Abstract
Crit Care Sci. 2023;35(2):177-186
DOI 10.5935/2965-2774.20230348-pt
To measure the prognostic value of peripheral ischemic microvascular reserve in the context of persistent sepsis-induced hyperlactatemia and measure its influence on the temporal dynamics of lactate and the strength of association between these variables.
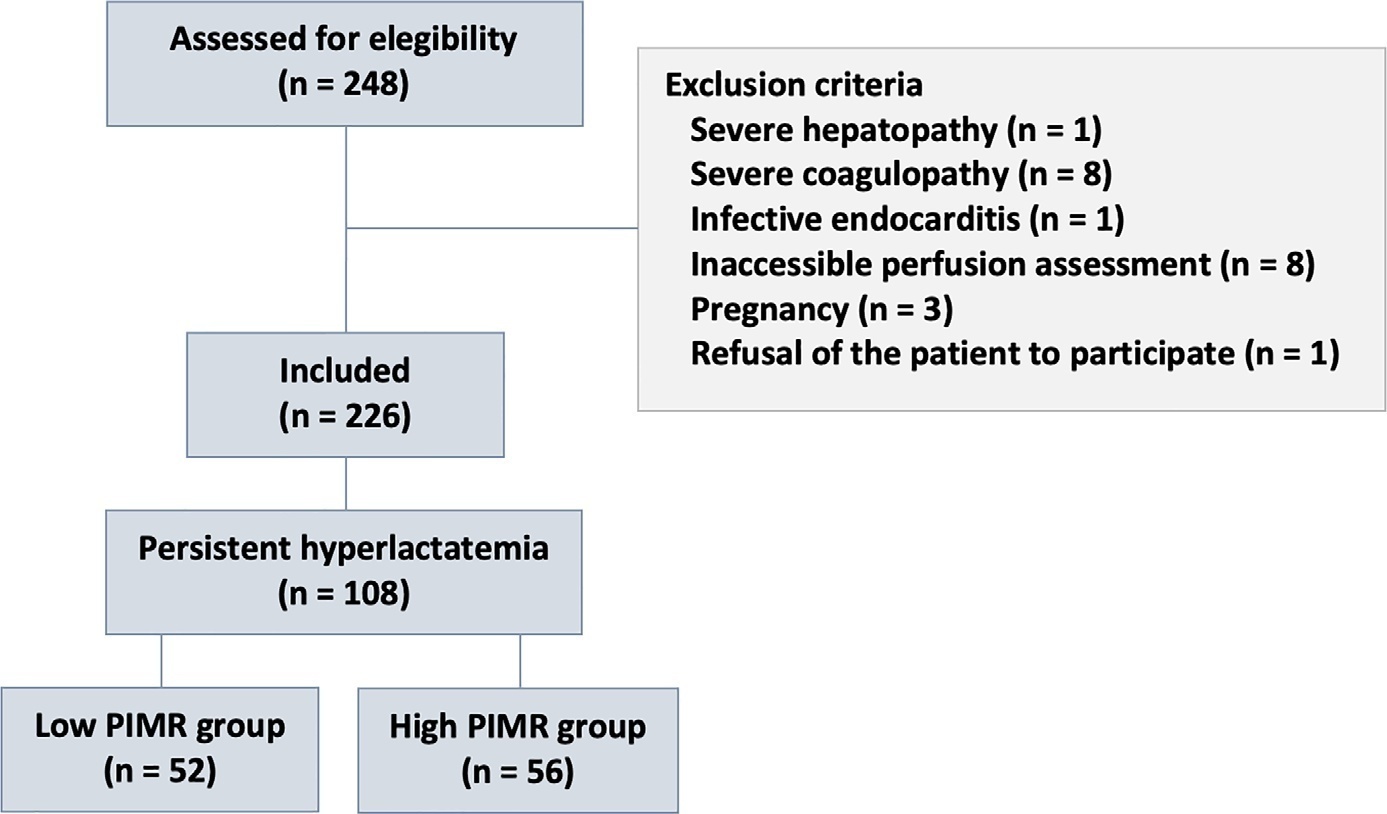
This post hoc analysis of the peripheral perfusion index/postocclusive reactive hyperemia trial, an observational cohort study that enrolled patients with sepsis who persisted with lactate levels ≥ 2mmol/L after fluid resuscitation (with or without shock). Peripheral ischemic microvascular reserve was evaluated using the association of the peripheral perfusion index and postocclusive reactive hyperemia techniques. The cutoff point of ∆ peripheral perfusion index peak values (%) defined the groups with low (≤ 62%) and high peripheral ischemic microvascular reserve (> 62%).
