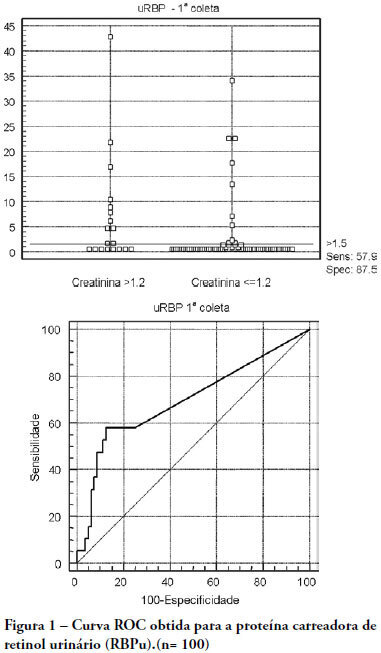
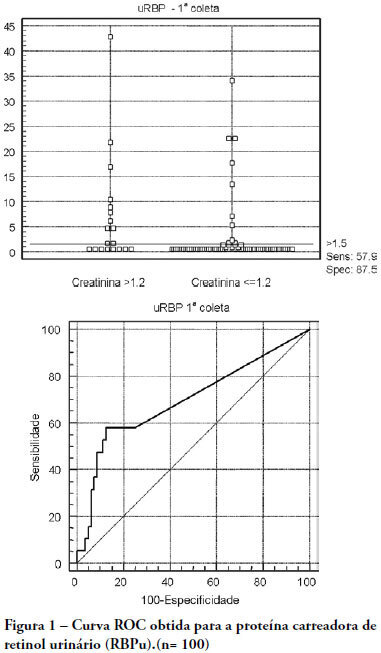
OBJECTIVES: The early assessment of renal dysfunction using common markers does not provide either a sensitive or specific indication of renal dysfunction in critically ill patients. More specific and sensitive markers are desirable for the early detection of an initial renal pathophysiological process. Urinary retinol-binding protein could be an alternative method to early evaluation of renal function in these patients. METHODS: This study followed-up 100 critical care patients and assessed their clinical and laboratory variables, including plasma creatinine and urinary retinol-binding ratio, and demographic variables. RESULTS: The sample was characterized by geriatric (63.4±15.6 years), male (68%), being 53% surgical patients. Statistical analysis showed association between plasma creatinine and the following variables: gender (p-0.026), age (p-0.038), use of vasoactive drugs (p-0.003), proteinuria (p-0.025), Acute Physiological Chronic Health Evaluation (APACHE) II score (p-0.000), urea (p-0.000), potassium (p-0.003) and estimated creatinine clearance (p-0.000). Urinary retinol-binding protein was correlated with more variables: weight, use of invasive ventilation (p-0.000), use of nonsteroidal antiinflammatory drugs (p-0.018), use of vasoactive drugs (p-0.021), high temperature (>37.5ºC) (p-0.005), proteinuria (p-0.000), bilirubinuria (p-0.004), urinary flow (p-0.019), minimal diastolic pressure (p-0.032), minimal systolic pressure (p-0.029), APACHE II (p-0.000), creatinine (p-0.001), urea (p-0.001), estimated creatinine clearance (p-0.000). Urinary retinol-binding protein also tended to associate with previous renal disease, vasculopathy and neoplasm. Sodium excretion fraction correlated with plasma creatinine and urinary retinol-binding protein in univariate analysis. CONCLUSIONS: Urinary retinol-binding protein might be considered in clinical practice as a better marker regarding diagnostic performance in patients at risk of developing acute kidney injury, when compared with other markers routinely used. Moreover, urinary retinol-binding protein has other features of a good diagnostic test – it is a practical and non-invasive method.
Search
Search in:

Comments