Abstract
Rev Bras Ter Intensiva. 2019;31(4):434-443
DOI 10.5935/0103-507X.20190084
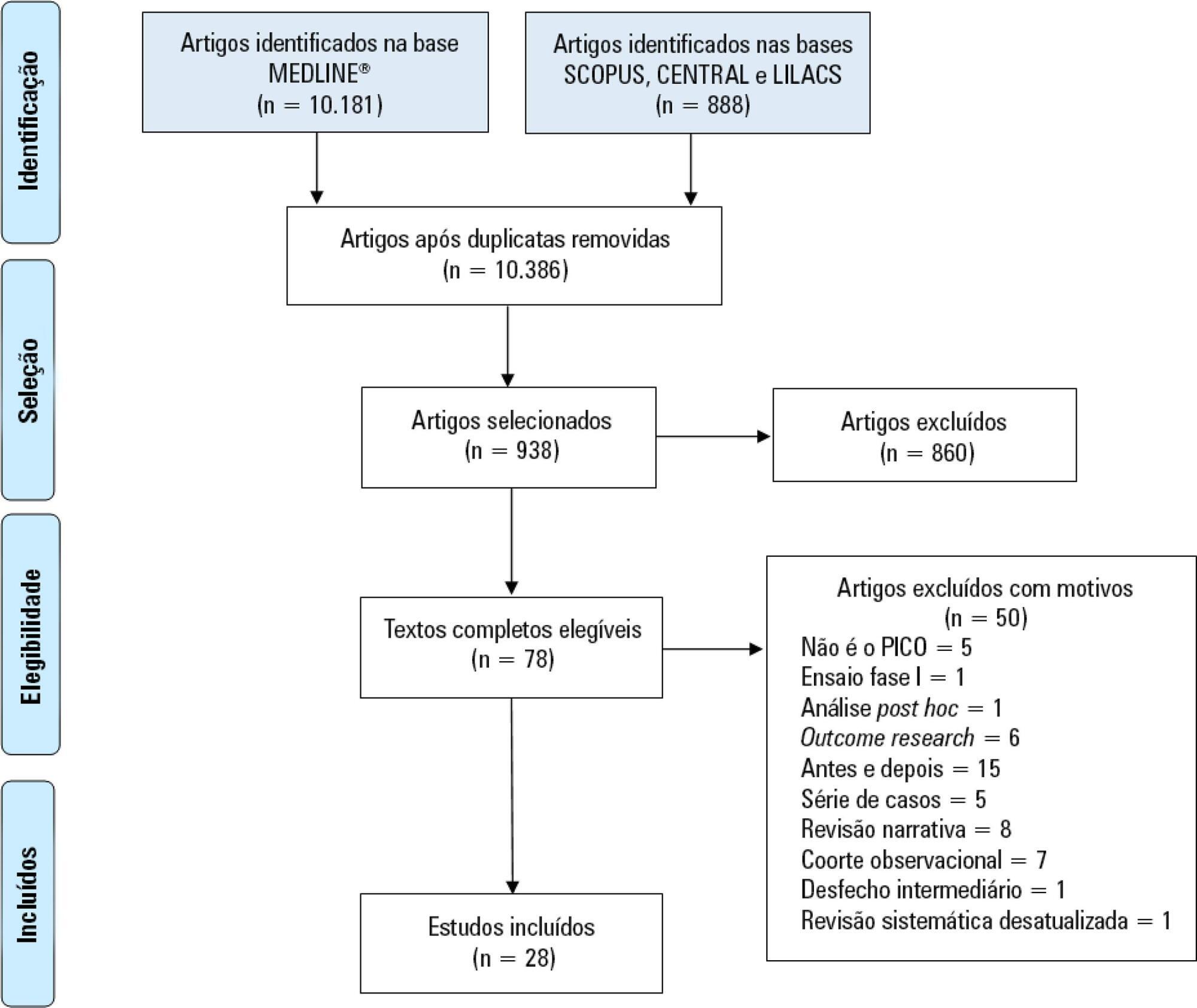
Immobility can cause several complications, including skeletal muscle atrophy and weakness, that influence the recovery of critically ill patients. This effect can be mitigated by early mobilization. Six key questions guided this research: Is early mobilization safe? Which patients are candidates for early mobilization? What are the contraindications? What is the appropriate dose, and how should it be defined? What results are obtained? What are the prognostic indicators for the use of early mobilization? The objective of this guideline was to produce a document that would provide evidence-based recommendations and suggestions regarding the early mobilization of critically ill adult patients, with the aim of improving understanding of the topic and making a positive impact on patient care. This guideline was based on a systematic review of articles conducted using the PICO search strategy, as recommended by the Guidelines Project of the Associação Médica Brasileira. Randomized clinical trials, prognostic cohort studies, and systematic reviews with or without meta-analysis were selected, and the evidence was classified according to the Oxford Center for Evidence-based Medicine Levels of Evidence. For all the questions addressed, enough evidence was found to support safe and well-defined early mobilization, with prognostic indicators that support and recommend the technique. Early mobilization is associated with better functional outcomes and should be performed whenever indicated. Early mobilization is safe and should be the goal of the entire multidisciplinary team.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):529-535
DOI 10.5935/0103-507X.20190066
To measure and compare the functionality of patients after discharge from the intensive care unit and at the time of hospital discharge.