A total of 108 consecutive patients with persistent sepsis-induced hyperlactatemia were studied. The high peripheral ischemic microvascular reserve group showed higher 28-day mortality than the low peripheral ischemic microvascular reserve group (p < 0.01). The temporal dynamics of lactate within the first 48 hours showed a rapid decrease in lactate levels in the low peripheral ischemic microvascular reserve group (p < 0.01). However, this result was not reproduced in the linear mixed effects model. A weak correlation between peripheral ischemic microvascular reserve (%) and lactate level (mmol/L) was observed within the first 24 hours (r = 0.23; p < 0.05).
The prognostic value of high peripheral ischemic microvascular reserve was confirmed in the context of persistent sepsis-induced hyperlactatemia. Although there was a weak positive correlation between peripheral ischemic microvascular reserve value and lactate level within the first 24 hours of sepsis diagnosis, the low peripheral ischemic microvascular reserve group appeared to have a faster decrease in lactate over the 48 hours of follow-up.
Abstract
Rev Bras Ter Intensiva. 2022;34(3):367-373
DOI 10.5935/0103-507X.20220102-en
To evaluate the mechanisms attributed to the prognostic value of peripheral ischemic microvascular reserve in patients with sepsis.
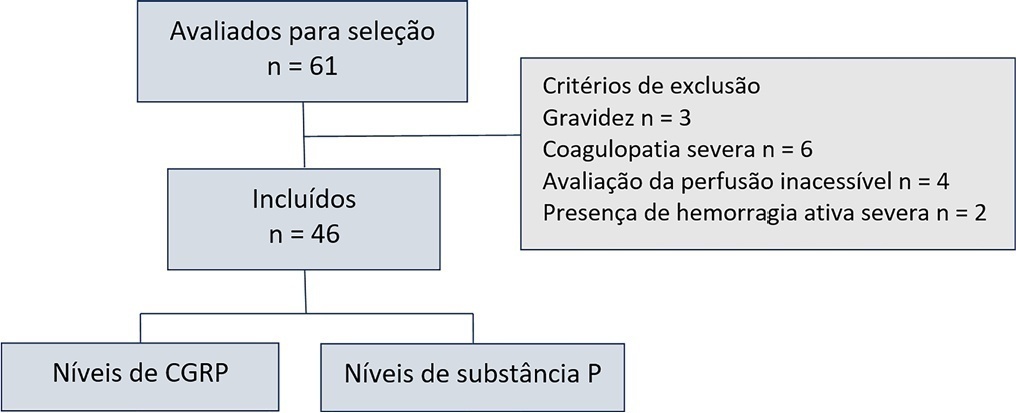
This observational cohort study enrolled 46 consecutive septic patients in the intensive care unit between November 2020 and October 2021. After fluid resuscitation, the peripheral ischemic microvascular reserve was evaluated using the association of postocclusion reactive hyperemia with the peripheral perfusion index. Additionally, peripheral venous blood samples were used to evaluate the neuropeptide calcitonin gene-related peptide and substance P levels in the upper limb before and immediately after postocclusion reactive hyperemia
There was no statistically significant correlation (p > 0.05) between basal values (pg/mL) or variations from neuropeptide levels (%) and the peripheral ischemic microvascular reserve (%).
Although calcitonin gene-related peptide and substance P may have a prognostic role in sepsis, these neuropeptides do not appear to contribute to peripheral ischemic microvascular reserve.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):36-43
DOI 10.5935/0103-507X.20150007
To evaluate the immediate effects of red blood cell transfusion on central venous oxygen saturation and lactate levels in septic shock patients with different transfusion triggers.
