To evaluate the usefulness and prognostic value of reactive hyperemia – peripheral arterial tonometry in patients with sepsis. Moreover, we investigated the association of reactive hyperemia – peripheral arterial tonometry results with serum levels of certain inflammatory molecules.
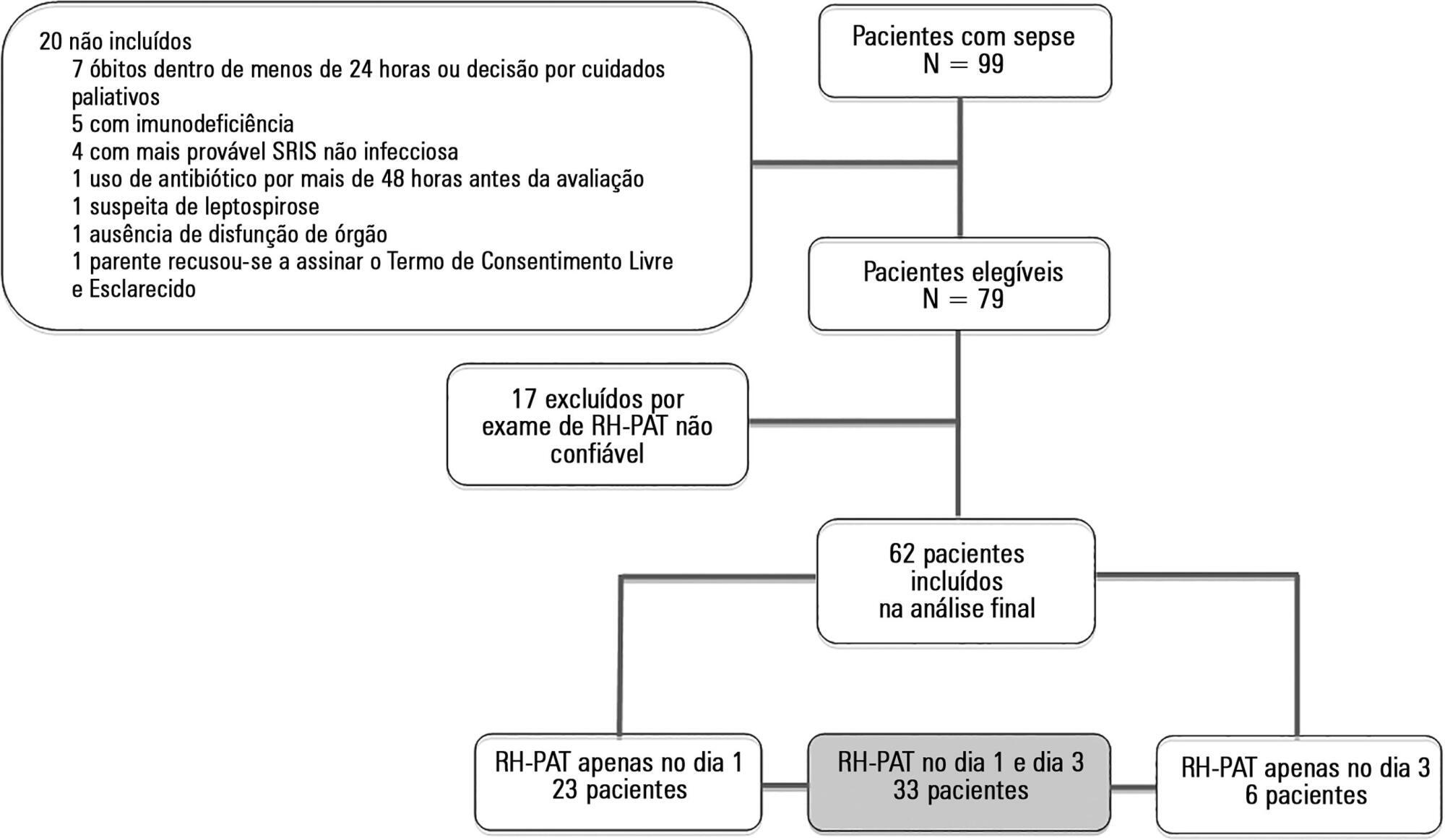
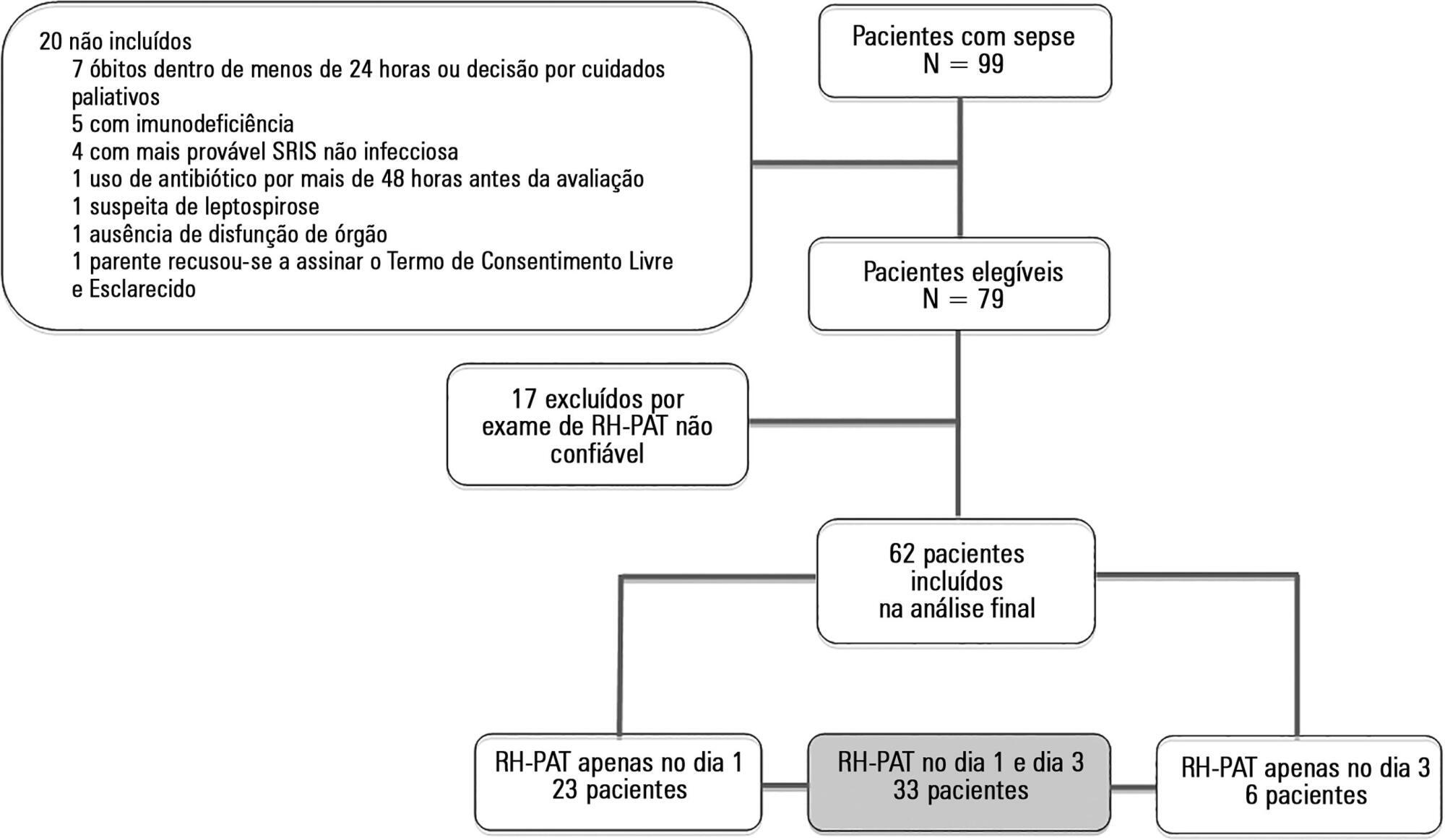
Prospective study, conducted in an 18-bed mixed intensive care unit for adults. The exclusion criteria included severe immunosuppression or antibiotic therapy initiated more than 48 hours before assessment. We measured the reactive hyperemia – peripheral arterial tonometry on inclusion (day 1) and on day 3. Interleukin-6, interleukin-10, high-mobility group box 1 protein and soluble ST2 levels were measured in the blood obtained upon inclusion.
Seventeen of the 79 patients (21.6%) enrolled were determined to have reactive hyperemia – peripheral arterial tonometry signals considered technically unreliable and were excluded from the study. Thus, 62 patients were included in the final analysis, and they underwent a total of 95 reactive hyperemia – peripheral arterial tonometry exams within the first 48 hours after inclusion. The mean age was 51.5 (SD: 18.9), and 49 (62%) of the patients were male. Reactive hyperemia indexes from days 1 and 3 were not associated with vasopressor need, Sequential Organ Failure Assessment score, Acute Physiology and Chronic Health Evaluation II score, or 28-day mortality. Among the patients who died, compared with survivors, there was a significant increase in the day 3 reactive hyperemia index compared with day 1 (p = 0.045). There was a weak negative correlation between the day 1 reactive hyperemia – peripheral arterial tonometry index and the levels of high-mobility group box 1 protein (r = -0.287).
Technical difficulties and the lack of clear associations between the exam results and clinical severity or outcomes strongly limits the utility of reactive hyperemia – peripheral arterial tonometry in septic patients admitted to the intensive care unit.
Search
Search in:

Comments