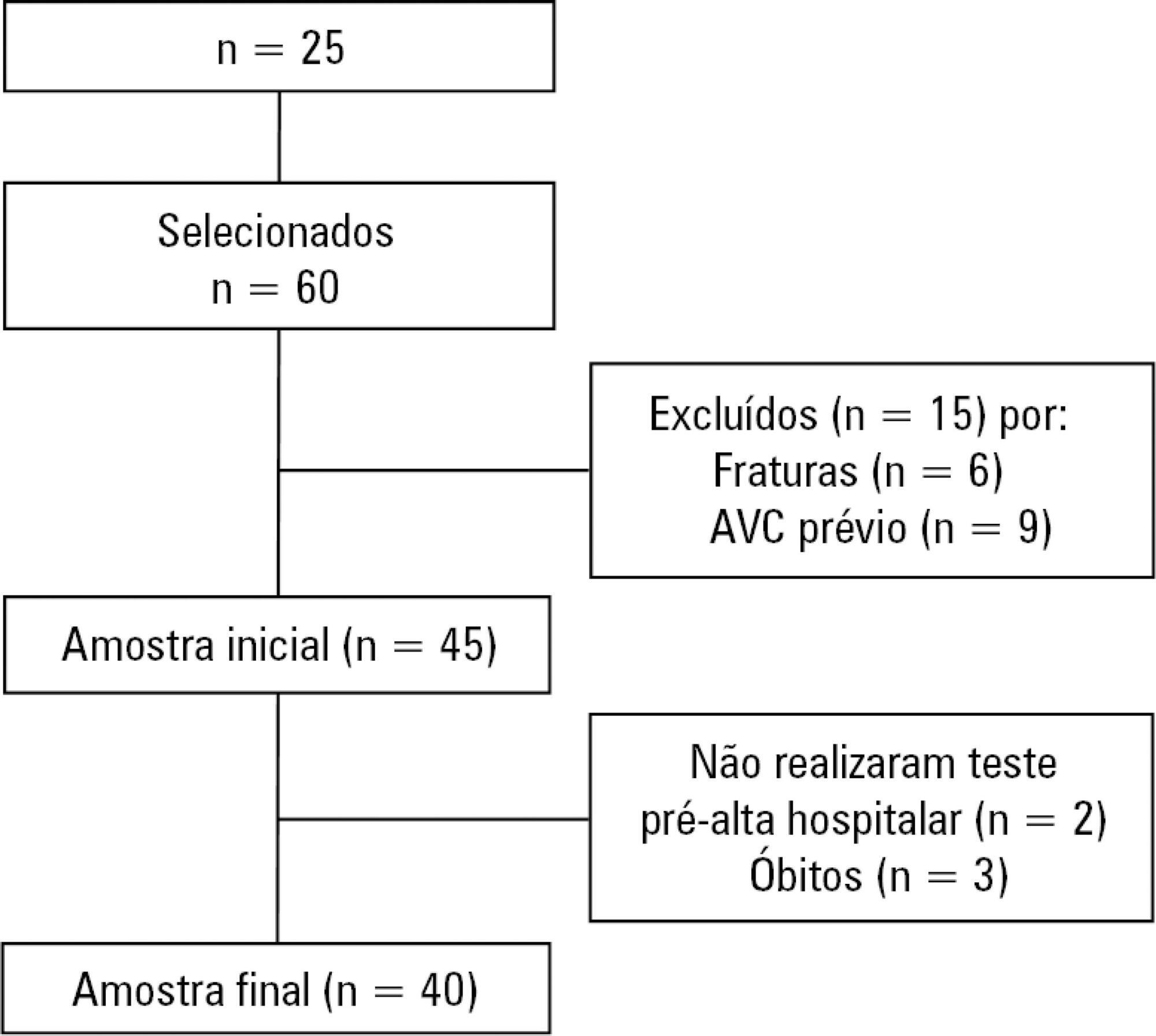
Quantitative study of a prospective cohort performed between August of 2016 and December of 2017 at a university hospital. A 10-meter walk test was performed at 2 timepoints: after discharge from the intensive care unit and prior to hospital discharge. The data were analyzed using Student's t-test and Pearson or Spearman correlation. Statistical Package for Social Science (SPSS) version 21.0 was used for the analysis, and p ≤ 0.05 was adopted as the level of significance.
Forty patients, with a mean age of 57.1 ± 12.2 years and with a predominance of males (60%), were evaluated. For the post-intensive care unit test, a mean speed of 0.48m/s was observed, and for the pre-hospital discharge test, there was an increase to 0.71m/s, evidencing functional evolution during the hospital stay (p < 0.001).
There was significant improvement in walking speed at the time of hospital discharge when compared to the walking speed at the time of intensive care unit discharge.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):227-239