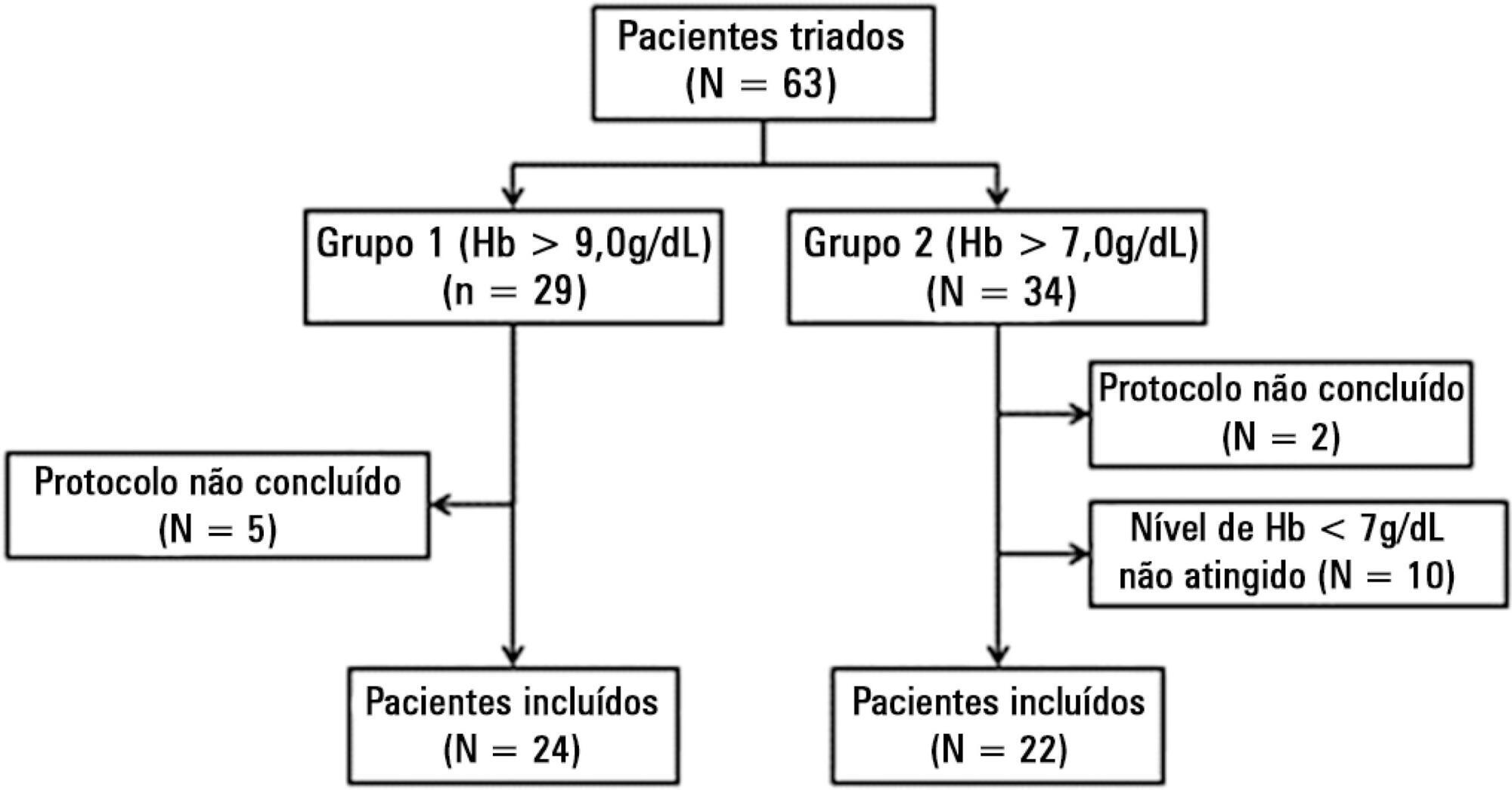
We included patients with a diagnosis of septic shock within the last 48 hours and hemoglobin levels below 9.0g/dL Patients were randomized for immediate transfusion with hemoglobin concentrations maintained above 9.0g/dL (Group Hb9) or to withhold transfusion unless hemoglobin felt bellow 7.0g/dL (Group Hb7). Hemoglobin, lactate, central venous oxygen saturation levels were determined before and one hour after each transfusion.
We included 46 patients and 74 transfusions. Patients in Group Hb7 had a significant reduction in median lactate from 2.44 (2.00 - 3.22) mMol/L to 2.21 (1.80 - 2.79) mMol/L, p = 0.005, which was not observed in Group Hb9 [1.90 (1.80 - 2.65) mMol/L to 2.00 (1.70 - 2.41) mMol/L, p = 0.23]. Central venous oxygen saturation levels increased in Group Hb7 [68.0 (64.0 - 72.0)% to 72.0 (69.0 - 75.0)%, p < 0.0001] but not in Group Hb9 [72.0 (69.0 - 74.0)% to 72.0 (71.0 - 73.0)%, p = 0.98]. Patients with elevated lactate or central venous oxygen saturation < 70% at baseline had a significant increase in these variables, regardless of baseline hemoglobin levels. Patients with normal values did not show a decrease in either group.
