Abstract
Rev Bras Ter Intensiva. 2021;33(1):154-166
DOI 10.5935/0103-507X.20210017
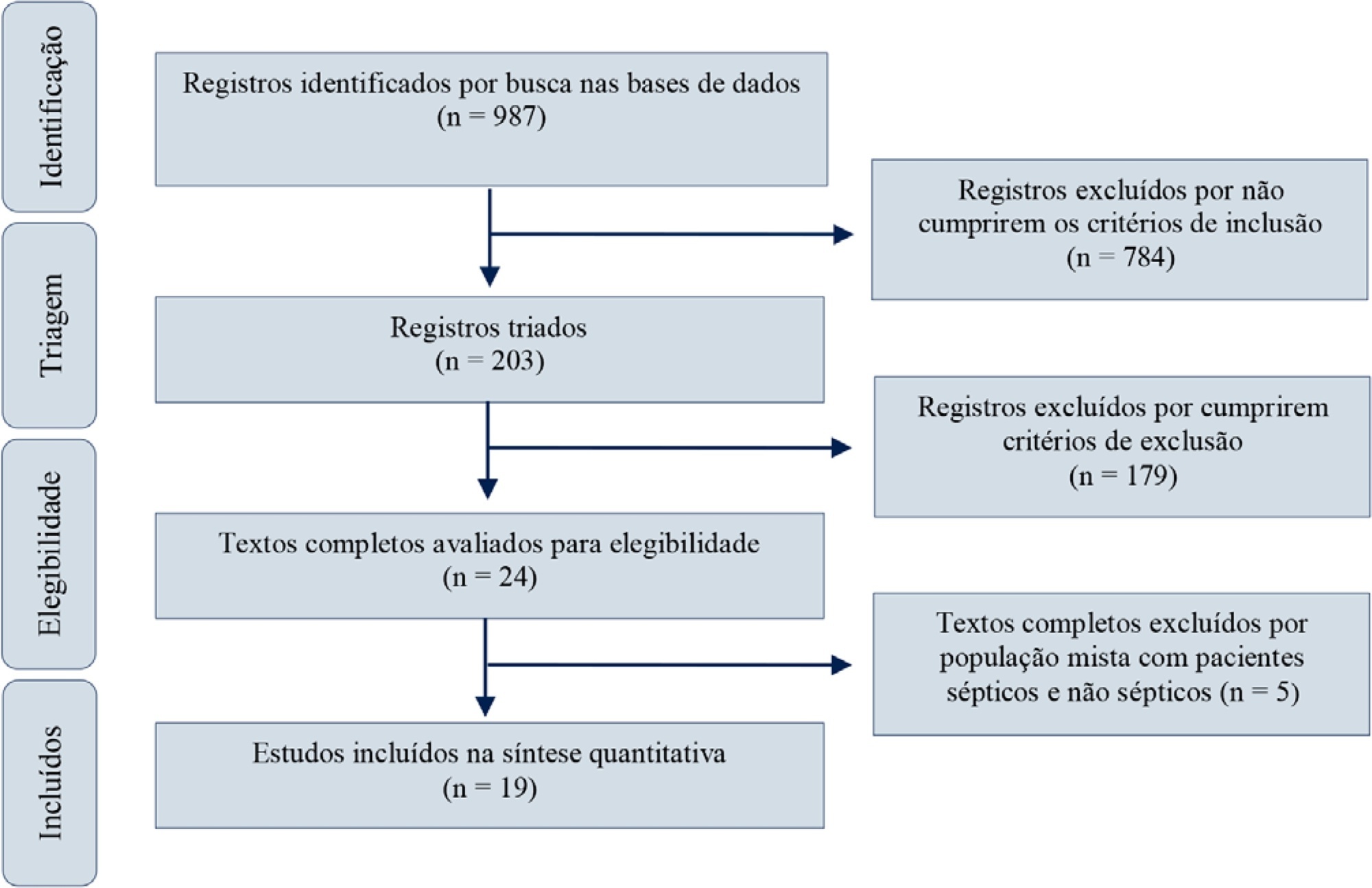
Red blood cell transfusion is thought to improve cell respiration during septic shock. Nevertheless, its acute impact on oxygen transport and metabolism in this condition remains highly debatable. The objective of this study was to evaluate the impact of red blood cell transfusion on microcirculation and oxygen metabolism in patients with sepsis and septic shock. We conducted a search in the MEDLINE®, Elsevier and Scopus databases. We included studies conducted in adult humans with sepsis and septic shock. A systematic review and meta-analysis were performed using the DerSimonian and Laird random-effects model. A p value < 0.05 was considered significant. Nineteen manuscripts with 428 patients were included in the analysis. Red blood cell transfusions were associated with an increase in the pooled mean venous oxygen saturation of 3.7% (p < 0.001), a decrease in oxygen extraction ratio of -6.98 (p < 0.001) and had no significant effect on the cardiac index (0.02L/minute; p = 0,96). Similar results were obtained in studies including simultaneous measurements of venous oxygen saturation, oxygen extraction ratio, and cardiac index. Red blood cell transfusions led to a significant increase in the proportion of perfused small vessels (2.85%; p = 0.553), while tissue oxygenation parameters revealed a significant increase in the tissue hemoglobin index (1.66; p = 0.018). Individual studies reported significant improvements in tissue oxygenation and sublingual microcirculatory parameters in patients with deranged microcirculation at baseline. Red blood cell transfusions seemed to improve systemic oxygen metabolism with apparent independence from cardiac