Abstract
Crit Care Sci. 2023;35(2):177-186
DOI 10.5935/2965-2774.20230348-pt
To measure the prognostic value of peripheral ischemic microvascular reserve in the context of persistent sepsis-induced hyperlactatemia and measure its influence on the temporal dynamics of lactate and the strength of association between these variables.
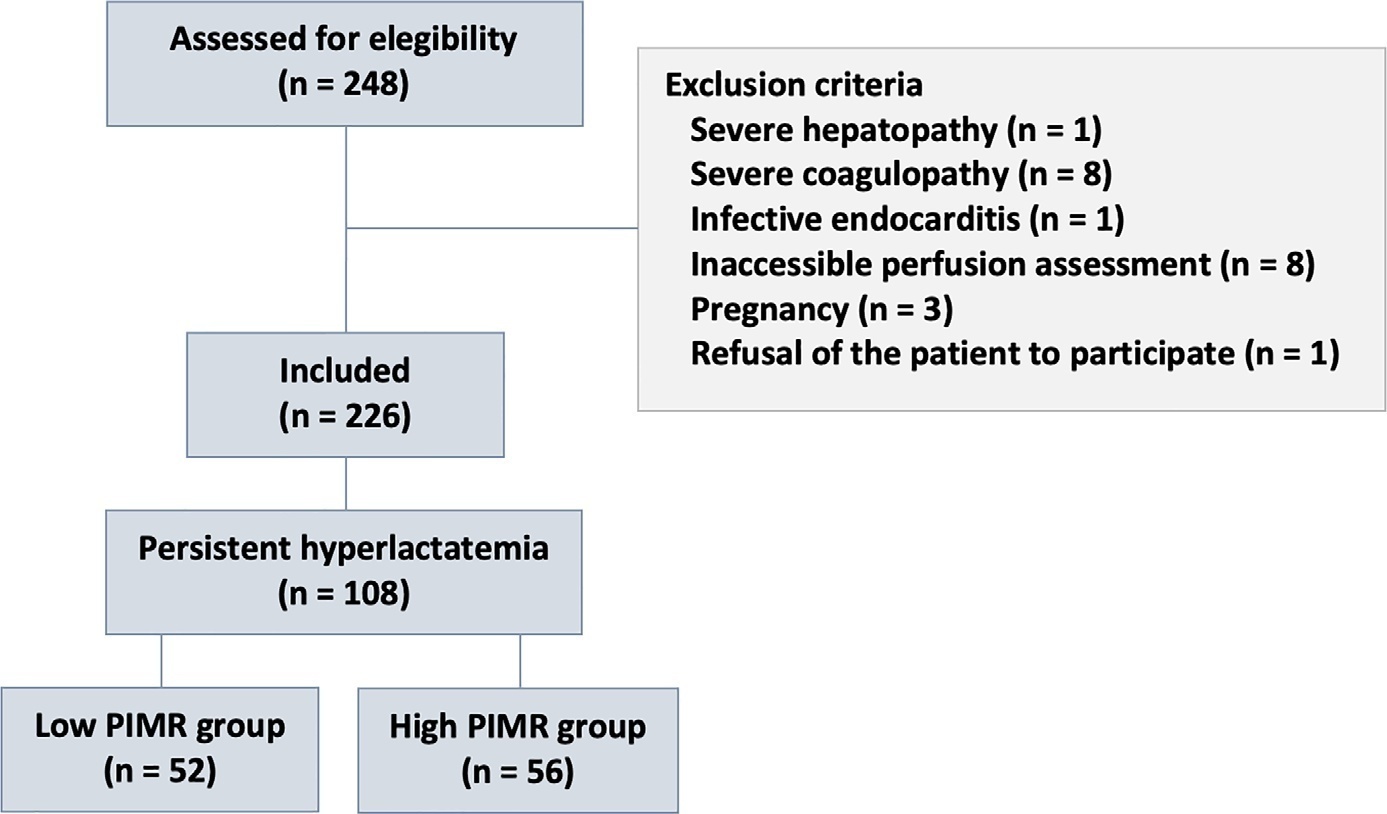
This post hoc analysis of the peripheral perfusion index/postocclusive reactive hyperemia trial, an observational cohort study that enrolled patients with sepsis who persisted with lactate levels ≥ 2mmol/L after fluid resuscitation (with or without shock). Peripheral ischemic microvascular reserve was evaluated using the association of the peripheral perfusion index and postocclusive reactive hyperemia techniques. The cutoff point of ∆ peripheral perfusion index peak values (%) defined the groups with low (≤ 62%) and high peripheral ischemic microvascular reserve (> 62%).