Red blood cell transfusion increased central venous oxygen saturation and decreased lactate levels in patients with hypoperfusion regardless of their baseline hemoglobin levels. Transfusion did not appear to impair these variables in patients without hypoperfusion.
Abstract
Rev Bras Ter Intensiva. 2014;26(3):277-286
DOI 10.5935/0103-507X.20140039
We investigated the effect of two different saline solutions on the mechanisms of injury after intestinal ischemia: oxidative stress and inflammatory responses.
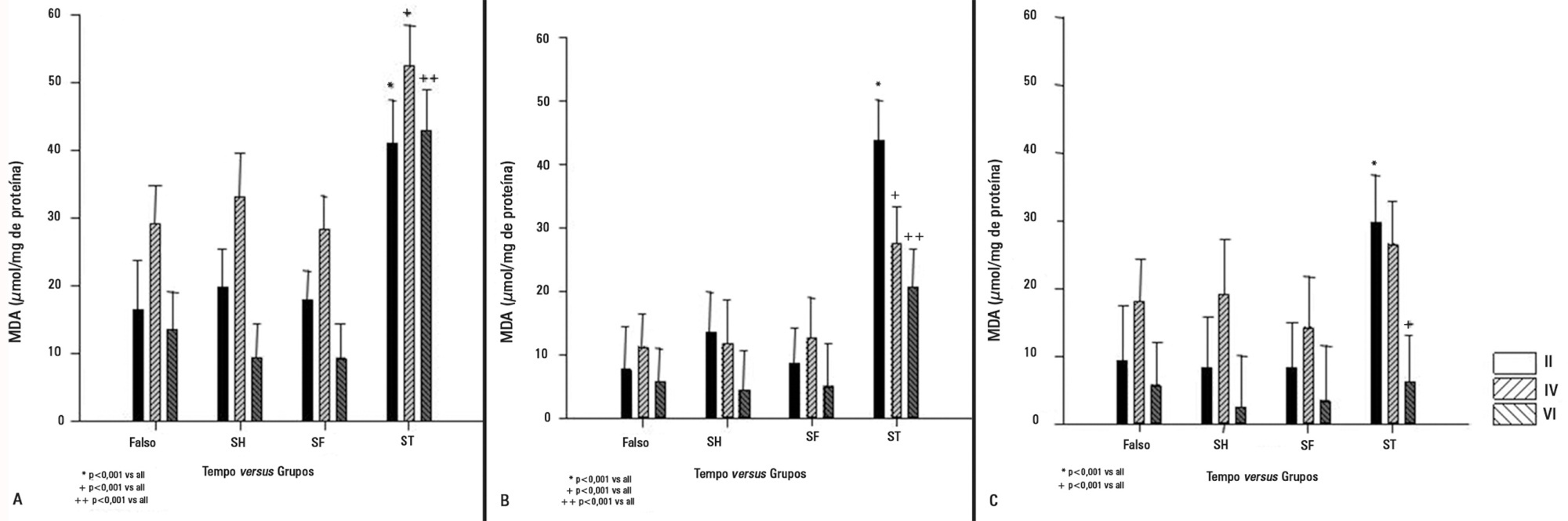
Wistar rats underwent transient superior mesenteric artery occlusion and were studied for 6 hours after reperfusion. After randomization, the animals were divided into four groups: Sham; Hypertonic Saline, in which they received infusion of 4mL/kg body weight of 7.5% hypertonic saline; Saline, in which they received infusion of 33mL/kg body weight of 0.9% saline; and Non Treatment. The infusion was performed immediately prior to the reperfusion. The plasma concentrations of interleukin 6 and interleukin 10 were measured. Tissue samples (lung, liver, and intestine) were collected for malondialdehyde, myeloperoxidase, and interleukin measurements.
The animals that received infusions (Hypertonic Saline and Saline) showed lower levels of tissue malondialdehyde, myeloperoxidase, interleukin 6, and interleukin 10 compared with the Non Treatment group. The plasma concentrations of interleukin 6 and interleukin 10 were higher in the animals treated with 7.5% hypertonic saline compared with Saline and Non Treatment groups.
In this model of transient intestinal ischemia, the adequate maintenance of intravascular volume decreased oxidative stress and the synthesis of inflammatory markers. Both 7.5% Hypertonic Saline and Saline attenuated the deleterious effects observed after intestinal ischemia.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)