Abstract
Crit Care Sci. 2023;35(2):168-176
DOI 10.5935/2965-2774.20230410-pt
We hypothesized that the use of mechanical insufflation-exsufflation can reduce the incidence of acute respiratory failure within the 48-hour post-extubation period in intensive care unit-acquired weakness patients.
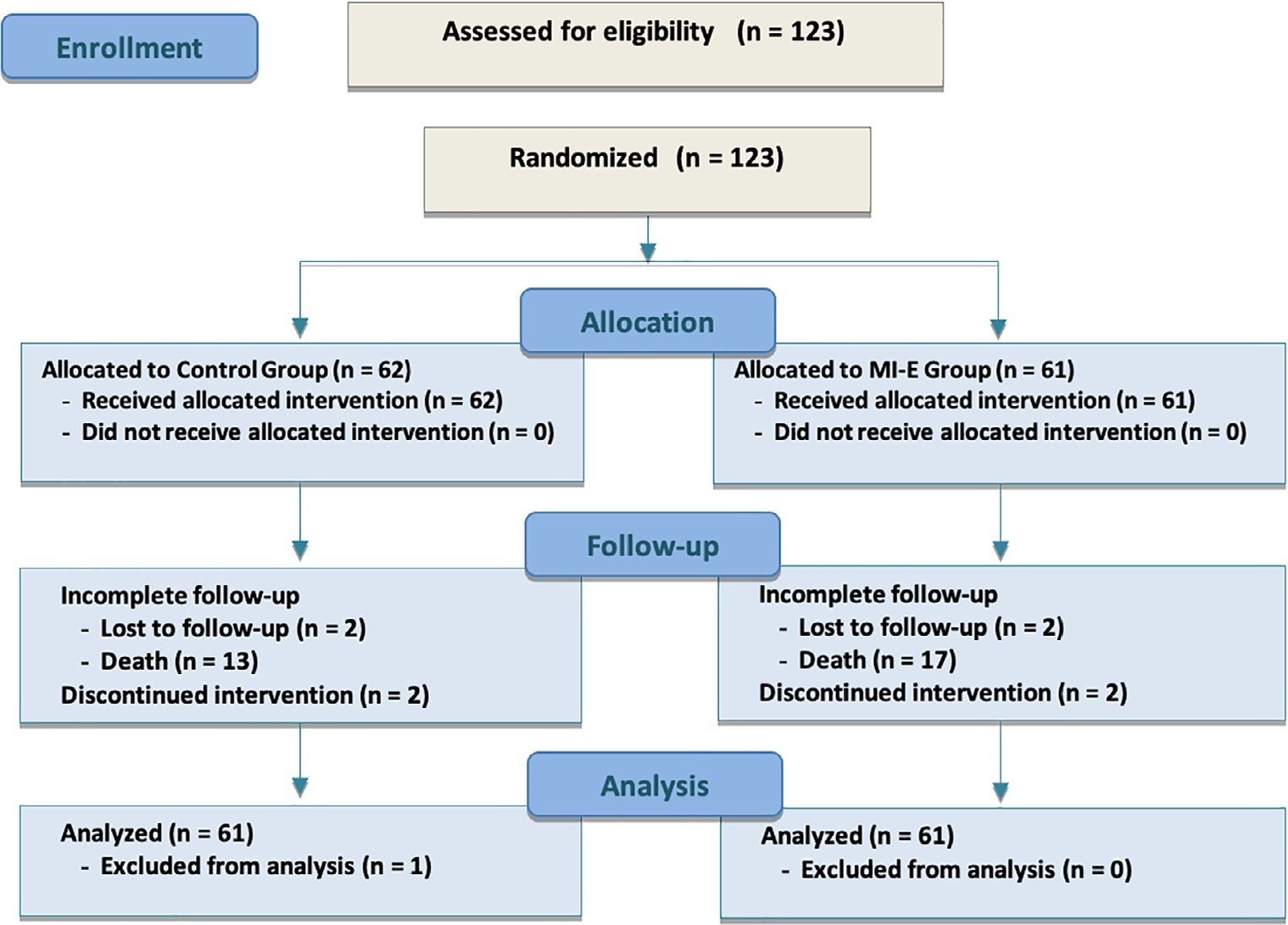
This was a prospective randomized controlled open-label trial. Patients diagnosed with intensive care unit-acquired weakness were consecutively enrolled based on a Medical Research Council score ≤ 48/60. The patients randomly received two daily sessions; in the control group, conventional chest physiotherapy was performed, while in the intervention group, chest physiotherapy was associated with mechanical insufflation-exsufflation. The incidence of acute respiratory failure within 48 hours of extubation was evaluated. Similarly, the reintubation rate, intensive care unit length of stay, mortality at 28 days, and survival probability at 90 days were assessed. The study was stopped after futility results in the interim analysis.