A total of 108 consecutive patients with persistent sepsis-induced hyperlactatemia were studied. The high peripheral ischemic microvascular reserve group showed higher 28-day mortality than the low peripheral ischemic microvascular reserve group (p < 0.01). The temporal dynamics of lactate within the first 48 hours showed a rapid decrease in lactate levels in the low peripheral ischemic microvascular reserve group (p < 0.01). However, this result was not reproduced in the linear mixed effects model. A weak correlation between peripheral ischemic microvascular reserve (%) and lactate level (mmol/L) was observed within the first 24 hours (r = 0.23; p < 0.05).
The prognostic value of high peripheral ischemic microvascular reserve was confirmed in the context of persistent sepsis-induced hyperlactatemia. Although there was a weak positive correlation between peripheral ischemic microvascular reserve value and lactate level within the first 24 hours of sepsis diagnosis, the low peripheral ischemic microvascular reserve group appeared to have a faster decrease in lactate over the 48 hours of follow-up.
Abstract
Rev Bras Ter Intensiva. 2022;34(3):367-373
DOI 10.5935/0103-507X.20220102-en
To evaluate the mechanisms attributed to the prognostic value of peripheral ischemic microvascular reserve in patients with sepsis.
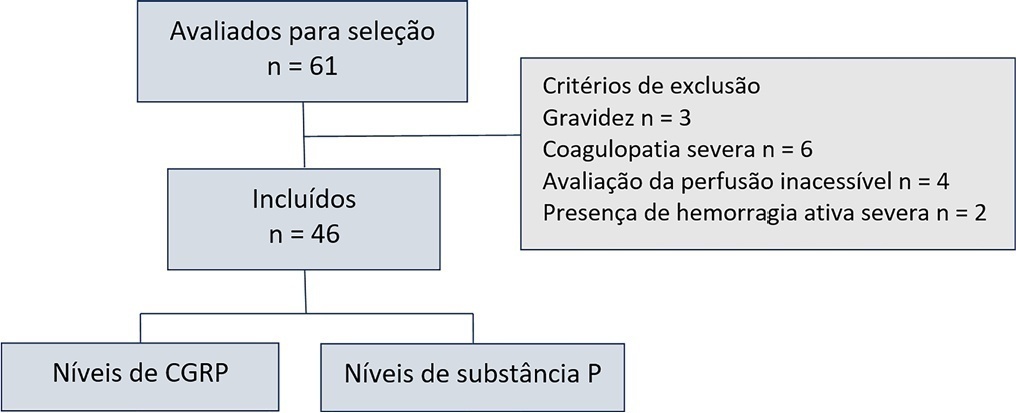
This observational cohort study enrolled 46 consecutive septic patients in the intensive care unit between November 2020 and October 2021. After fluid resuscitation, the peripheral ischemic microvascular reserve was evaluated using the association of postocclusion reactive hyperemia with the peripheral perfusion index. Additionally, peripheral venous blood samples were used to evaluate the neuropeptide calcitonin gene-related peptide and substance P levels in the upper limb before and immediately after postocclusion reactive hyperemia
There was no statistically significant correlation (p > 0.05) between basal values (pg/mL) or variations from neuropeptide levels (%) and the peripheral ischemic microvascular reserve (%).
Although calcitonin gene-related peptide and substance P may have a prognostic role in sepsis, these neuropeptides do not appear to contribute to peripheral ischemic microvascular reserve.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):363-373
DOI 10.5935/0103-507X.20200064
To investigate whether reactive hyperemia measured by peripheral arterial tonometry correlates with markers of endothelial dysfunction and may be used to identify sepsis in critical illness.
A prospective study was performed using a cohort of critically ill patients. Endothelial dysfunction was assessed on admission by quantifying reactive hyperemia-peripheral arterial tonometry and plasma levels of endothelin-1, soluble E-selectin, endocan and syndecan-1. Septic patients were compared to patients without evidence of infection.
Fifty-eight septic patients were compared to 28 controls. The natural logarithm of reactive hyperemia-peripheral arterial tonometry was negatively correlated with cardiovascular comorbidities, disease severity and plasma levels of soluble E-selectin (p = 0.024) and syndecan-1 (p < 0.001). The natural logarithm of reactive hyperemia-peripheral arterial tonometry was lower in septic patients than in controls (0.53 ± 0.48 versus 0.69 ± 0.42, respectively). When adjusted for age, the multivariable model predicted that each 0.1-unit decrease in natural logarithm of reactive hyperemia-peripheral arterial tonometry increased the odds for infection by 14.6%. m.
Reactive hyperemia-peripheral arterial tonometry is closely related to soluble E-selectin and syndecan-1, suggesting an association between endothelial activation, glycocalyx degradation and vascular reactivity. Reactive hyperemia-peripheral arterial tonometry appears to be compromised in critically ill patients, especially those with sepsis.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):135-143
DOI 10.5935/0103-507X.20180027
Microcirculation disturbances are implicated in the prognosis of septic shock. Microvascular hyporesponsiveness can be assessed by an oximetry-derived perfusion index and reactive hyperemia. Using this perfusion index, we investigated reactive hyperemia and its relationship with peripheral perfusion and clinical-hemodynamic parameters in septic shock.
