Abstract
Rev Bras Ter Intensiva. 2020;32(3):374-380
DOI 10.5935/0103-507X.20200065
To evaluate whether the decrease in blood pressure caused by the increase in the positive end-expiratory pressure corresponds to the pulse pressure variation as an indicator of fluid responsiveness.
This exploratory study prospectively included 24 patients with septic shock who were mechanically ventilated and subjected to three stages of elevation of the positive end-expiratory pressure: from 5 to 10cmH2O (positive end-expiratory pressure level 1), from 10 to 15cmH2O (positive end-expiratory pressure level 2), and from 15 to 20cmH2O (positive end-expiratory pressure level 3). Changes in systolic blood pressure, mean arterial pressure, and pulse pressure variation were evaluated during the three maneuvers. The patients were classified as responsive (pulse pressure variation ≥ 12%) or unresponsive to volume replacement (pulse pressure variation < 12%).
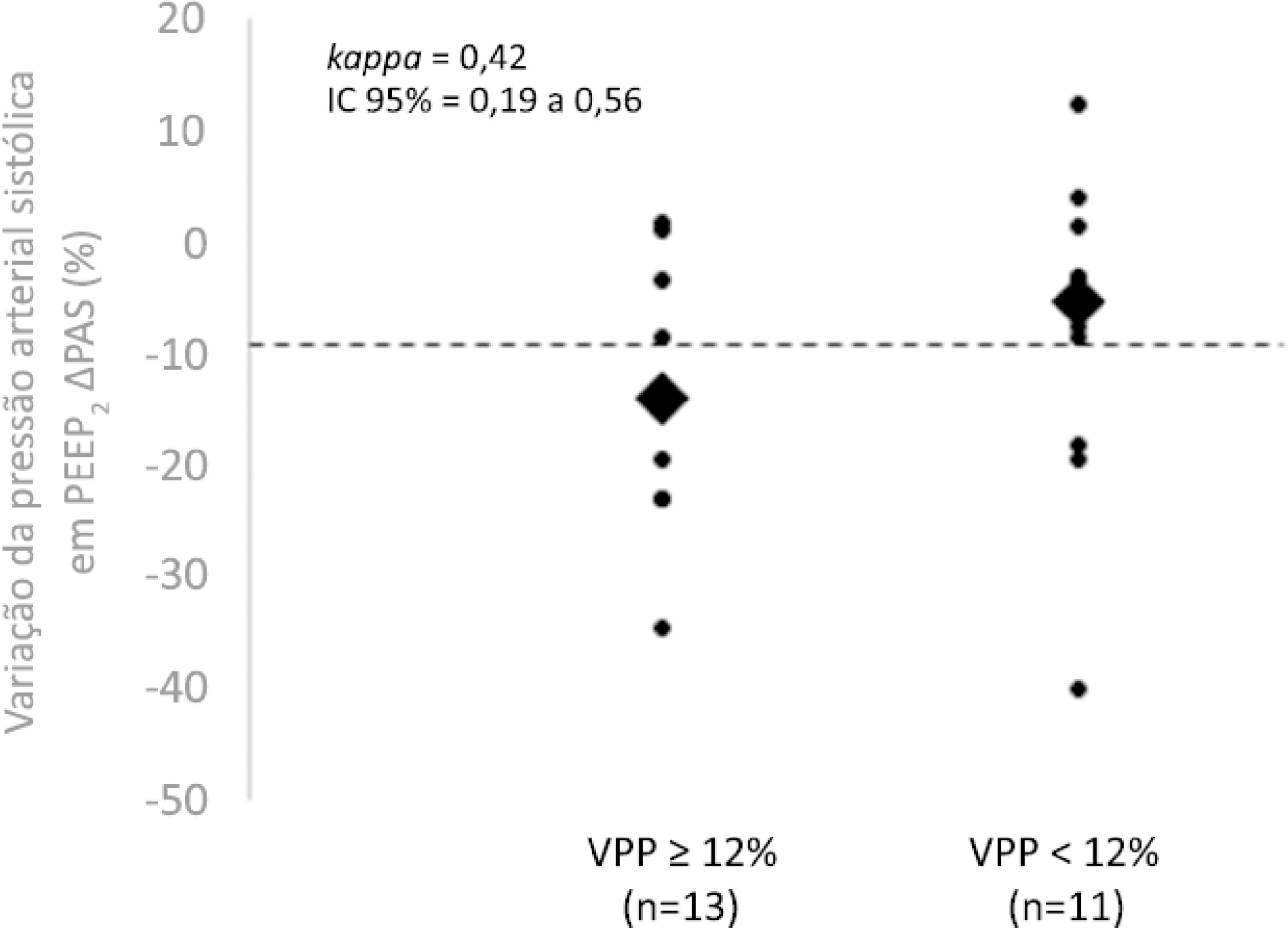
The best performance at identifying patients with pulse pressure variation ≥ 12% was observed at the positive end-expiratory pressure level 2: -9% systolic blood pressure variation (area under the curve 0.73; 95%CI: 0.49 - 0.79; p = 0.04), with a sensitivity of 63% and specificity of 80%. Concordance was low between the variable with the best performance (variation in systolic blood pressure) and pulse pressure variation ≥ 12% (kappa = 0.42; 95%CI: 0.19 - 0.56). The systolic blood pressure was < 90mmHg at positive end-expiratory pressure level 2 in 29.2% of cases and at positive end-expiratory pressure level 3 in 41.63% of cases.
Variations in blood pressure in response to the increase in positive end-expiratory pressure do not reliably reflect the behavior of the pulse pressure as a measure to identify the fluid responsiveness status.