DOI 10.5935/0103-507X.20190017
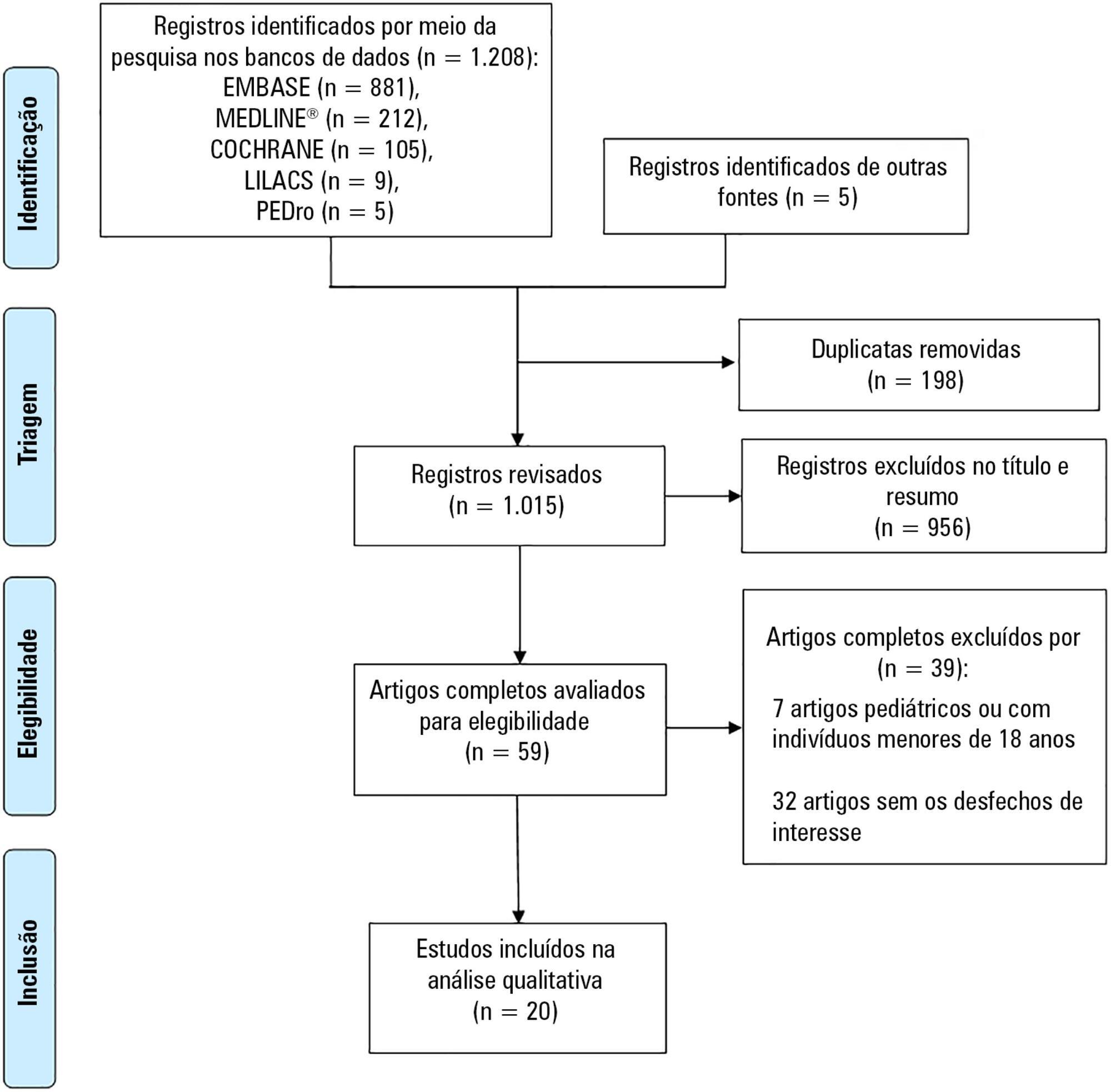
Scientific and technological advances, coupled with the work of multidisciplinary teams in intensive care units, have increased the survival of critically ill patients. An essential life support resource used in intensive care is extracorporeal membrane oxygenation. Despite the increased number of studies involving critically ill patients, few studies to date have demonstrated the safety and benefits of physical therapy combined with extracorporeal membrane oxygenation support. This review identified the clinical outcomes of physical therapy in adult patients on extracorporeal membrane oxygenation support by searching the MEDLINE®, PEDro, Cochrane CENTRAL, LILACS, and EMBASE databases and by manually searching the references of the articles published until September 2017. The database search retrieved 1,213 studies. Of these studies, 20 were included in this review, with data on 317 subjects (58 in the control group). Twelve studies reported that there were no complications during physical therapy. Cannula fracture during ambulation (one case), thrombus in the return cannula (one case), and leg swelling (one case) were reported in two studies, and desaturation and mild vertigo were reported in two studies. In contrast, improvements in respiratory/pulmonary function, functional capacity, muscle strength (with reduced muscle mass loss), incidence of myopathy, length of hospitalization, and mortality in patients who underwent physical therapy were reported. The analysis of the available data indicates that physical therapy, including early progressive mobilization, standing, ambulation, and breathing techniques, together with extracorporeal membrane oxygenation, is feasible, relatively safe, and potentially beneficial for critically ill adult patients.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):187-194
DOI 10.5935/0103-507X.20180037
To investigate the knowledge of multi-professional staff members about the early mobilization of critically ill adult patients and identify attitudes and perceived barriers to its application.