We included 122 consecutive patients (n = 61 per group). There was no significant difference in the incidence of acute respiratory failure between treatments (11.5% control group versus 16.4%, intervention group; p = 0.60), the need for reintubation (3.6% versus 10.7%; p = 0.27), mean length of stay (3 versus 4 days; p = 0.33), mortality at Day 28 (9.8% versus 15.0%; p = 0.42), or survival probability at Day 90 (21.3% versus 28.3%; p = 0.41).
Mechanical insufflation-exsufflation combined with chest physiotherapy seems to have no impact in preventing postextubation acute respiratory failure in intensive care unit-acquired weakness patients. Similarly, mortality and survival probability were similar in both groups. Nevertheless, given the early termination of the trial, further clinical investigation is strongly recommended.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):511-520
DOI 10.5935/0103-507X.20190088
To characterize patients with chronic critical illness and identify predictors of development of chronic critical illness.
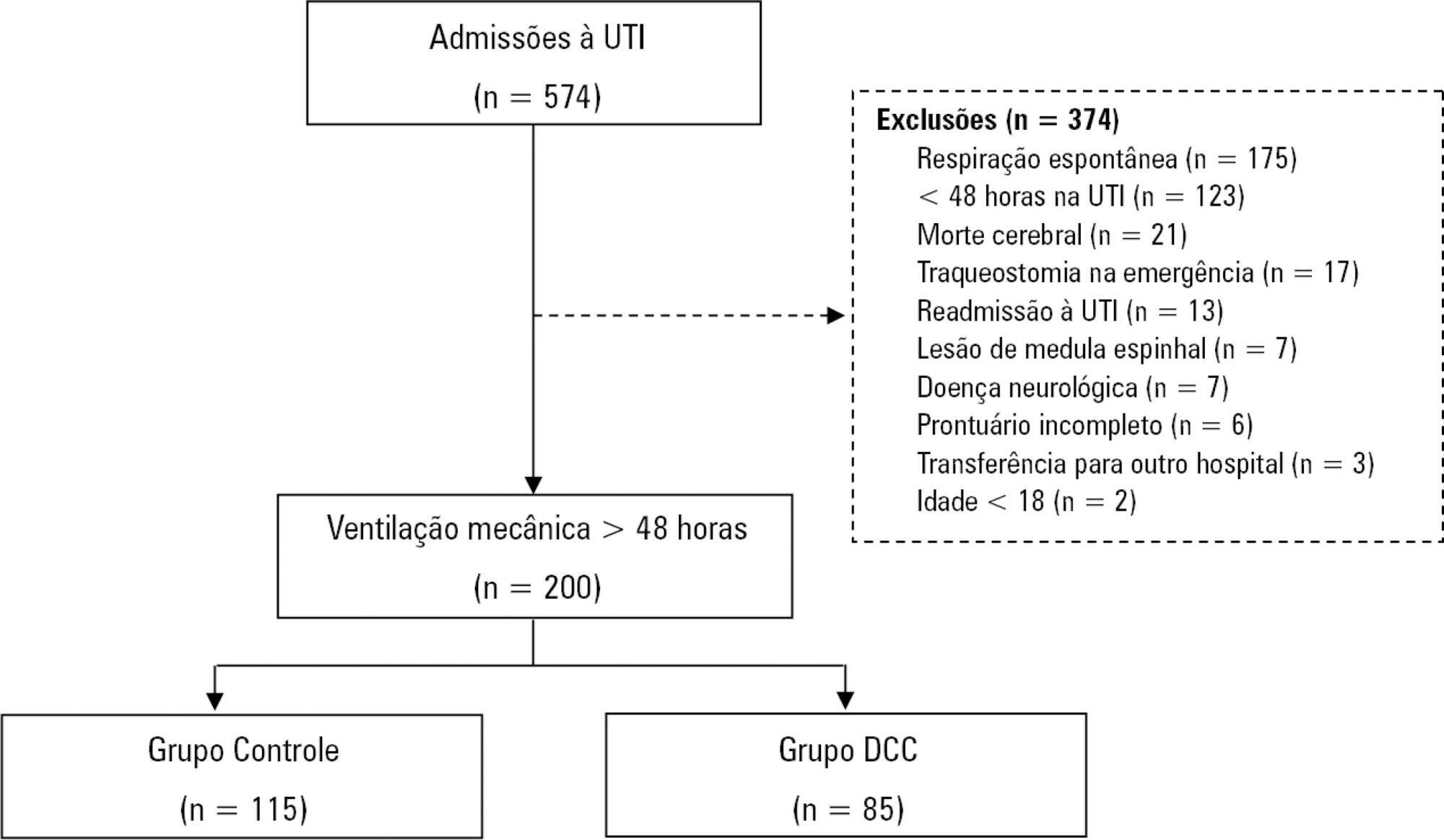
Prospective data was collected for 1 year in the intensive care unit of a general hospital in Southern Brazil. Three logistic regression models were constructed to identify factors associated with chronic critical illness.
