You searched for:"Clarissa Netto Blattner"
We found (3) results for your search.-
Original Article
Postextubation fluid balance is associated with extubation failure: a cohort study
Rev Bras Ter Intensiva. 2021;33(3):422-427
Abstract
Original ArticlePostextubation fluid balance is associated with extubation failure: a cohort study
Rev Bras Ter Intensiva. 2021;33(3):422-427
DOI 10.5935/0103-507X.20210057
Views1ABSTRACT
Objective:
To assess whether there is an association between 48-hour postextubation fluid balance and extubation failure.
Methods:
This was a prospective cohort study that included patients admitted to the intensive care unit of a tertiary hospital in southern Brazil from March 2019 to December 2019. Patients who required mechanical ventilation for at least 24 hours and who were extubated during the study period were included. The primary outcome was extubation failure, considered as the need for reintubation in the first 72 hours after extubation. The secondary outcome was a combined outcome with extubation failure or the need for therapeutic noninvasive ventilation.
Results:
A total of 101 patients were included. Extubation failure was observed in 29 (28.7%) patients. In univariate analysis, patients with a negative 48-hour postextubation fluid balance higher than one liter had a lower rate of extubation failure (12.0%) than patients with a negative 48-hour postextubation fluid balance lower than 1L (34.2%; p = 0.033). Mechanical ventilation duration and negative 48-hour postextubation fluid balance lower than one liter were