Abstract
Rev Bras Ter Intensiva. 2014;26(3):277-286
DOI 10.5935/0103-507X.20140039
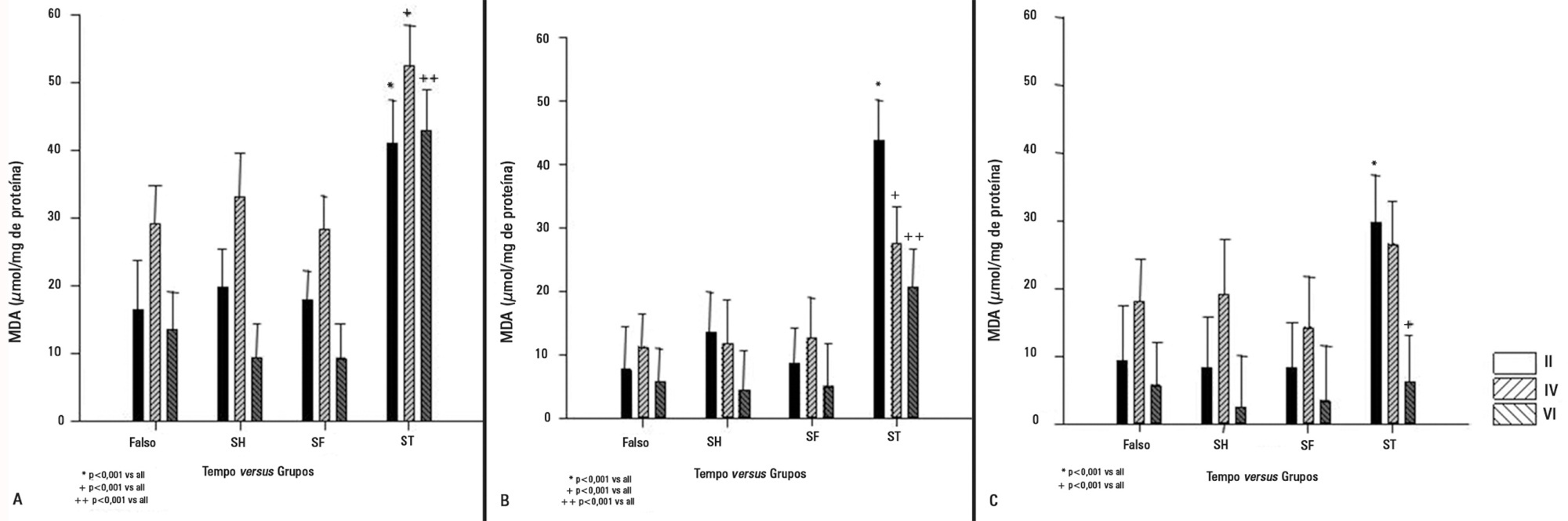
We investigated the effect of two different saline solutions on the mechanisms of injury after intestinal ischemia: oxidative stress and inflammatory responses.
Wistar rats underwent transient superior mesenteric artery occlusion and were studied for 6 hours after reperfusion. After randomization, the animals were divided into four groups: Sham; Hypertonic Saline, in which they received infusion of 4mL/kg body weight of 7.5% hypertonic saline; Saline, in which they received infusion of 33mL/kg body weight of 0.9% saline; and Non Treatment. The infusion was performed immediately prior to the reperfusion. The plasma concentrations of interleukin 6 and interleukin 10 were measured. Tissue samples (lung, liver, and intestine) were collected for malondialdehyde, myeloperoxidase, and interleukin measurements.
The animals that received infusions (Hypertonic Saline and Saline) showed lower levels of tissue malondialdehyde, myeloperoxidase, interleukin 6, and interleukin 10 compared with the Non Treatment group. The plasma concentrations of interleukin 6 and interleukin 10 were higher in the animals treated with 7.5% hypertonic saline compared with Saline and Non Treatment groups.