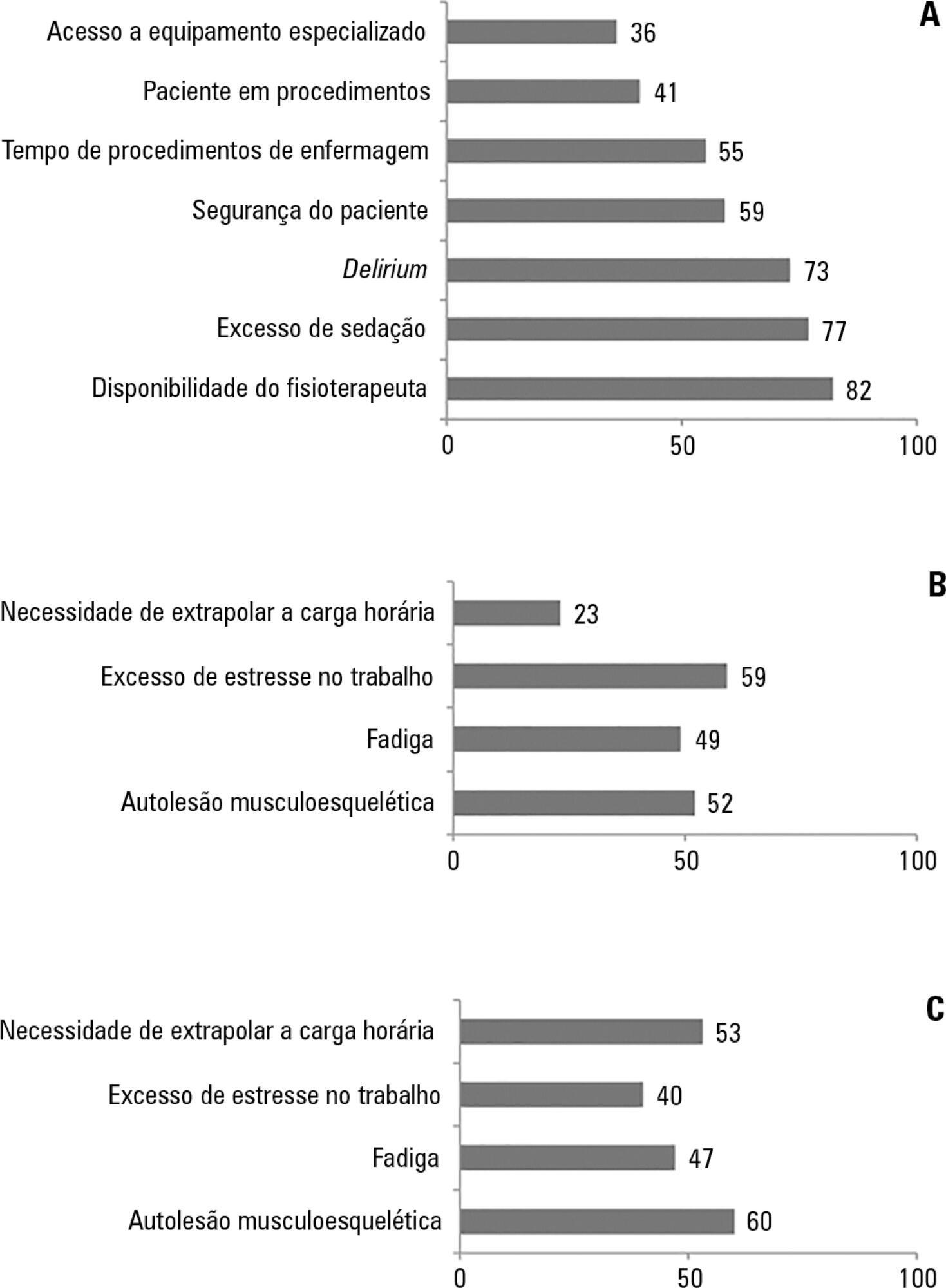
A cross-sectional study was conducted during the second semester of 2016 with physicians, nursing professionals and physical therapists from six intensive care units at two teaching hospitals. Questions were answered on a 5-point Likert scale and analyzed as proportions of professionals who agreed or disagreed with statements. The chi-square and Fisher's exact tests were used to investigate differences in the responses according to educational/training level, previous experience with early mobilization and years of experience in intensive care units.
The questionnaire was answered by 98 out of 514 professionals (response rate: 19%). The acknowledged benefits of early mobilization were maintenance of muscle strength (53%) and shortened length of mechanical ventilation (83%). Favorable attitudes toward early mobilization included recognition that its benefits for patients under mechanical ventilation exceed the risks for both patients and staff, that early mobilization should be routinely performed via nursing and physical therapy protocols, and readiness to change the parameters of mechanical ventilation and reduce sedation to facilitate the early mobilization of patients. The main barriers mentioned were the unavailability of professionals and time to mobilize patients, excessive sedation, delirium, risk of musculoskeletal self-injury and excessive stress at work.