index variations. Some beneficial effects have been observed for tissue oxygenation and microcirculation parameters, particularly in patients with more severe alterations at baseline. More studies are necessary to evaluate their clinical impact and to individualize transfusion decisions.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):36-43
DOI 10.5935/0103-507X.20150007
To evaluate the immediate effects of red blood cell transfusion on central venous oxygen saturation and lactate levels in septic shock patients with different transfusion triggers.
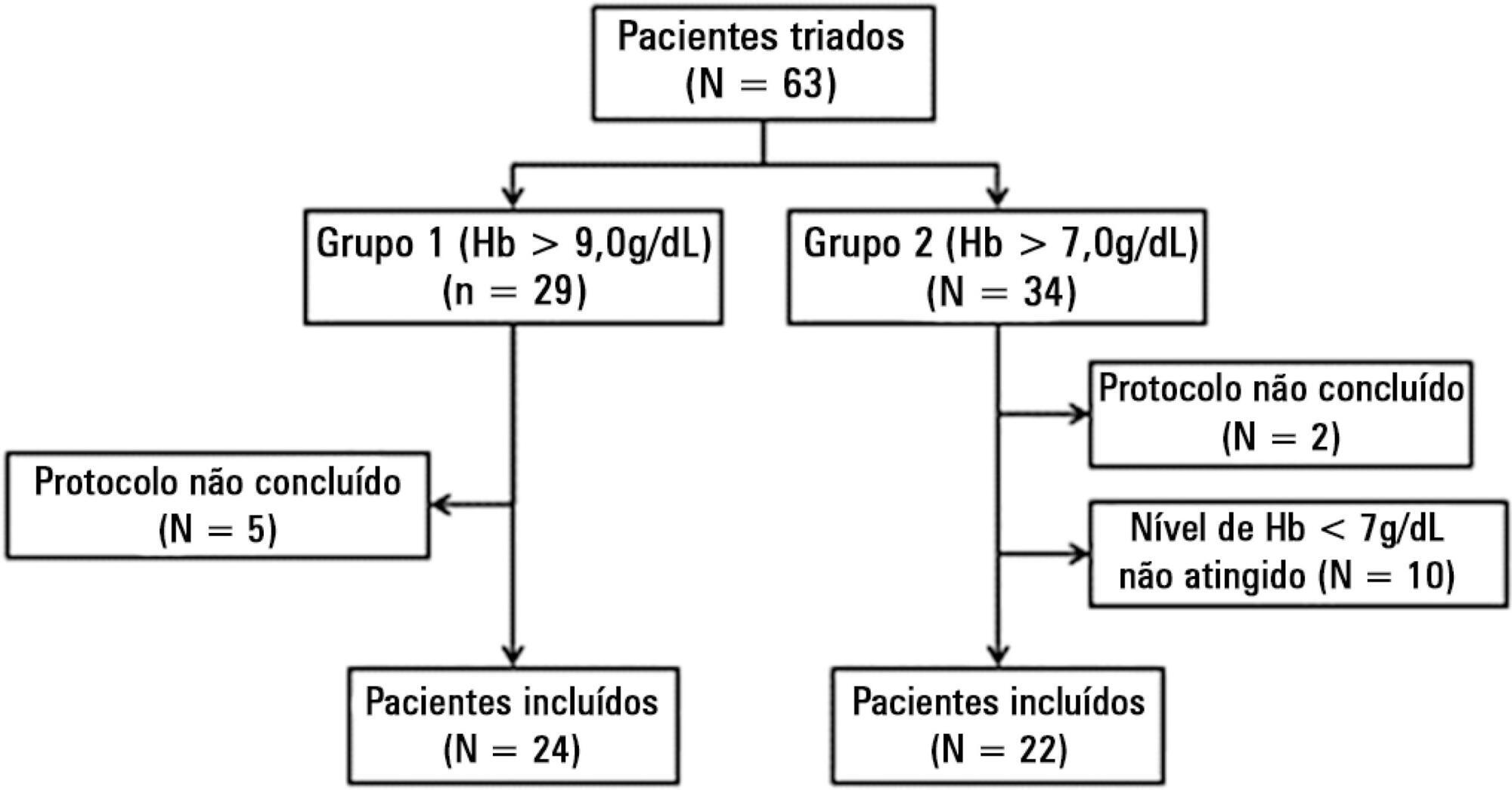
We included patients with a diagnosis of septic shock within the last 48 hours and hemoglobin levels below 9.0g/dL Patients were randomized for immediate transfusion with hemoglobin concentrations maintained above 9.0g/dL (Group Hb9) or to withhold transfusion unless hemoglobin felt bellow 7.0g/dL (Group Hb7). Hemoglobin, lactate, central venous oxygen saturation levels were determined before and one hour after each transfusion.
We included 46 patients and 74 transfusions. Patients in Group Hb7 had a significant reduction in median lactate from 2.44 (2.00 - 3.22) mMol/L to 2.21 (1.80 - 2.79) mMol/L, p = 0.005, which was not observed in Group Hb9 [1.90 (1.80 - 2.65) mMol/L to 2.00 (1.70 - 2.41) mMol/L, p = 0.23]. Central venous oxygen saturation levels increased in Group Hb7 [68.0 (64.0 - 72.0)% to 72.0 (69.0 - 75.0)%, p < 0.0001] but not in Group Hb9 [72.0 (69.0 - 74.0)% to 72.0 (71.0 - 73.0)%, p = 0.98]. Patients with elevated lactate or central venous oxygen saturation < 70% at baseline had a significant increase in these variables, regardless of baseline hemoglobin levels. Patients with normal values did not show a decrease in either group.
