Abstract
Rev Bras Ter Intensiva. 2010;22(3):245-249
DOI 10.1590/S0103-507X2010000300005
OBJECTIVE: Ischemic acute kidney injury (iLRA), with multifatorial cause, presents alarming morbidity and mortality. Statin, HMG-CoA inhibition reductase has shown a renoprotective effect, with antioxidant, antiinflamatory and vascular actions. The heme oxygenase-1 (HO-1) can be involved in these pleitropic effects of statin on the renal function. This study was performed in order to evaluate if the renoprotective effect of the statin is a heme mechanism of protection in rats. METHODS: The ischemic model was reproduced by through clamping the bilateral renal pedicles for 30 minutes followed by reperfusion. Adult Wistar rats, weighting from 250-300g, were divided into the following groups: SHAM (control); Ischemia (30 minutes renal ischemia); Ischemia+Statin (sinvastatin 0.5mg/kg,orally (v.o.) for 3 days); Ischemia+Hemin (Hemin, 1.0mg/100g, intraperitoneal (i.p.), 24 hours before surgery); Ischemia+SnPP (SnPP 2μmol/kg, i.p., 24 hours before surgery ); Ischemia+Statin+Hemin; Ischemia+Statin+SnPP. RF (clearance of creatinine, Jaffé method), urinary peroxides (UP), urinary osmolality (UO) and immunohistochemical for ED-1 were evaluated. RESULTS: Results showed that sinvastatin ameliorated RF, urinary osmolality, reduced the UP excrection and the macrophage infiltration in rats submitted to renal ischemia. The inducer of HO-1 and its association with sinvastatin induced a similar pattern of improvement of renal function. CONCLUSION: the study confirmed the renoprotective effect of the statins on renal function, with antioxidant and antiinflamatory actions, and it suggests that this effect can have an interface with the heme system of renal protection.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):166-174
DOI 10.1590/S0103-507X2010000200011
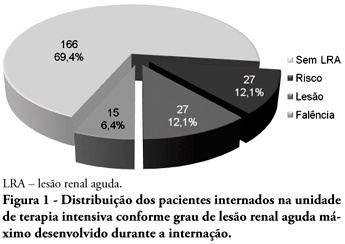
OBJECTIVES: Acute kidney injury is characterized by sudden and generally revertible renal function impairment involving inability to maintain homeostasis. In pediatrics, the main causes of acute kidney injury are sepsis, use of nephrotoxic drugs and renal ischemia in critically ill patients. The incidence of acute kidney injury in these patients ranges from 20 to 30%, resulting in increased morbid-mortality, a 40 to 90% rate. This study aimed to evaluate the incidence of acute kidney injury in intensive care unit patients, to categorize the severity of the acute kidney injury according to the Pediatric Risk, Injury, Failure, Loss, End-Stage (pRIFLE), examine the relationship between the acute kidney injury and severity using the Pediatric Index of Mortality (PIM) and to analyze outcome predictors. METHODS: A prospective study of the patients admitted to the intensive care unit of Hospital Infantil Joana de Gusmão - Florianópolis / SC - Brazil was conducted between July 2008 and January 2009. Were evaluated daily the urine output and serum creatinine, and the patients were categorized according to the pRIFLE criteria. RESULTS: During the follow-up period, 235 children were admitted. The incidence of acute kidney injury was 30.6%, and the maximal pRIFLE score during hospitalization was 12.1% for R, 12.1% for I and 6.4% for F. The mortality rate was 12.3%. The patients who developed acute kidney injury had a ten times bigger risk of death versus the not exposed patients. CONCLUSIONS: Acute kidney injury is frequent in critically ill patients. Early diagnosis and prompt and appropriate therapy for each clinical aspect may change this condition's course and severity, and reduce the patients' morbidity and mortality.