The participants were aware of the benefits of early mobilization and manifested attitudes favorable to its application. However, the actual performance of early mobilization was perceived as a challenge, mainly due to the lack of professionals and time, excessive sedation, delirium, risk of musculoskeletal self-injury and excessive stress at work.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):509-519
DOI 10.5935/0103-507X.20170076
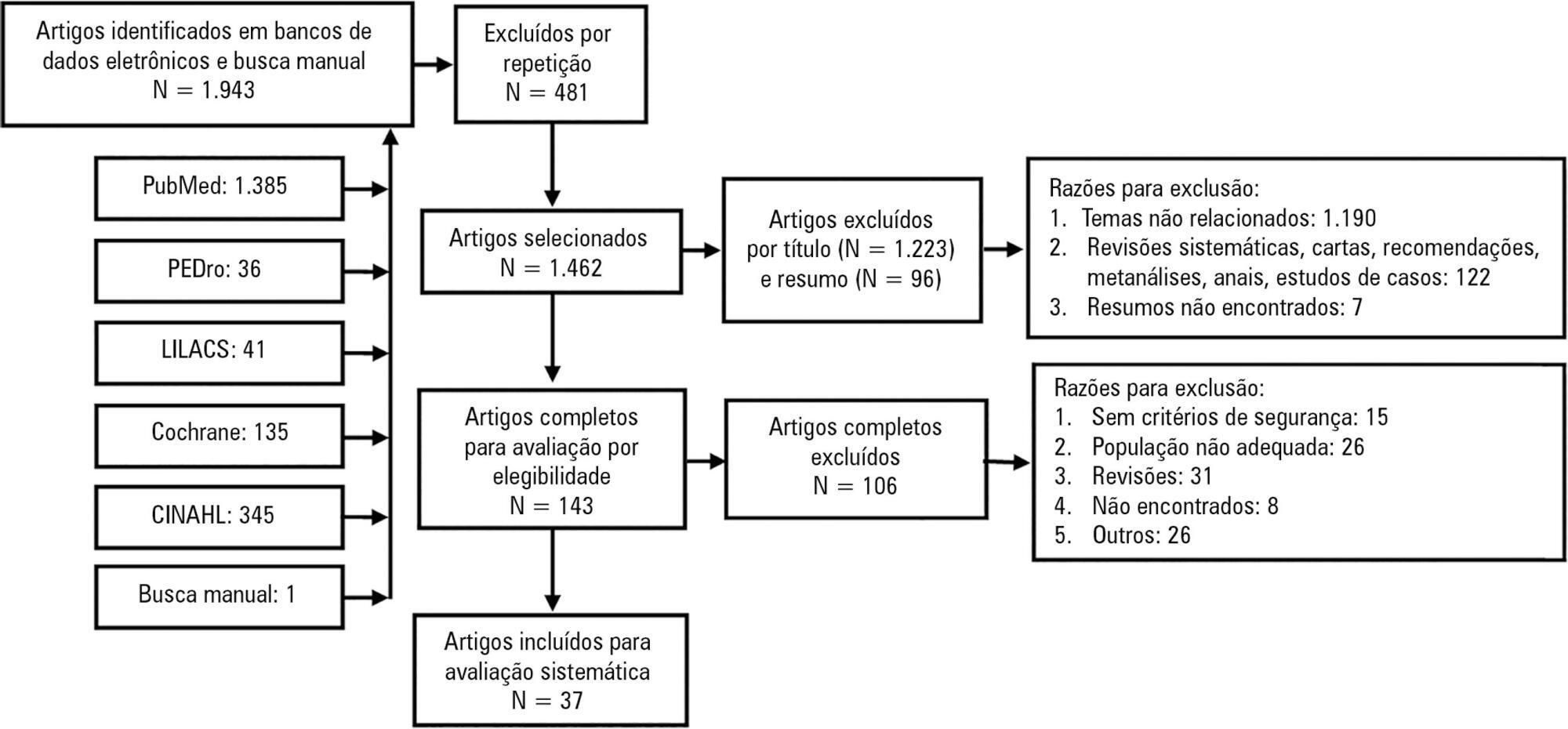
Mobilization of critically ill patients admitted to intensive care units should be performed based on safety criteria. The aim of the present review was to establish which safety criteria are most often used to start early mobilization for patients under mechanical ventilation admitted to intensive care units. Articles were searched in the PubMed, PEDro, LILACS, Cochrane and CINAHL databases; randomized and quasi-randomized clinical trials, cohort studies, comparative studies with or without simultaneous controls, case series with 10 or more consecutive cases and descriptive studies were included. The same was performed regarding prospective, retrospective or cross-sectional studies where safety criteria to start early mobilization should be described in the Methods section. Two reviewers independently selected potentially eligible studies according to the established inclusion criteria, extracted data and assessed the studies' methodological quality. Narrative description was employed in data analysis to summarize the characteristics and results of the included studies; safety criteria were categorized as follows: cardiovascular, respiratory, neurological, orthopedic and other. A total of 37 articles were considered eligible. Cardiovascular safety criteria exhibited the largest number of variables. However, respiratory safety criteria exhibited higher