Abstract
Rev Bras Ter Intensiva. 2020;32(1):66-71
DOI 10.5935/0103-507X.20200011
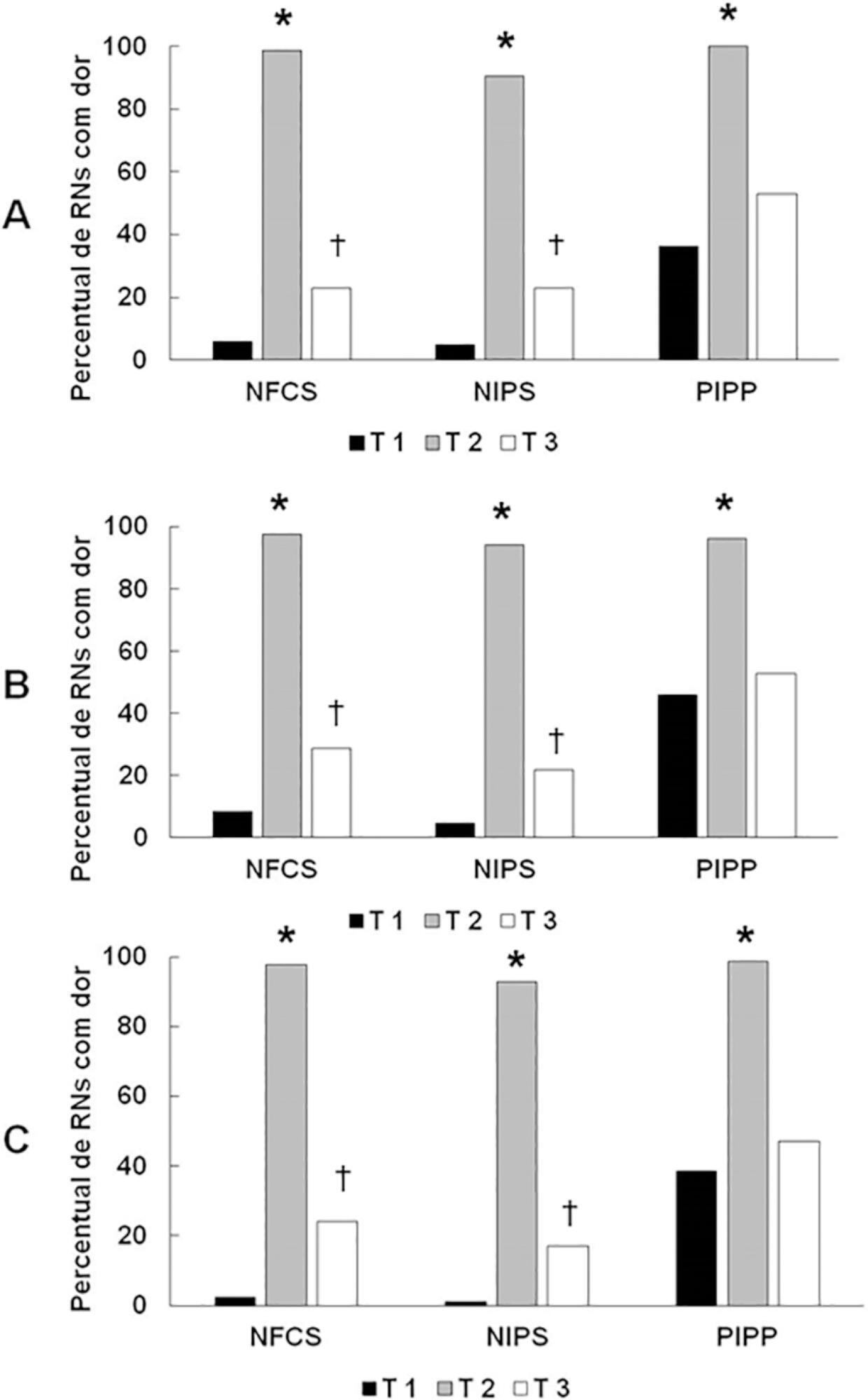
To temporally assess a painful stimulus in premature infants using 3 neonatal pain scales.