Red blood cell transfusion increased central venous oxygen saturation and decreased lactate levels in patients with hypoperfusion regardless of their baseline hemoglobin levels. Transfusion did not appear to impair these variables in patients without hypoperfusion.
Abstract
Rev Bras Ter Intensiva. 2012;24(3):224-229
DOI 10.1590/S0103-507X2012000300004
OBJECTIVE: This study analyzed the factors that are associated with the need for packed red blood cell transfusions in premature infants in a neonatal intensive care unit. METHODS: This study is a cross-sectional study of secondary data from premature infants who were admitted to a neonatal intensive care unit between 2008 and 2010. Premature infants with low birth weight were included. Packed red blood cell transfusion was the dependent variable. Pearson's Chi-square or Fisher's exact tests were used for data analysis, and the median, minimum, and maximum values were calculated. Prevalence ratios were calculated using the Poisson regression and Pearson correlation coefficient. Linear regression analyses were performed. P < 0.05 was considered to be significant. RESULTS: We examined 254 premature infants, and 39.4% of this sample received packed red blood cells. Transfusions were 70% less prevalent in premature infants who were born at >32 weeks of gestation, and 191% more prevalent in infants who exhibited late-onset neonatal sepsis. The number of transfusions per patient was negatively correlated with gestational age and positively correlated with late-onset neonatal sepsis. A gestational age <32 weeks and late-onset neonatal sepsis explained 45% of the transfusions (p<0.0001). CONCLUSIONS: Premature infants with a gestational age <32 weeks and who developed late-onset neonatal sepsis exhibited a greater need for packed red blood cell transfusions.
