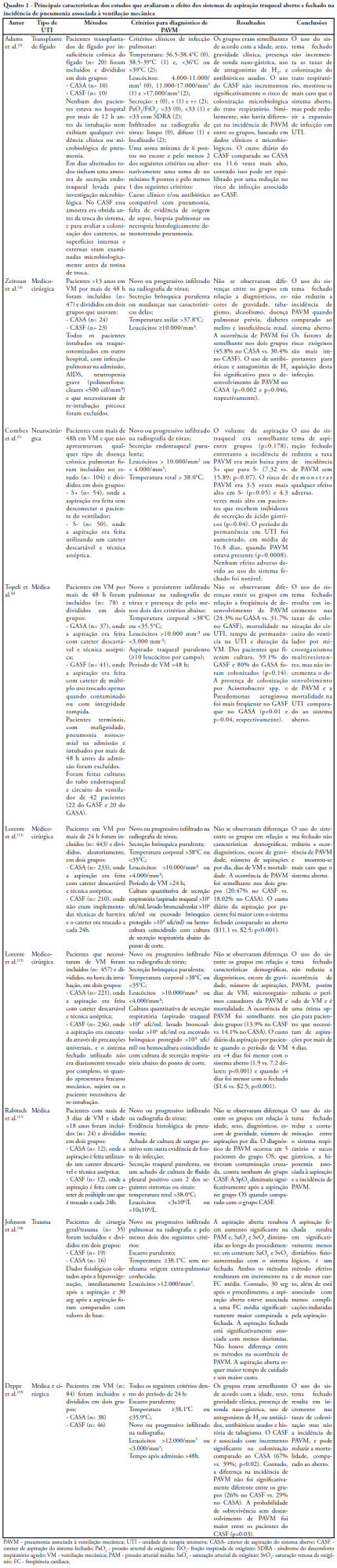
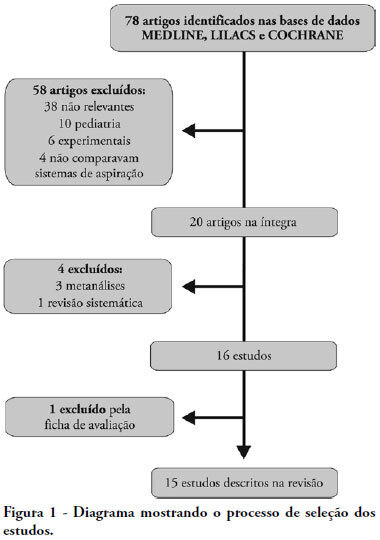
OBJECTIVES: This study attempted to identify which is the more effective suction system. The objective was to compare open versus closed suction systems according to a systematic review. METHODS: A search of scientific literature was conducted in MedLine, LILACS and Cochrane between 1997 and August 2007 using the key words: endotracheal suction and closed suction. Included were articles that compared the open and closed suction systems used in adult humans and that were randomized and controlled trials. RESULTS: From the 78 articles identified, only 15 were accepted and described in this review. Nine compared incidence of ventilator-associated pneumonia, six compared oxygen saturation, four compared blood pressure and heart rate, three compared pulmonary volumes, two compared secretion removal and four compared costs. No difference was found in these variables compared: incidence of ventilator associated pneumonia, mortality, intensive care unit length of stay, duration of mechanical ventilation, PaCO2, PaO2, mean blood pressure, heart rate and secretion removal. However, there were always SpO2 and pulmonary volume decreases when using the open suction system; and costs were lower in most of the studies that used the closed suction system. CONCLUSIONS: Closed suction system seems to increase the risk of colonization, but has the advantage of not reducing the pulmonary volumes and not entailing a drop of saturation, especially in patients with severe respiratory failure and in the use of higher levels of positive end expiratory pressure.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)