Abstract
Rev Bras Ter Intensiva. 2012;24(2):179-183
DOI 10.1590/S0103-507X2012000200014
OBJECTIVE:The aim of the present study was to evaluate the prevalence and factors associated with bronchopulmonary dysplasia at a neonatal intensive care unit. METHODS: The study was a cross-sectional study that used secondary data from premature infants who were born with less than 32 weeks of gestational age and were admitted to a neonatal intensive care unit. Chi-square, Mann-Whitney and multivariate tests were used. Significance was set at p<0.05. RESULTS: A total of 88 premature infants were included in the study. Bronchopulmonary dysplasia occurred in 27.3% of the infants and was related to having a gestational age below 28 weeks (OR: 4.80; 95% CI: 1.50-15.34; p=0.008) and a patent ductus arteriosus (OR: 3.44; 95% CI: 1.10-10.76; p=0.034). The group with bronchopulmonary dysplasia used mechanical ventilation for a longer duration, with a median of 24.5 days (p<0.0001). At discharge, the corrected and chronological ages were higher in the group with bronchopulmonary dysplasia (p<0.0001), with respective medians of 38.4 weeks and 70.5 days. CONCLUSIONS: In this study, the prevalence of bronchopulmonary dysplasia was high; the high prevalence was related to extreme prematurity, patent ductus arteriosus, a longer period under mechanical ventilation and prolonged hospitalization. The increased survival of infants with low gestational age makes this disorder a public health issue.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):207-210
DOI 10.1590/S0103-507X2012000200018
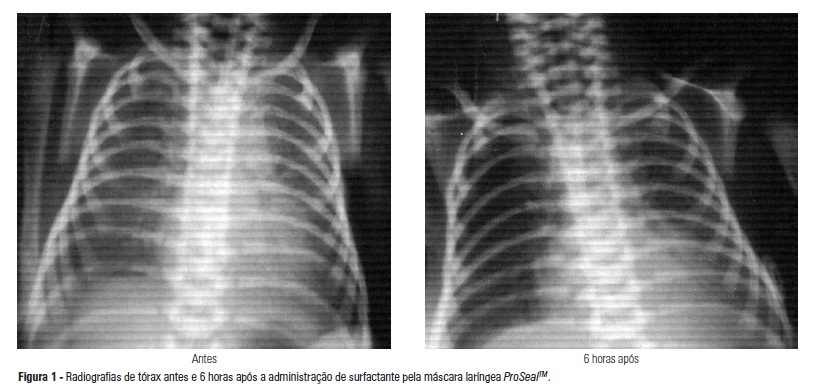
The administration of surfactant via tracheal cannula with mechanical ventilation is the conventional treatment for infant respiratory distress syndrome. Hemodynamic and respiratory changes due to tracheal intubation and the need for premedication justify the search for less invasive alternatives of surfactant administration. The objective of this study was to describe the use of the ProSealTM laryngeal mask airway as an option for the treatment of respiratory distress syndrome in a premature infant born at 31 weeks of gestation, at 1335 g, with respiratory difficulty after the first hour of life and exhibiting the clinical and radiologic features of respiratory distress syndrome. The surfactant was administered with the use of the ProSealTM laryngeal mask airway at 3.5 hours of life. It was well tolerated, with no need for tracheal intubation. Normal gasometry and radiologic improvement were observed after three and six hours of administration. Oxygen administration was suspended after eight days, with no comorbidities at discharge. The laryngeal mask airway seems to be a painless and less invasive alternative to treat respiratory distress syndrome and may reduce the need for tracheal intubation and mechanical ventilation. The efficacy and advantages of this route of treatment should be confirmed in a study of an adequate sample.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):79-85
DOI 10.1590/S0103-507X2012000100012
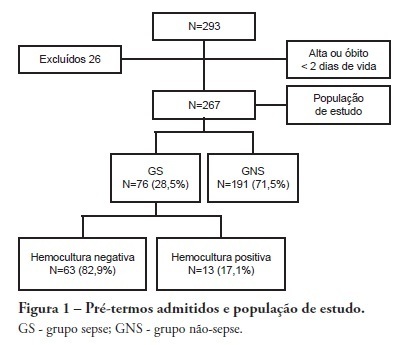
OBJECTIVE: To evaluate the prevalence factors and etiologies associated with late neonatal sepsis in preterm neonates in a neonatal intensive care unit. METHODS: This was a cross-sectional study of secondary data pertaining to preterm neonates admitted to the neonatal intensive care unit between 2008 and 2010 and was gathered from medical charts. The outcome variable, late neonatal sepsis, was characterized using the Brazilian national health surveillance agency criteria. Pearson's Chi-squared test, Fisher's exact test and the linear trend Chi-squared test were used to assess the qualitative variables