A total of 83 premature infants were observed during airway aspiration by 3 evaluators (E1, E2 and E3) using 3 pain assessment scales (Neonatal Facial Coding System - NFCS; Neonatal Infant Pain Scale - NIPS; and Premature Infant Pain Profile - PIPP) at 5 time points: T1 (before airway aspiration), T2 (during airway aspiration), T3 (1 minute after airway aspiration), T4 (3 minutes after airway aspiration), and T5 (5 minutes after airway aspiration). Light’s Kappa (agreement among examiners and among scales at each time point) and the McNemar test (comparison among time points) were used considering p < 0.05.
There was a significant difference between the 3 examiners for T1 and T2 using the 3 scales. In T3, pain was observed in 22.9%/E1, 28.9%/E2, and 24.1%/E3 according to the NFCS; 22.9%/E1, 21.7%/E2, and 16.9%/E3 according to the NIPS; and 49.4%/E1, 53.9%/E2, and 47%/E3 according to the PIPP. There was a difference between T1 and T3 using the 3 scales, except for 2 examiners for the PIPP (E2: p = 0.15/E3: p = 0.17). Comparing T4 and T5 to T1, there was no difference in the 3 scales.
Premature infants required at least 3 minutes to return to their initial state of rest (no pain).
Abstract
Rev Bras Ter Intensiva. 2019;31(3):312-317
DOI 10.5935/0103-507X.20190056
To investigate the influence of respiratory distress syndrome management on clinical and echocardiographic parameters used for hemodynamic evaluation in ≤ 32- week newborns.
Thirty-three ≤ 32-week newborns were prospectively evaluated and subjected to invasive mechanical ventilation. The need for exogenous surfactant and clinical and echocardiographic parameters in the first 24 hours of life was detailed in this group of patients.
The mean airway pressure was significantly higher in newborn infants who required inotropes [10.8 (8.8 - 23) cmH2O versus 9 (6.2 - 12) cmH2O; p = 0.04]. A negative correlation was found between the mean airway pressure and velocity-time integral of the pulmonary artery (r = -0.39; p = 0.026), right ventricular output (r = -0.43; p = 0.017) and measurements of the tricuspid annular plane excursion (r = -0.37; p = 0.036). A negative correlation was found between the number of doses of exogenous surfactant and the right ventricular output (r = -0.39; p = 0.028) and pulmonary artery velocity-time integral (r = -0.35; p = 0.043).
In ≤ 32-week newborns under invasive mechanical ventilation, increases in the mean airway pressure and number of surfactant doses are correlated with the worsening of early cardiac function. Therefore, more aggressive management of respiratory distress syndrome may contribute to the hemodynamic instability of these patients.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):347-353