concordance among studies. There was greater divergence among the authors regarding neurological criteria. There is a need to reinforce the recognition of the safety criteria used to start early mobilization for critically ill patients; the parameters and variables found might contribute to inclusion into service routines so as to start, make progress and guide clinical practice.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):161-169
DOI 10.5935/0103-507X.20150028
Evaluation of the functional outcomes of patients undergoing an early rehabilitation protocol for critically ill patients from admission to discharge from the intensive care unit.
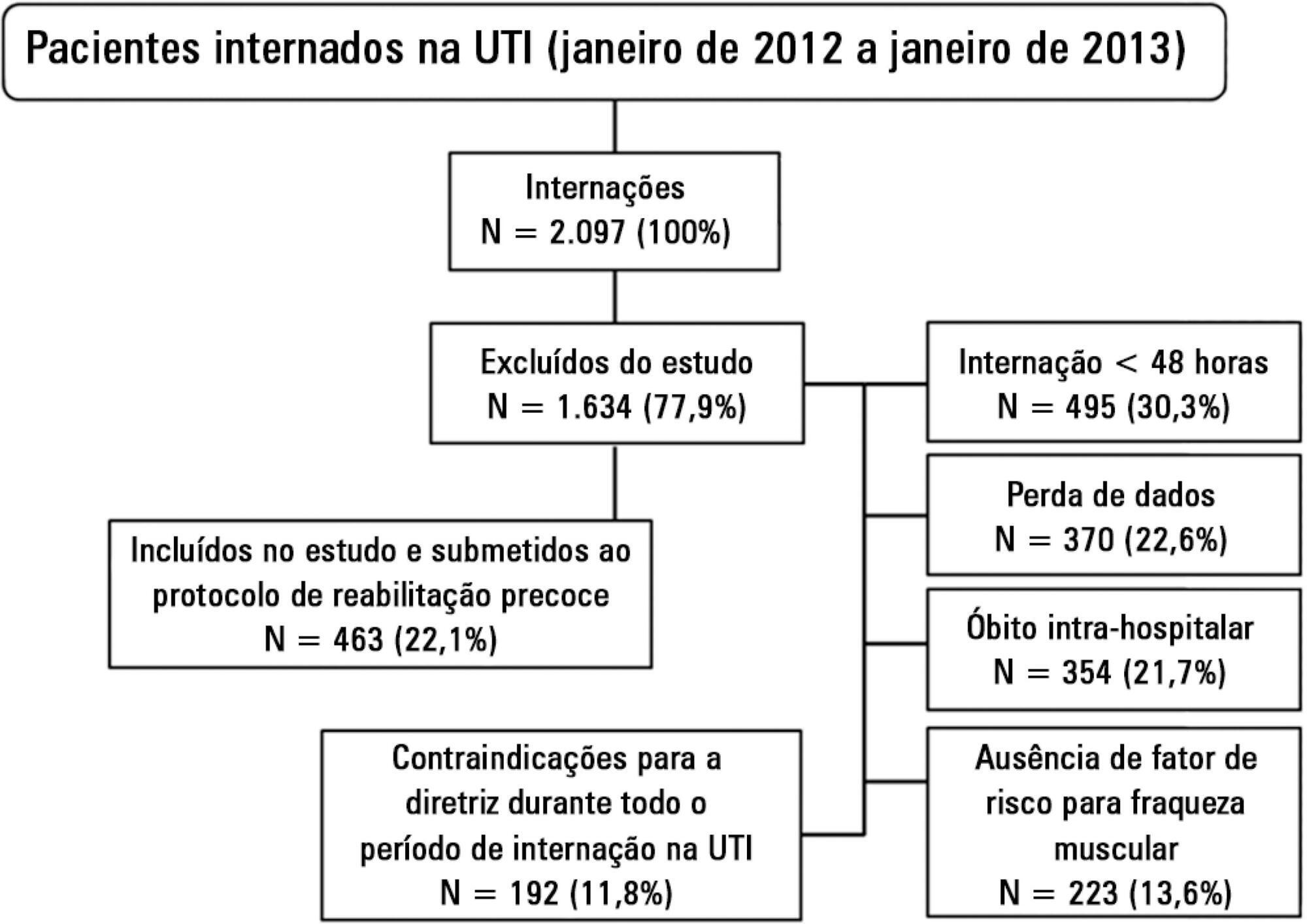
A retrospective cross-sectional study was conducted that included 463 adult patients with clinical and/or surgical diagnosis undergoing an early rehabilitation protocol. The overall muscle strength was evaluated at admission to the intensive care unit using the Medical Research Council scale. Patients were allocated to one of four intervention plans according to the Medical Research Council score, the suitability of the plan’s parameters, and the increasing scale of the plan expressing improved functional status. Uncooperative patients were allocated to intervention plans based on their functional status. The overall muscle strength and/or functional status were reevaluated upon discharge from the intensive care unit by comparison between the Intervention Plans upon admission (Planinitial) and discharge (Planfinal). Patients were classified into three groups according to the improvement of their functional status or not: responsive 1 (Planfinal > Planinitial), responsive 2 (Planfinal = Planinitial) and unresponsive (Planfinal < Planinitial).