associated with extubation failure when corrected for Simplified Acute Physiology Score 3 in multivariate analysis. When we evaluated the combined outcome, only negative 48-hour postextubation lower than 1L maintained an association when corrected for for Simplified Acute Physiology Score 3 and mechanical ventilation duration.
Conclusion:
The 48-hour postextubation fluid balance is associated with extubation failure. Further studies are necessary to assess whether avoiding positive fluid balance in this period might improve weaning outcomes.
Keywords:Airway extubationNoninvasive ventilationRespiration, artificialWater-electrolyte balanceWeaningSee more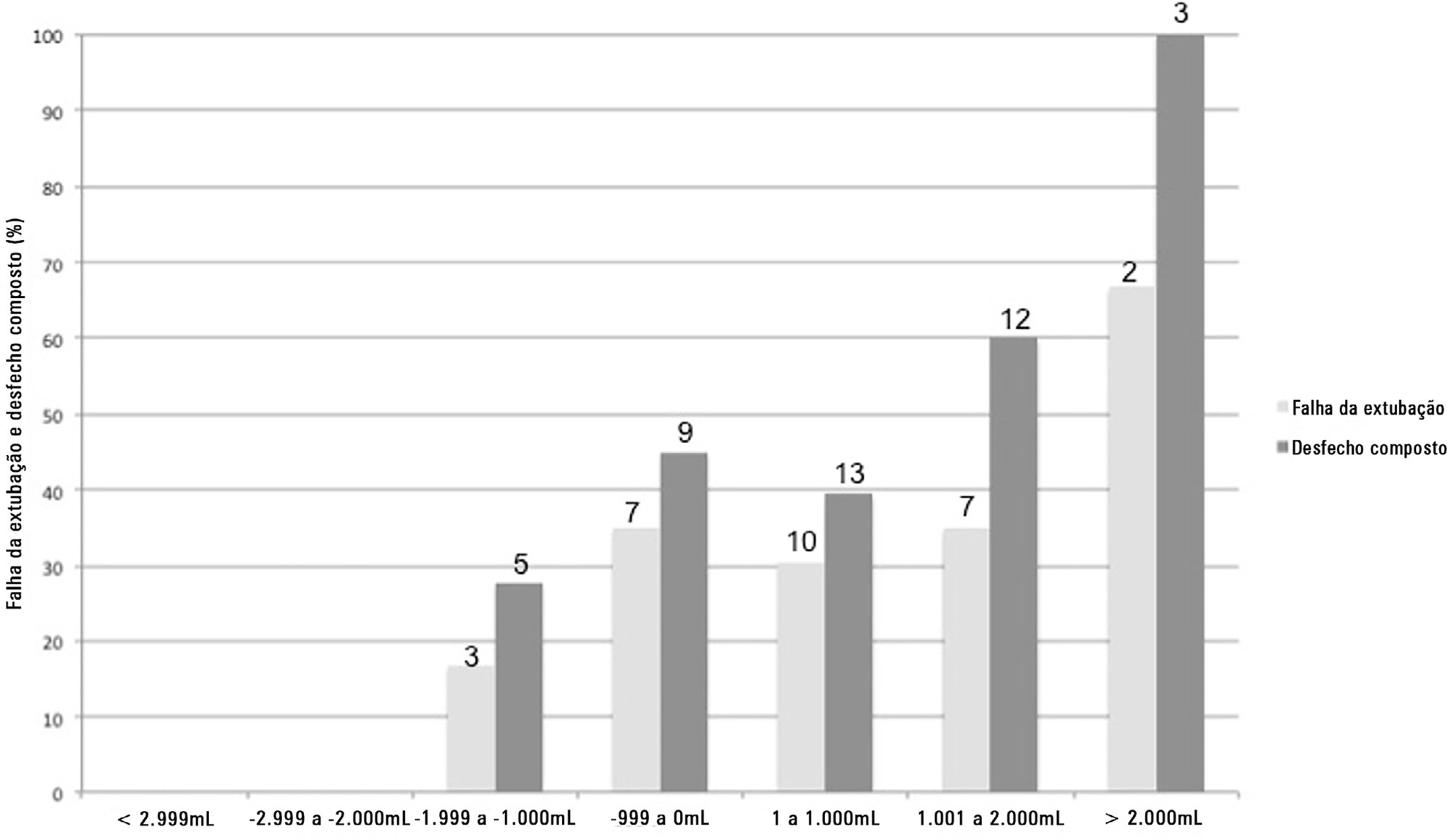
-
Original Articles
Acute bag-valve breathing maneuvers plus manual chest compression is safe during stable septic shock: a randomized clinical trial
Rev Bras Ter Intensiva. 2017;29(1):14-22
Abstract
Original ArticlesAcute bag-valve breathing maneuvers plus manual chest compression is safe during stable septic shock: a randomized clinical trial
Rev Bras Ter Intensiva. 2017;29(1):14-22
DOI 10.5935/0103-507X.20170004
Views1See moreABSTRACT
Objective:
To evaluate the effects of bag-valve breathing maneuvers combined with standard manual chest compression techniques on safety, hemodynamics and oxygenation in stable septic shock patients.
Design:
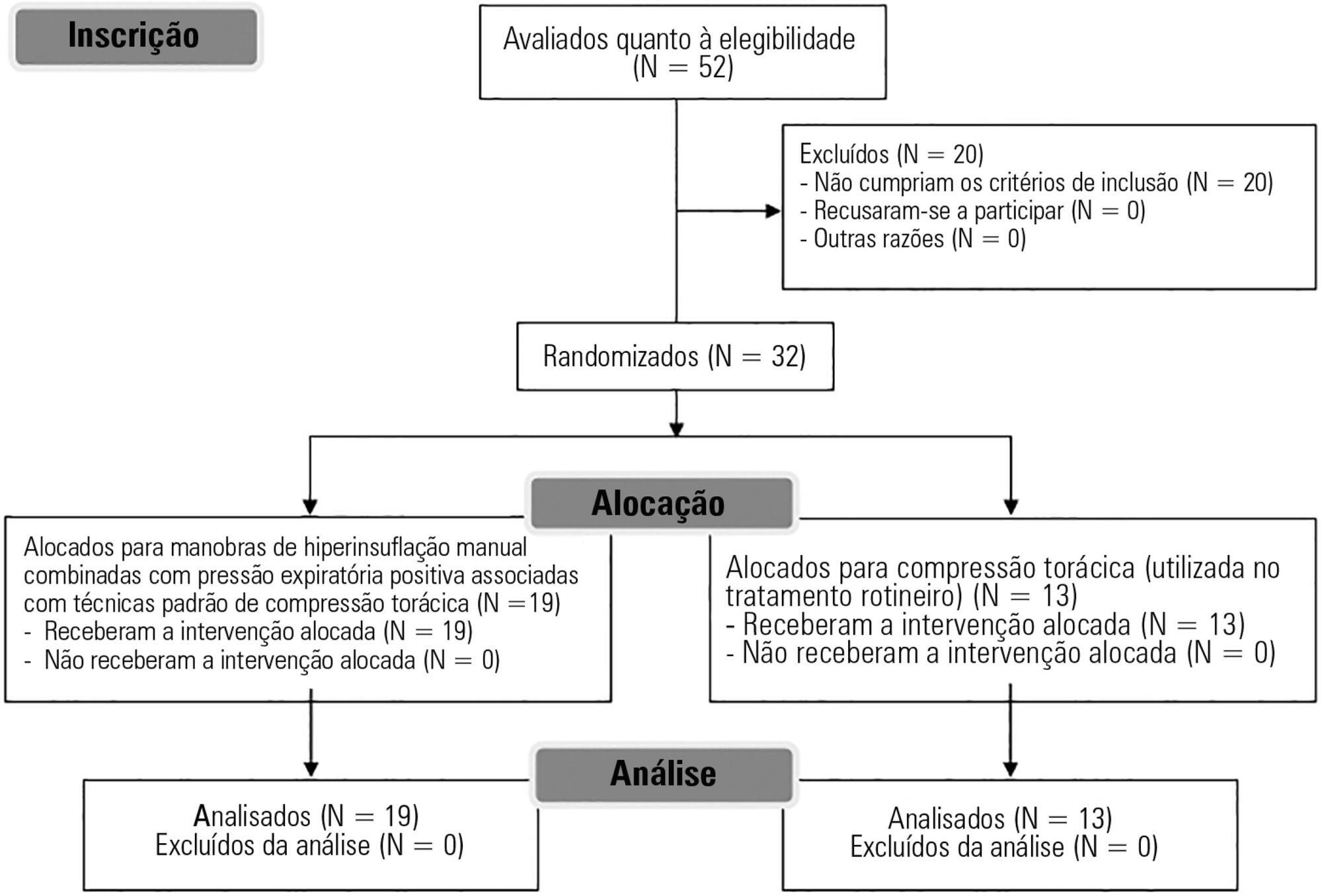
A parallel, assessor-blinded, randomized trial of two groups. A computer-generated list of random numbers was prepared by an independent researcher to allocate treatments.