DOI 10.5935/0103-507X.20190047
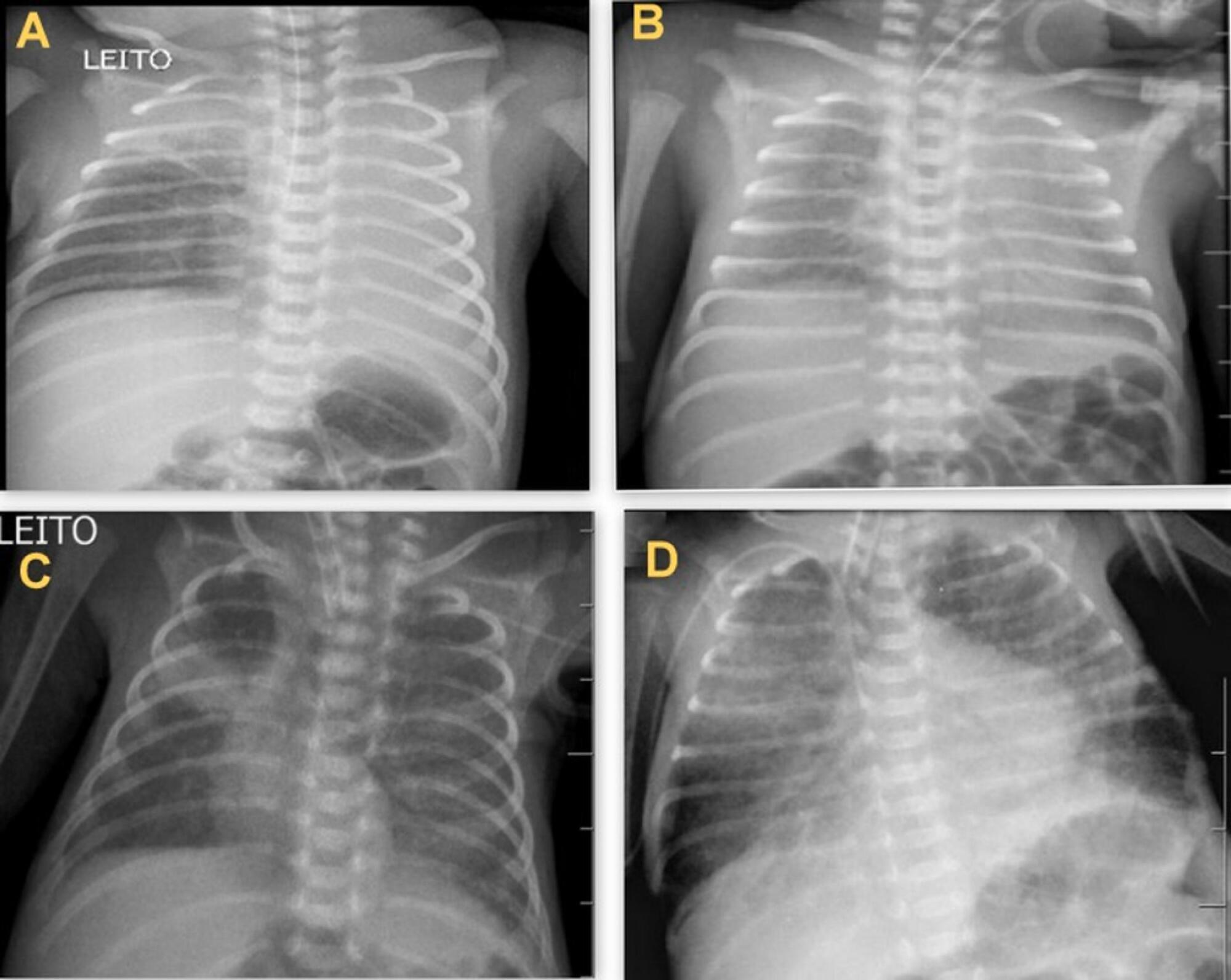
To determine the occurrence and characteristics of atelectasis, opacities, hypolucency and pulmonary infiltrates observed on chest X-rays of preterm infants in a neonatal intensive care unit.
This was a cross-sectional observational study. From August to December 2017, all chest radiographs of newborn infants were analyzed. The study included the chest radiographs of preterm neonates with gestational ages up to 36 weeks in the neonatal period that showed clear changes or suspected changes, which were confirmed after a radiologist’s report. Radiological changes were associated with possible predisposing factors.
During the study period, 450 radiographs were performed on preterm neonates, and 37 lung changes were identified and classified into 4 types: 12 (2.66%) changes were described as opacities, 11 (2.44%) were described as atelectasis, 10 (2.22%) were described as pulmonary infiltrate, and 4 (0.88%) were described as hypolucency. A higher occurrence of atelectasis was noted in the right lung (81.8%). Among the abnormal radiographs, 25 (67.6%) newborn infants were receiving invasive mechanical ventilation.
Considering the radiological report, no significance was found for the observed changes. Atelectasis was not the most frequently observed change. The predisposing factors for these changes were extreme prematurity, low weight, male sex, a poorly positioned endotracheal tube and the use of invasive mechanical ventilation.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):174-180
DOI 10.5935/0103-507X.20180023
To compare the neuropsychomotor development in the first year of life of premature infants with and without bronchopulmonary dysplasia.
A cross-sectional retrospective study was conducted between January 1, 2014, and December 30, 2015, with premature infants weighing < 1,500g at birth and diagnosed with bronchopulmonary dysplasia at the corrected ages of 6 and 9 months, assessed using the DENVER II Developmental Screening Test. Quantitative variables were described as the means, medians and standard deviations. Variables with normal distribution were tested using Student's t test; otherwise, the Mann-Whitney test was used, considering significance at p-value < 0.05. Qualitative variables were expressed as frequencies and percentages. Logistic regression was used with odds ratio analysis to evaluate the effects of other variables as risk factors for changes in neuropsychomotor development.