In total, 432 (93.3%) of 463 patients undergoing the protocol responded positively to the intervention strategy, showing maintenance and/or improvement of the initial functional status. Clinical patients classified as unresponsive were older (74.3 ± 15.1 years of age; p = 0.03) and had longer lengths of intensive care unit (11.6 ± 14.2 days; p = 0.047) and hospital (34.5 ± 34.1 days; p = 0.002) stays.
The maintenance and/or improvement of the admission functional status were associated with shorter lengths of intensive care unit and hospital stays. The results suggest that the type of diagnosis, clinical or surgical, fails to define the positive response to an early rehabilitation protocol.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):27-32
DOI 10.1590/S0103-507X2010000100006
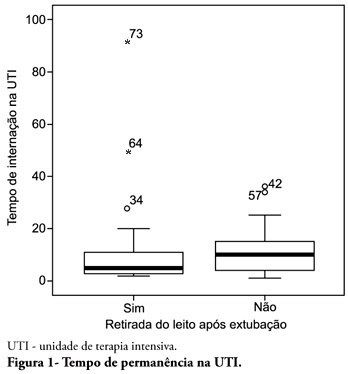
OBJECTIVE: To describe the withdrawal of the bed frequency in mechanic ventilation patients and its impact on mortality and length of stay in the intensive care unit. METHODS: This was a retrospective cohort study in mechanical ventilation patients. Clinical and epidemiological variables, withdrawal of bed related motor therapy, intensive care unit length of stay and mortality were evaluated. RESULTS: We studied 91 patients, mean age of 62.5± 18.8 years, predominantly female (52%) and mean intensive care unit length of stay of 07 days (95% CI, 8-13 days). Considering the withdrawal of the bed or not, no difference was observed between groups regarding length of stay in intensive care unit. Patients who were withdrawn of bed had a lower clinical severity. Their mortality rate was 29.7%. The not withdrawn of bed group had higher both actual and expected mortality. CONCLUSIONS: Patients withdrawn of bed following mechanical ventilation discontinuation showed lower mortality. It is suggested that early intensive care unit mobilization and withdrawal of bed should be stimulated.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)