Setting:
The Intensive Care Unit at Hospital São Lucas, Pontifícia Universidade Católica do Rio Grande do Sul.
Participants:
Fifty-two subjects were assessed for eligibility, and 32 were included. All included subjects (n = 32) received the allocated intervention (n = 19 for the Experimental Group and n = 13 for the Control Group).
Intervention:
Twenty minutes of bag-valve breathing maneuvers combined with manual chest compression techniques (Experimental Group) or chest compression, as routinely used at our intensive care unit (Control Group). Follow-up was performed immediately after and at 30 minutes after the intervention.
Main outcome measure:
Mean artery pressure.
Results:
All included subjects completed the trial (N = 32). We found no relevant effects on mean artery pressure (p = 0.17), heart rate (p = 0.50) or mean pulmonary artery pressure (p = 0.89) after adjusting for subject age and weight. Both groups were identical regarding oxygen consumption after the data adjustment (p = 0.84). Peripheral oxygen saturation tended to increase over time in both groups (p = 0.05), and there was no significant association between cardiac output and venous oxygen saturation (p = 0.813). No clinical deterioration was observed.
Conclusion:
A single session of bag-valve breathing maneuvers combined with manual chest compression is hemodynamically safe for stable septic-shocked subjects over the short-term.
-
Original Articles
Effects of manual hyperinflation maneuver associated with positive end expiratory pressure in patients within coronary artery bypass grafting
Rev Bras Ter Intensiva. 2010;22(1):40-46
Abstract
Original ArticlesEffects of manual hyperinflation maneuver associated with positive end expiratory pressure in patients within coronary artery bypass grafting
Rev Bras Ter Intensiva. 2010;22(1):40-46
DOI 10.1590/S0103-507X2010000100008
Views1OBJECTIVE: To verify the effects of manual hyperinflation maneuver associated with positive end expiratory pressure in coronary artery bypass grafting patients. METHODS: This was a randomized trial, conducted from August 2007 to July 2008 in the intensive care unit of the Hospital Luterano (ULBRA). The patients were divided in the groups intervention – with manual hyperinflation plus positive end expiratory pressure – and controlThe ventilatory variables were measured before and after the manual hyperinflation. The t Student’s test was used for independent and paired samples as well as Fisher’s exact test and McNemar’s Chi-square test with 0.05 significance level. RESULTS: Eighteen patients were included. The mean age was 64± 11 years and 55.6% were female. The inspired tidal volume was 594± 112ml in the intervention group and 487± 51ml in the control group (p=0.024) and the expired tidal volume was 598± 105ml in the intervention group and 490± 58ml in the control group (p=0.02). The mean pre-maneuver static pulmonary compliance in the intervention group was 41.6± 12.1 ml/cmH2O and post maneuver it was 47.4± 16.6 ml/cmH2O (p=0.03). There was no significant between groups difference in the following variables: oxygen peripheral saturation, oxygen arterial pressure, extubation time and radiological changes. CONCLUSION: The results show that the manual hyperinflation associated with positive end expiratory pressure maneuver trends to promote increased lung volumes and static compliance, however these findings require further confirmation.
Keywords:Breathing exercisesMyocardial revascularizationPhysical therapy modalitiesPositive pressure respirationRehabilitationRespiration, artificialRespiratory therapySee more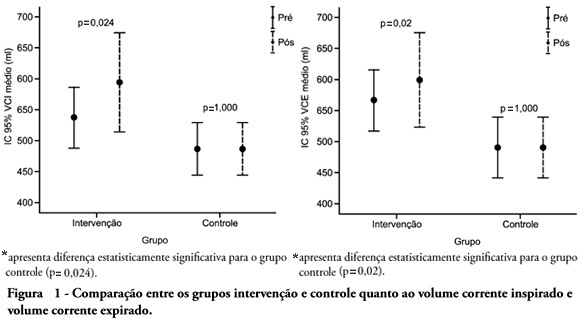
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