Infants with bronchopulmonary dysplasia showed greater developmental delay compared with those without bronchopulmonary dysplasia (p-value = 0.001). The factors associated with a higher incidence of changes in neuropsychomotor development, in addition to bronchopulmonary dysplasia, were antenatal steroid, gender, birth weight, 5-minute Apgar score, Score for Neonatal Acute Physiology-Perinatal Extension, duration of oxygen therapy, duration of mechanical ventilation and length of hospital stay. Other variables may also have influenced the result, such as drug use by mothers of infants with bronchopulmonary dysplasia.
Bronchopulmonary dysplasia associated with other pre- and postnatal factors may be considered a risk factor for delayed neuropsychomotor development in the first year of life in premature infants born weighing less than 1,500g.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):57-64
DOI 10.5935/0103-507X.20140009
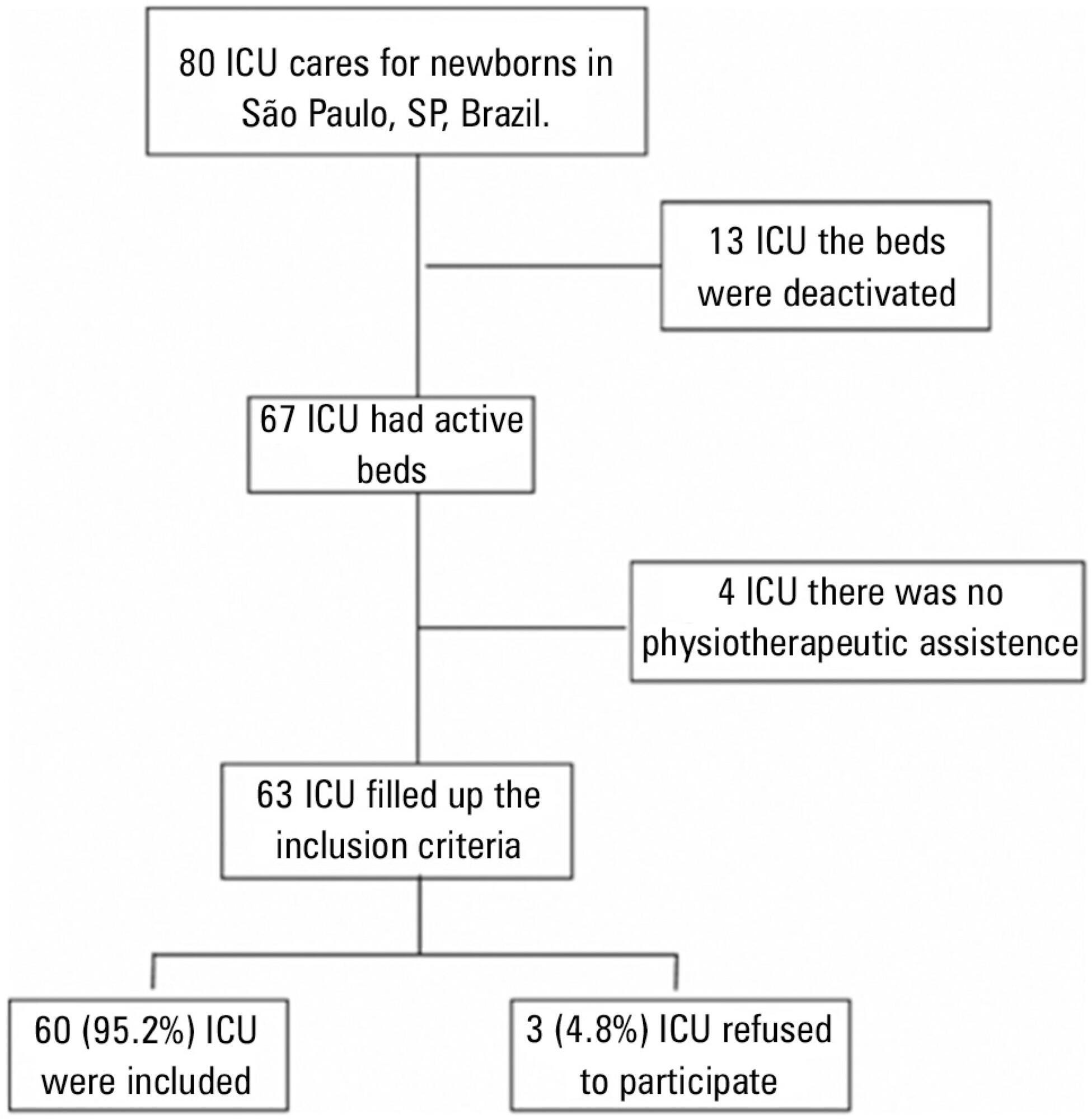
To describe the characteristics of physical therapy assistance to newborns and to provide a profile of physical therapists working in intensive care units in the city of São Paulo, Brazil.