for linear trends. The statistical significance level was set at p < 0.05. Bivariate and multivariate analyses of the independent and dependent variables were conducted to obtain a measure of the effect and prevalence ratios, considering a p-value of less than 0.20 to indicate statistical significance. RESULTS: This study included 267 preterm neonates. Of the participants, 28.5% were characterized as having late-onset sepsis. Positive blood cultures were recorded for 17.1% of the neonates. Death occurred in 8.2% of the total cases, and of these deaths, 68.2% occurred within the sepsis group. Three deaths were associated with positive blood cultures, all of which grew Gram-negative bacteria. The bivariate analysis demonstrated that as the gestational age and birth weight decreased, the prevalence of late-onset sepsis trended upward. Ten or more days on mechanical ventilation was associated with late-onset neonatal sepsis in 80.8% of cases. Peripherally inserted central catheters left in place for 11 or more days were associated with late-onset neonatal sepsis in 76.2% of cases. The multivariate analysis demonstrated that a peripherally inserted catheter left in place for less than 11 days was associated with late-onset neonatal sepsis. Gram-negative bacteria, including Klebsiella pneumoniae and Escherichia coli, were the most frequent causative agents. CONCLUSIONS: Late sepsis remains a concern because of its prevalence in intensive care units and because it increases the number of invasive procedures that preterm children usually undergo in these units. The authors emphasize the expanding role of Gram-negative bacteria in late-onset neonatal sepsis and the need for more efficient methods to identify confirmed sepsis.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):159-165
DOI 10.1590/S0103-507X2010000200010
OBJECTIVE: Neonates mechanic ventilation weaning has become a major clinical challenge, and constitutes a large portion of neonatal intensive care units workload. The spontaneous breathing trial (SBT), performed immediately before extubation, can provide useful information on the patient's spontaneous breathing ability. This study aimed to assess the SBT effectiveness for extubation success prediction in mechanically ventilated preterm infants. METHODS: After Ethics Committee approval, an observational, longitudinal, prospective study was conducted. A sample of 60 preterm infants compliant with the weaning criteria was categorized in two groups: 'SBT' group (n=30), with the patients who underwent 30 minutes spontaneous breathing trial (SBT) with continuous positive pressure airway (CPAP), and the control group (n=30) where the extubation was performed without spontaneous breathing trial. The heart rate (HR), respiratory rate (RR), pulse oxymetry oxygen saturation (SpO2) and the Silverman-Andersen score were recorded before and 10, 20 and 30 minutes after the spontaneous breathing trial. Were also assessed for both groups, and versus extubation success or failure, the weight, gestational age, Apgar score, mean airway pressure, inspired oxygen concentration, and tracheal tube time. The Chi-square test was used for categorical variables and the Mann-Whitney test for non-normal distribution. Extubation success was defined as a 48 hours period with no reintubation requirement. RESULTS: No significant differences were identified between the groups for the analyzed variables, except for the mean airway pressure. A significant association was shown between spontaneous breathing trial and successful extubation. CONCLUSION: The significant association between SBT and extubation success may contribute for prediction of successful weaning in preterm infants.