Abstract
Rev Bras Ter Intensiva. 2009;21(1):25-31
DOI 10.1590/S0103-507X2009000100004
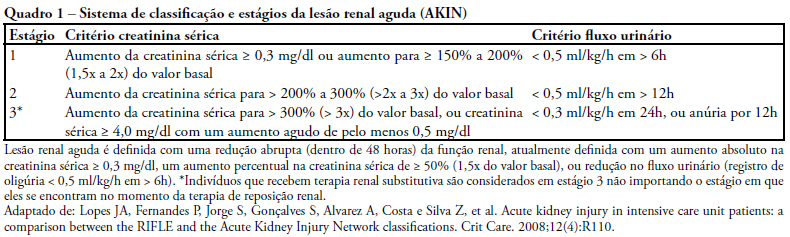
OBJECTIVES: To identify the frequency of the Acute Kidney Injury and to compare the application of the AKIN classification with the separate use of the serum creatinine in the postoperative period of cardiac surgery. METHODS: This study was prospectively developed in a teaching and specialized research hospital in cardiology of the public health system of the state of São Paulo. Forty-four patients submitted to the elective cardiac surgery since the immediate post-surgical period up to the 2nd post-surgical period were followed. RESULTS: It was possible to verify that from the forty-four patients, 75% were hypertensive, 27% were diabetic and mostly were male (64%), with an average age of 55+16 years old. It was observed that advanced age and the elevated body mass index shows a significant correlation to renal dysfunction (p<0, 05). According to the AKIN classification, the urinary flow criterion identified more renal dysfunction than creatinine criterion. It was verified that the renal dysfunction occurred more frequently in the postsurgery period and the majority (82%) from the 63,6% of the patients which were submitted to the revascularization of the myocardium surgery. CONCLUSION: The majority of patients (75%) evolved initially with renal dysfunction signaled it mainly by the urinary flow criterion from the AKIN classification, a higher number compared to the separated creatinine. This fact confirms that the serum creatinine association with the urinary flow has a higher discriminatory performance for the early identification of this syndrome comparatively with the routinely use of the isolated creatinine.
Abstract
Rev Bras Ter Intensiva. 2008;20(4):385-393
DOI 10.1590/S0103-507X2008000400011
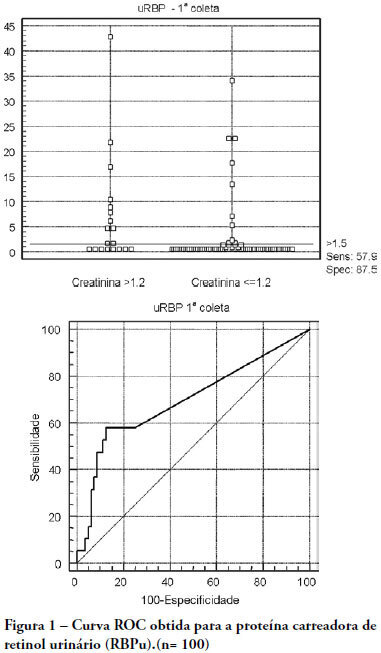
OBJECTIVES: The early assessment of renal dysfunction using common markers does not provide either a sensitive or specific indication of renal dysfunction in critically ill patients. More specific and sensitive markers are desirable for the early detection of an initial renal pathophysiological process. Urinary retinol-binding protein could be an alternative method to early evaluation of renal function in these patients. METHODS: This study followed-up 100 critical care patients and assessed their clinical and laboratory variables, including plasma creatinine and urinary retinol-binding ratio, and demographic variables. RESULTS: The sample was characterized by geriatric (63.4±15.6 years), male (68%), being 53% surgical patients. Statistical analysis showed association between plasma creatinine and the following variables: gender (p-0.026), age (p-0.038), use of vasoactive drugs (p-0.003), proteinuria (p-0.025), Acute Physiological Chronic Health Evaluation (APACHE) II score (p-0.000), urea (p-0.000), potassium (p-0.003) and estimated creatinine clearance (p-0.000). Urinary retinol-binding protein was correlated with more variables: weight, use of invasive ventilation (p-0.000), use of nonsteroidal antiinflammatory drugs (p-0.018), use of vasoactive drugs (p-0.021), high temperature (>37.5ºC) (p-0.005), proteinuria (p-0.000), bilirubinuria (p-0.004), urinary flow (p-0.019), minimal diastolic pressure (p-0.032), minimal systolic pressure (p-0.029), APACHE II (p-0.000), creatinine (p-0.001), urea (p-0.001), estimated creatinine clearance (p-0.000). Urinary retinol-binding protein also tended to associate with previous renal disease, vasculopathy and neoplasm. Sodium excretion fraction correlated with plasma creatinine and urinary retinol-binding protein in univariate analysis. CONCLUSIONS: Urinary retinol-binding protein might be considered in clinical practice as a better marker regarding diagnostic performance in patients at risk of developing acute kidney injury, when compared with other markers routinely used. Moreover, urinary retinol-binding protein has other features of a good diagnostic test - it is a practical and non-invasive method.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)