Among the 574 subjects admitted to the intensive care unit, 200 were submitted to mechanical ventilation. Of these patients, 85 (43.5%) developed chronic critical illness, composing 14.8% of all the patients admitted to the intensive care unit. The regression model that evaluated the association of chronic critical illness with conditions present prior to intensive care unit admission identified chronic renal failure in patients undergoing hemodialysis (OR 3.57; p = 0.04) and a neurological diagnosis at hospital admission (OR 2.25; p = 0.008) as independent factors. In the model that evaluated the association of chronic critical illness with situations that occurred during intensive care unit stay, muscle weakness (OR 2.86; p = 0.01) and pressure ulcers (OR 9.54; p < 0.001) had the strongest associations. In the global multivariate analysis (that assessed previous factors and situations that occurred in the intensive care unit), hospital admission due to neurological diseases (OR 2.61; p = 0.03) and the development of pressure ulcers (OR 9.08; p < 0.001) had the strongest associations.
The incidence of chronic critical illness in this study was similar to that observed in other studies and had a strong association with the diagnosis of neurological diseases at hospital admission and chronic renal failure in patients undergoing hemodialysis, as well as complications developed during hospitalization, such as pressure ulcers and muscle weakness.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):187-194
DOI 10.5935/0103-507X.20180037
To investigate the knowledge of multi-professional staff members about the early mobilization of critically ill adult patients and identify attitudes and perceived barriers to its application.
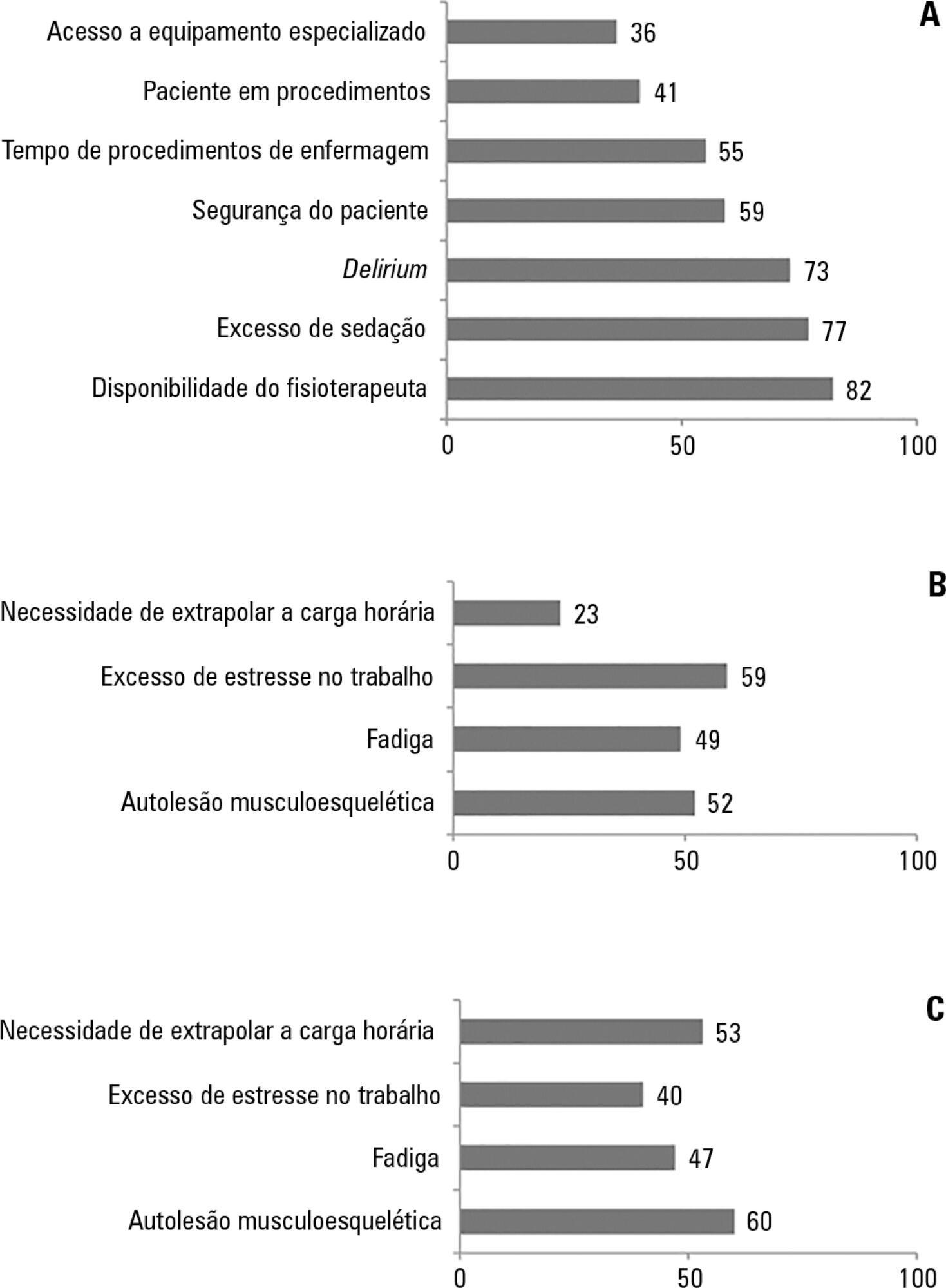