Abstract
Rev Bras Ter Intensiva. 2011;23(1):30-35
DOI 10.1590/S0103-507X2011000100006
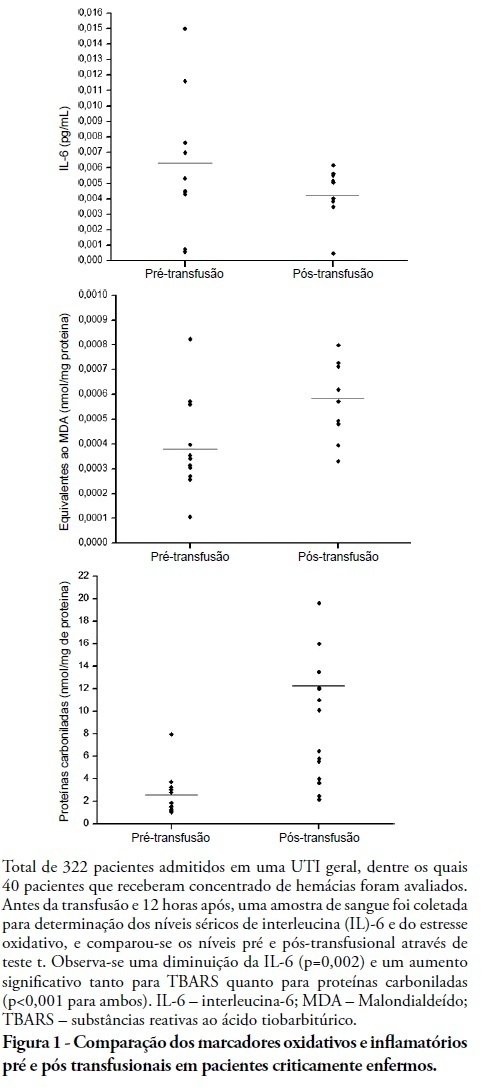
INTRODUCTION: Red blood cell transfusions are common in intensive care units. For many years, transfusions of red blood were thought to have obvious clinical benefits. However, in recent years, the risks and benefits of blood transfusions have been examined more carefully, including the risk of increased morbidity and mortality due to transfusion-related immunomodulation effects. OBJECTIVES: To evaluate red blood cell transfusion effects and the relationship of this procedure to the production of inflammatory cytokines and oxidative damage in critically ill patients admitted to an intensive care unit. METHODS: For 6 months in 2008, we evaluated patients admitted to an intensive care unit who underwent packed red blood cell transfusions. Pre- and post-transfusion levels of interleukin-6, carbonylated proteins and thiobarbituric acid reactive substances were assessed. RESULTS: Serum post-transfusion interleukin-6 levels were reduced, and thiobarbituric acid reactive substances and carbonylated proteins were significantly increased. No statistically significant relationship was found between the levels of pre- and post-transfusion interleukin-6 and thiobarbituric acid reactive substances and the mortality rate. However, there was a significant relationship between levels of post-transfusion carbonylated proteins and mortality. CONCLUSION: Red blood cell transfusion is associated with increased oxidative damage markers and reduced interleukin-6 levels in critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):391-397
DOI 10.1590/S0103-507X2009000400009
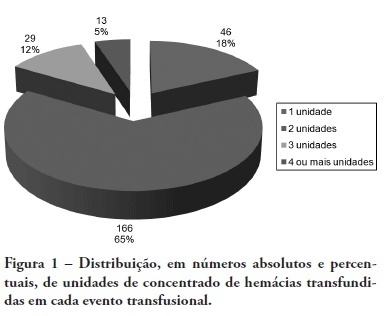
BACKGROUND: The anemia is a common problem upon admission of the patients in the intensive care unit being the red blood cell transfusion a frequent therapeutic. The causes of anemia in critical patients who under go red blood cell transfusion are several: acute loss of blood after trauma, gastrointestinal hemorrhage, surgery amongst others. Currently, few studies are available regarding the use of blood components in patients at intensive care unit. Although blood transfusions are frequent in intensive care unit, the optimized criteria for handling are not clearly defined, with no available guidelines. OBJECTIVES: To analyze the clinical indications of the use of the red blood cell in the intensive care unit. METHODS: The clinical history of the patients admitted in the intensive care unit were analyzed, revisiting which had have red blood cell transfusion in the period between January 1st 2005 and December 31 2005. The study was accepted by the Research Ethics Committee - Comitê de Ética em Pesquisa (CEP) - of the University of South of Santa Catarina (UNISUL). RESULTS: The transfusion rate was 19,33, and the majority of the patients were of the male gender. Their age prevalence was of 60 years old or older. The mortality rate among patients who under went red blood cell transfusion died was of 38,22%. The transfusions criterias were low serum hemoglobin (78%) and the hemoglobin pre - transfusion was 8,11 g/dL. CONCLUSIONS: Politrauma and sepsis/sepsis chock were the pre diagnosis criteria. A low hemoglobin level is the main clinical criteria with average hemoglobin pre - transfusion was 8,11 g/dL.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)