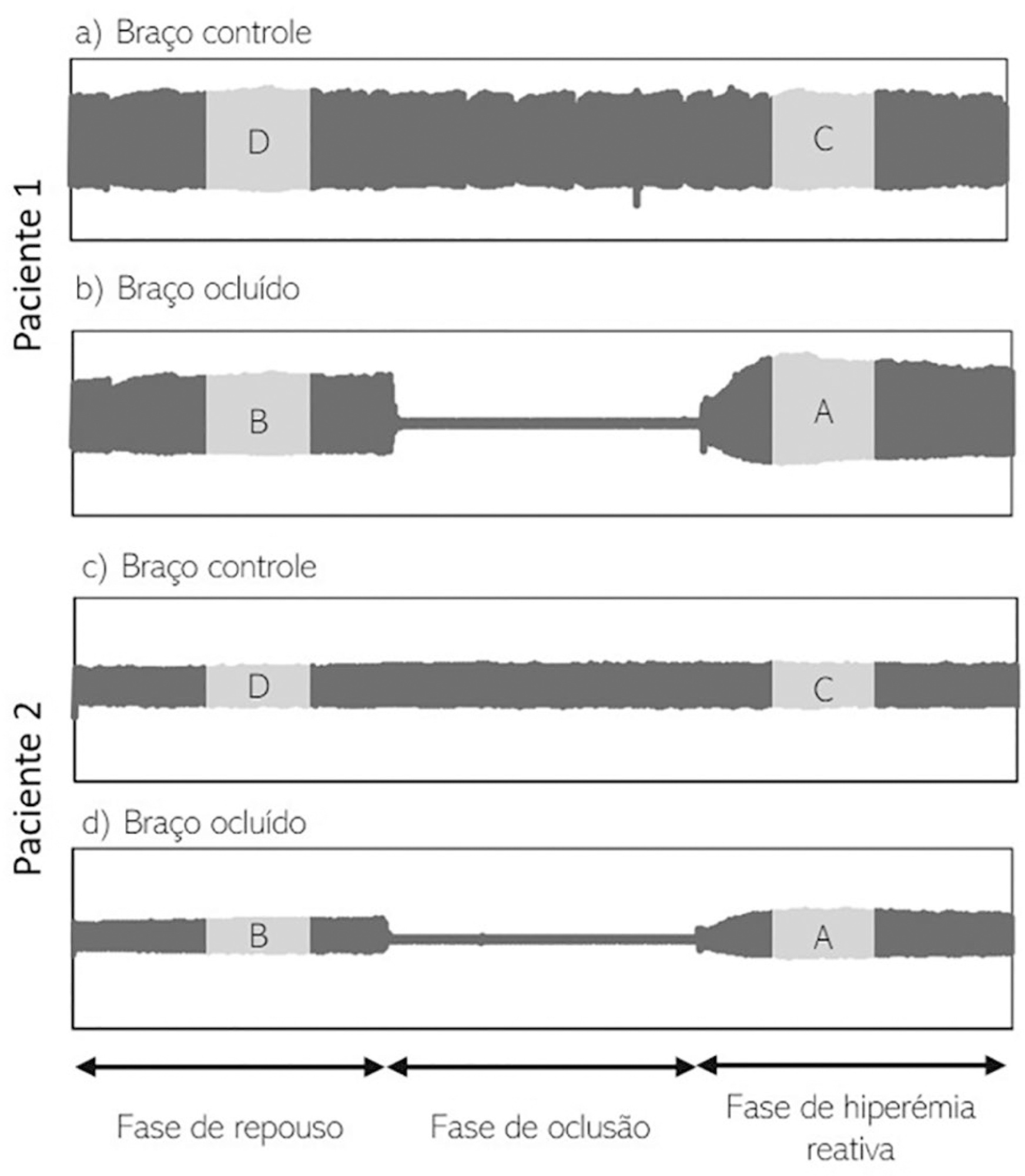
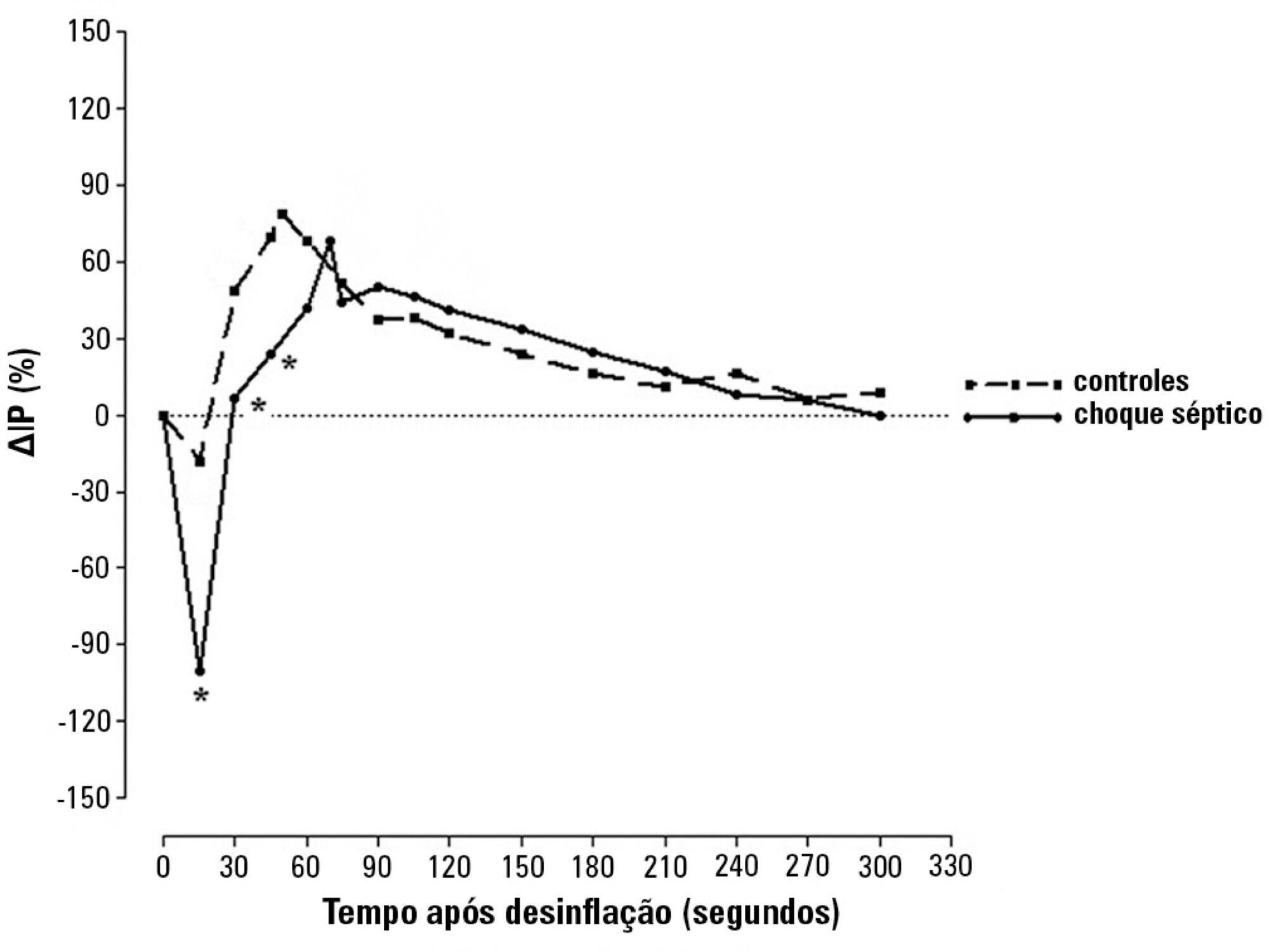
Eighty-two patients were evaluated: 47 with septic shock and 35 controls. Tests were performed within 24 hours after admission. The perfusion index was evaluated before and after a 3-min blood flow occlusion using a time-response analysis for 5 min. The perfusion index was also evaluated in the hyperemic phases and was mainly derived by mechanosensitive (ΔPI0-60) and metabolic mechanisms (ΔPI60-120). Correlation tests were performed between reactive hyperemia and clinical-hemodynamic data.
Reactive hyperemia measured by the perfusion index was significantly lower in patients with septic shock, but this was only observed for the first 45 seconds after cuff-deflation. In the remaining period, there were no statistical differences between the groups. The peaks in the perfusion index were similar between groups, although the peak was reached more slowly in the septic group. Values of ΔPI0-60 were lower in shock [01% (-19% - -40%) versus 39% (6% - 75%); p = 0.001]. However, ΔPI60-120 was similar between the groups [43% (18% - 93%) versus 48% (18% - 98%); p = 0.58]. The time-to-peak of the perfusion index was correlated positively with the SOFA scores and negatively with C-reactive protein; the peak of the perfusion index was positively correlated with vasopressor doses; and the ΔPI60-120 values were positively correlated with C-reactive protein and vasopressor doses. No other significant correlations occurred.
This perfusion index-based study suggests that septic shock promotes initial peripheral vascular hyporesponsiveness and preserves posterior vascular reactivity to a considerable degree. These results demonstrate a time-dependent peripheral hyperemic response and a significant ischemic reserve in septic shock.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)