A cross-sectional study was conducted during the second semester of 2016 with physicians, nursing professionals and physical therapists from six intensive care units at two teaching hospitals. Questions were answered on a 5-point Likert scale and analyzed as proportions of professionals who agreed or disagreed with statements. The chi-square and Fisher's exact tests were used to investigate differences in the responses according to educational/training level, previous experience with early mobilization and years of experience in intensive care units.
The questionnaire was answered by 98 out of 514 professionals (response rate: 19%). The acknowledged benefits of early mobilization were maintenance of muscle strength (53%) and shortened length of mechanical ventilation (83%). Favorable attitudes toward early mobilization included recognition that its benefits for patients under mechanical ventilation exceed the risks for both patients and staff, that early mobilization should be routinely performed via nursing and physical therapy protocols, and readiness to change the parameters of mechanical ventilation and reduce sedation to facilitate the early mobilization of patients. The main barriers mentioned were the unavailability of professionals and time to mobilize patients, excessive sedation, delirium, risk of musculoskeletal self-injury and excessive stress at work.
The participants were aware of the benefits of early mobilization and manifested attitudes favorable to its application. However, the actual performance of early mobilization was perceived as a challenge, mainly due to the lack of professionals and time, excessive sedation, delirium, risk of musculoskeletal self-injury and excessive stress at work.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):466-475