This cross-sectional study was conducted in every hospital in São Paulo city that had at least one intensive care unit bed for newborns registered at the National Registry of Health Establishments in 2010. In each unit, three types of physical therapists were included: an executive who was responsible for the physical therapy service in that hospital (chief-physical therapists), a physical therapist who was responsible for the physical therapy assistance in the neonatal unit (reference-physical therapists), and a randomly selected physical therapist who was directly involved in the neonatal care (care-physical therapists).
Among the 67 hospitals eligible for the study, 63 (94.0%) had a physical therapy service. Of those hospitals, three (4.8%) refused to participate. Thus, 60 chief-PTs, 52 reference-physical therapists, and 44 care-physical therapists were interviewed. During day shifts, night shifts, and weekends/holidays, there were no physical therapists in 1.7%, 45.0%, and 13.3% of the intensive care units, respectively. Physical therapy assistance was available for 17.8±7.2 hours/day, and each physical therapist cared for 9.4±2.6 newborns during six working hours. Most professionals had completed at least one specialization course.
Most neonatal intensive care units in the city of São Paulo had physical therapists working on the day shift. However, other shifts had incomplete staff with less than 18 hours of available physical therapy assistance per day.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):386-392
DOI 10.1590/S0103-507X2012000400016
OBJECTIVE: To analyze the process of care provided to premature infants in a neonatal intensive care unit and the factors associated with their mortality. METHODS: Cross-sectional retrospective study of premature infants in an intensive care unit between 2008 and 2010. The characteristics of the mothers and premature infants were described, and a bivariate analysis was performed on the following characteristics: the study period and the "death" outcome (hospital, neonatal and early) using Pearson's chi-square test, Fisher's exact test or a chi-square test for linear trends. Bivariate and multivariable logistic regression analyses were performed using a stepwise backward logistic regression method between the variables with p<0.20 and the "death" outcome. A p value <0.05 was considered to be significant. RESULTS: In total, 293 preterm infants were studied. Increased access to complementary tests (transfontanellar ultrasound and Doppler echocardiogram) and breastfeeding rates were indicators of improving care. Mortality was concentrated in the neonatal period, especially in the early neonatal period, and was associated with extreme prematurity, small size for gestational age and an Apgar score <7 at 5 minutes after birth. The late-onset sepsis was also associated with a greater chance of neonatal death, and antenatal corticosteroids were protective against neonatal and early deaths. CONCLUSIONS: Although these results are comparable to previous findings regarding mortality among premature infants in Brazil, the study emphasizes the need to implement strategies that promote breastfeeding and reduce neonatal mortality and its early component.
Abstract
Rev Bras Ter Intensiva. 2012;24(3):224-229
DOI 10.1590/S0103-507X2012000300004
OBJECTIVE: This study analyzed the factors that are associated with the need for packed red blood cell transfusions in premature infants in a neonatal intensive care unit. METHODS: This study is a cross-sectional study of secondary data from premature infants who were admitted to a neonatal intensive care unit between 2008 and 2010. Premature infants with low birth weight were included. Packed red blood cell transfusion was the dependent variable. Pearson's Chi-square or Fisher's exact tests were used for data analysis, and the median, minimum, and maximum values were calculated. Prevalence ratios were calculated using the Poisson regression and Pearson correlation coefficient. Linear regression analyses were performed. P < 0.05 was considered to be significant. RESULTS: We examined 254 premature infants, and 39.4% of this sample received packed red blood cells. Transfusions were 70% less prevalent in premature infants who were born at >32 weeks of gestation, and 191% more prevalent in infants who exhibited late-onset neonatal sepsis. The number of transfusions per patient was negatively correlated with gestational age and positively correlated with late-onset neonatal sepsis. A gestational age <32 weeks and late-onset neonatal sepsis explained 45% of the transfusions (p<0.0001). CONCLUSIONS: Premature infants with a gestational age <32 weeks and who developed late-onset neonatal sepsis exhibited a greater need for packed red blood cell transfusions.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)