In this model of transient intestinal ischemia, the adequate maintenance of intravascular volume decreased oxidative stress and the synthesis of inflammatory markers. Both 7.5% Hypertonic Saline and Saline attenuated the deleterious effects observed after intestinal ischemia.
Abstract
Rev Bras Ter Intensiva. 2010;22(4):321-326
DOI 10.1590/S0103-507X2010000400002
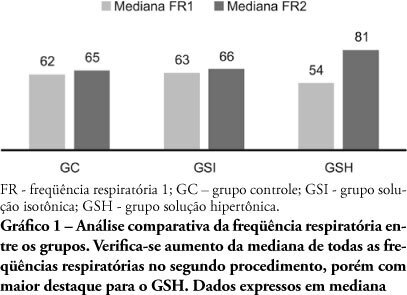
PURPOSE: Sepsis severity and mortality risk require aggressive therapy which includes hemodynamic support. The best fluid for volume replacement, however, is controversial. This study aimed to compare 0.9% isotonic saline solution versus 7.5% hypertonic saline solution as volume replacement fluid in sepsis induced by cecum ligation plus puncture rats. METHODS: This experimental trial included 30 rats divided into three groups: Control group (CG, n = 10), isotonic (ISG, n = 10) and hypertonic solution (HSG, n = 10). Fifteen hours after cecum ligation and puncture, all animals underwent respiratory rate, mean arterial pressure, renal and hepatic blood flow and weight evaluation, plus blood collection for TNF-α measurement. The ISG and HSG treatment groups received volume replacement 60 minutes before the procedure with either 0.9% or 7.5% saline solution, respectively. RESULTS: Two animals died. Significant differences were found for the animals' mean weight after 15 hours (p=0.018), particularly relevant when ISG and HSG are compared (p=0.003). Renal blood flow was also significantly different for the CG versus HSG (p=0.002) and CG versus ISG (p=0.008), but not significantly different for ISG versus HSG. No mean arterial pressure improvement was found for HSG (0.054). Other variables were not significant. CONCLUSIONS: Although no mean blood pressure, hepatic flow or TNF-α improvements were detected, the rats with sepsis 15 hours after cecum ligation and puncture showed significantly increased renal blood flow which was 0.9% isotonic saline solution or of 7.5% hypertonic solution use independent.
Abstract
Rev Bras Ter Intensiva. 2010;22(3):245-249
DOI 10.1590/S0103-507X2010000300005
OBJECTIVE: Ischemic acute kidney injury (iLRA), with multifatorial cause, presents alarming morbidity and mortality. Statin, HMG-CoA inhibition reductase has shown a renoprotective effect, with antioxidant, antiinflamatory and vascular actions. The heme oxygenase-1 (HO-1) can be involved in these pleitropic effects of statin on the renal function. This study was performed in order to evaluate if the renoprotective effect of the statin is a heme mechanism of protection in rats. METHODS: The ischemic model was reproduced by through clamping the bilateral renal pedicles for 30 minutes followed by reperfusion. Adult Wistar rats, weighting from 250-300g, were divided into the following groups: SHAM (control); Ischemia (30 minutes renal ischemia); Ischemia+Statin (sinvastatin 0.5mg/kg,orally (v.o.) for 3 days); Ischemia+Hemin (Hemin, 1.0mg/100g, intraperitoneal (i.p.), 24 hours before surgery); Ischemia+SnPP (SnPP 2μmol/kg, i.p., 24 hours before surgery ); Ischemia+Statin+Hemin; Ischemia+Statin+SnPP. RF (clearance of creatinine, Jaffé method), urinary peroxides (UP), urinary osmolality (UO) and immunohistochemical for ED-1 were evaluated. RESULTS: Results showed that sinvastatin ameliorated RF, urinary osmolality, reduced the UP excrection and the macrophage infiltration in rats submitted to renal ischemia. The inducer of HO-1 and its association with sinvastatin induced a similar pattern of improvement of renal function. CONCLUSION: the study confirmed the renoprotective effect of the statins on renal function, with antioxidant and antiinflamatory actions, and it suggests that this effect can have an interface with the heme system of renal protection.