DOI 10.5935/0103-507X.20170063
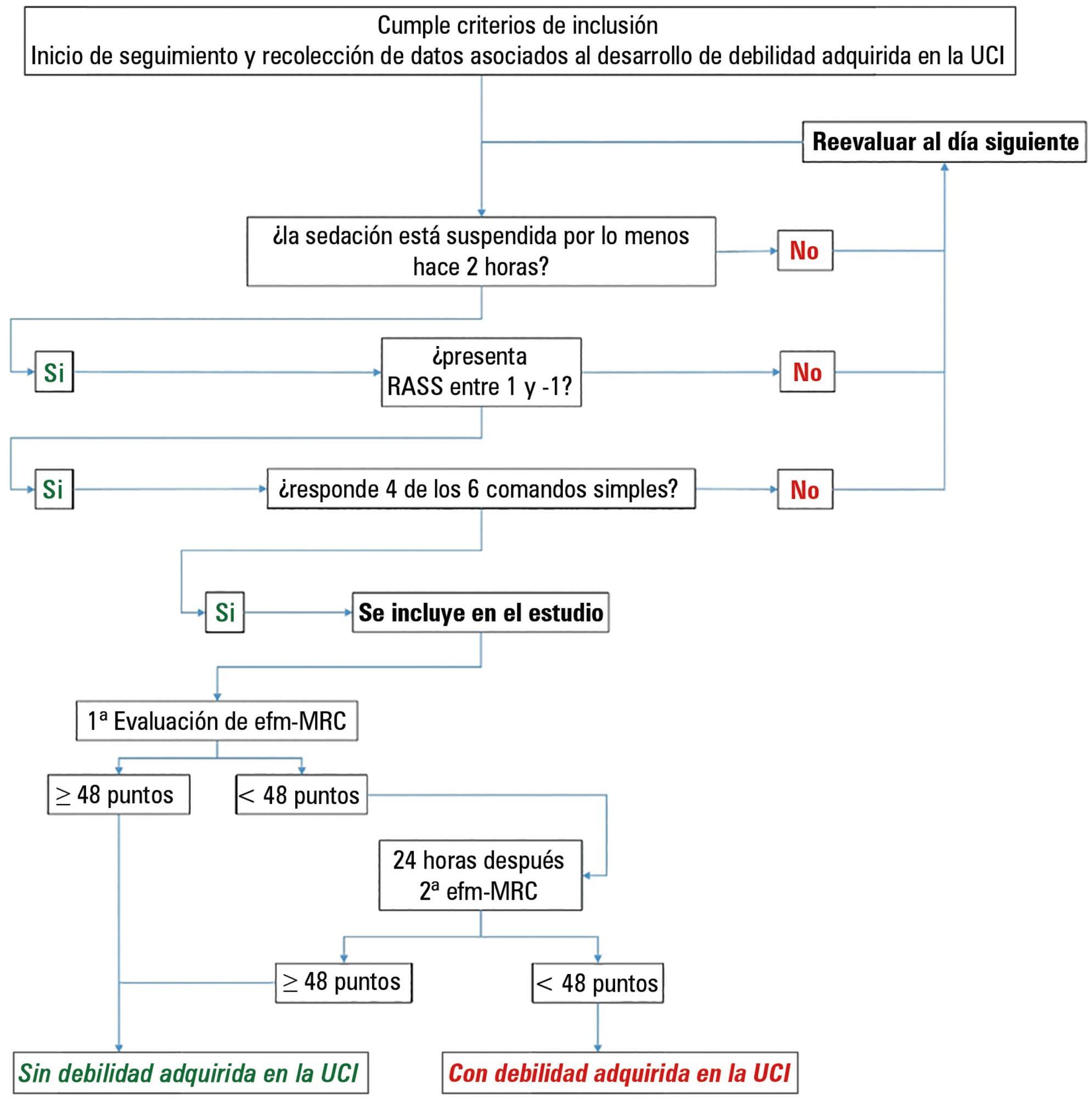
This paper sought to determine the accumulated incidence and analyze the risk factors associated with the development of weakness acquired in the intensive care unit and its relationship to inspiratory weakness.
We conducted a prospective cohort study at a single center, multipurpose medical-surgical intensive care unit. We included adult patients who required mechanical ventilation ≥ 24 hours between July 2014 and January 2016. No interventions were performed. Demographic data, clinical diagnoses, the factors related to the development of intensive care unit -acquired weakness, and maximal inspiratory pressure were recorded.
Of the 111 patients included, 66 developed intensive care unit -acquired weakness, with a cumulative incidence of 40.5% over 18 months. The group with intensive care unit-acquired weakness were older (55.9 ± 17.6 versus 45.8 ± 16.7), required more mechanical ventilation (7 [4 - 10] days versus 4 [2 - 7.3] days), and spent more time in the intensive care unit (15.5 [9.2 - 22.8] days versus 9 [6 - 14] days). More patients presented with delirium (68% versus 39%), hyperglycemia > 3 days (84% versus 59%), and positive balance > 3 days (73.3% versus 37%). All comparisons were significant at p < 0.05. A multiple logistic regression identified age, hyperglycemia ≥ 3 days, delirium, and mechanical ventilation > 5 days as independent predictors of intensive care unit-acquired weakness. Low maximal inspiratory pressure was associated with intensive care unit-acquired weakness (p < 0.001), and the maximum inspiratory pressure cut-off value of < 36cmH2O had sensitivity and specificity values of 31.8% and 95.5%, respectively, when classifying patients with intensive care unit-acquired weakness.
The intensive care unit acquired weakness is a condition with a high incidence in our environment. The development of intensive care unit-acquired weakness was associated with age, delirium, hyperglycemia, and mechanical ventilation > 5 days. The maximum inspiratory pressure value of ≥ 36cmH2O was associated with a high diagnostic value to exclude the presence of intensive care unit -acquired weakness.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):85-91
DOI 10.1590/S0103-507X2010000100014
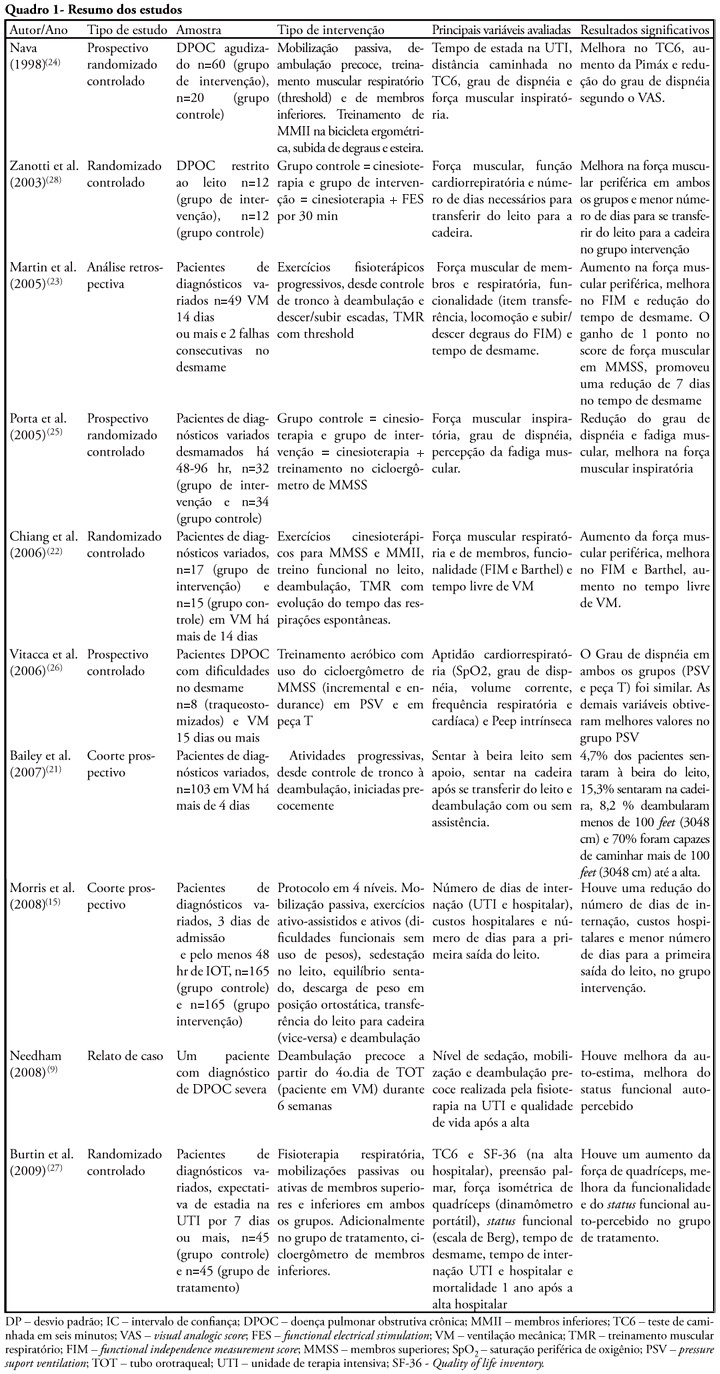
The development of critical patient-related generalized weakness is a common complication in patients admitted to an intensive care unit. The reduced muscle strength increases the time for weaning, hospitalization, the risk of infections and consequent mortality. Physiotherapy is used in these patients as a resource for the prevention of muscle weakness, atrophy and functional capacity recovery. The aim of this study was to review the literature regarding the use of exercise alone in intensive care units staying patients. Literature searches were performed using the electronic databases Medline, LILACS, CINAHL, Cochrane, High Wire Press and SciELO, from January 1998 to July 2009 and book chapters, using keywords including "critical illness", "cinesiotherapy", "physical therapy", "physiotherapy", "exercises", "training", "force", "active mobilization", "mobilization", "ICU", "rehabilitation", "mobility", "muscle strength" and "weakness". Despite the lack of studies and methodological diversity of studies found, confirming the use of exercise alone as a therapeutic resource, its use, including early seems an alternative to prevent and reverse muscle weakness intensive care unit ICU-acquired.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)