Abstract
Rev Bras Ter Intensiva. 2022;34(2):295-299
DOI 10.5935/0103-507X.20220028-en
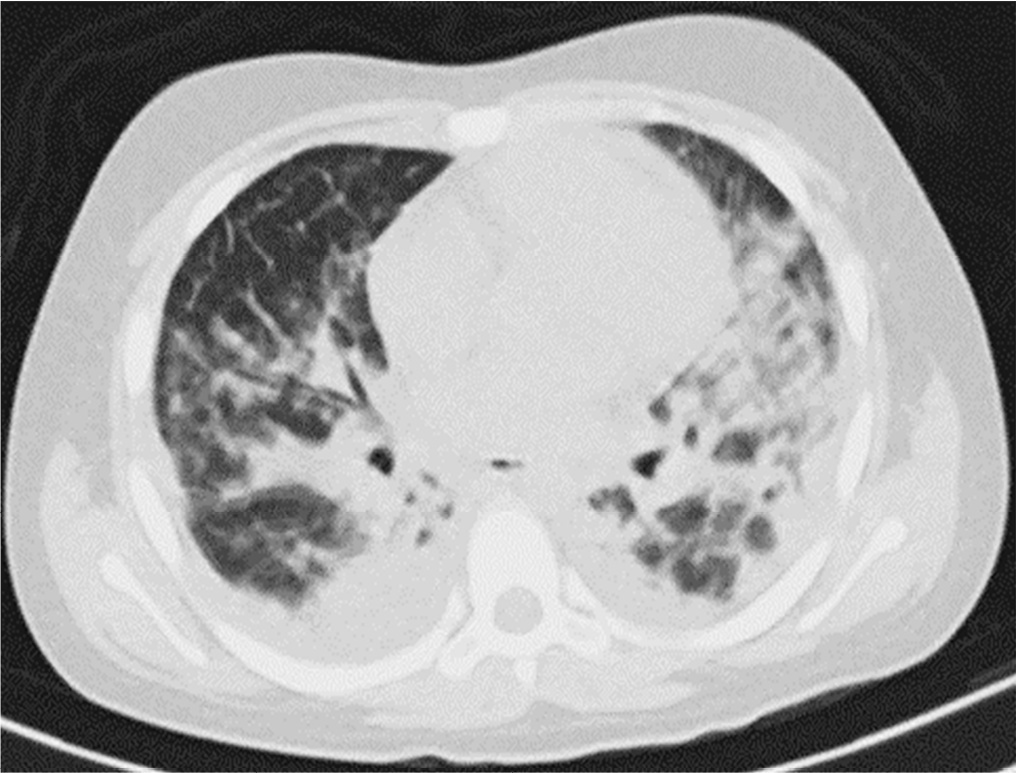
Posterior reversible encephalopathy syndrome is a rare clinical and radiological syndrome characterized by vasogenic edema of the white matter of the occipital and parietal lobes, which are usually symmetrical, resulting from a secondary manifestation of acute dysfunction of the posterior cerebrovascular system. We describe a case of posterior reversible encephalopathy syndrome secondary to SARS-CoV-2 infection in a 9-year-old boy who developed acute hypoxemic respiratory failure and required assisted mechanical ventilation. The child developed multisystem inflammatory syndrome, and he was monitored in the pediatric intensive care unit and was provided mechanical ventilation and vasoactive agents for hemodynamic support. Additionally, he developed pulmonary and extrapulmonary clinical manifestations along with neuropsychiatric manifestations that required close follow-up and were verified using brain magnetic resonance imaging for timely intervention. Currently, there are few reports of children with posterior reversible encephalopathy syndrome associated with multisystem inflammatory syndrome.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):317-324
DOI 10.5935/0103-507X.20170047
This study intended to determine whether the systemic inflammatory response syndrome criteria can predict hospital mortality in a Brazilian cohort of critically ill patients.
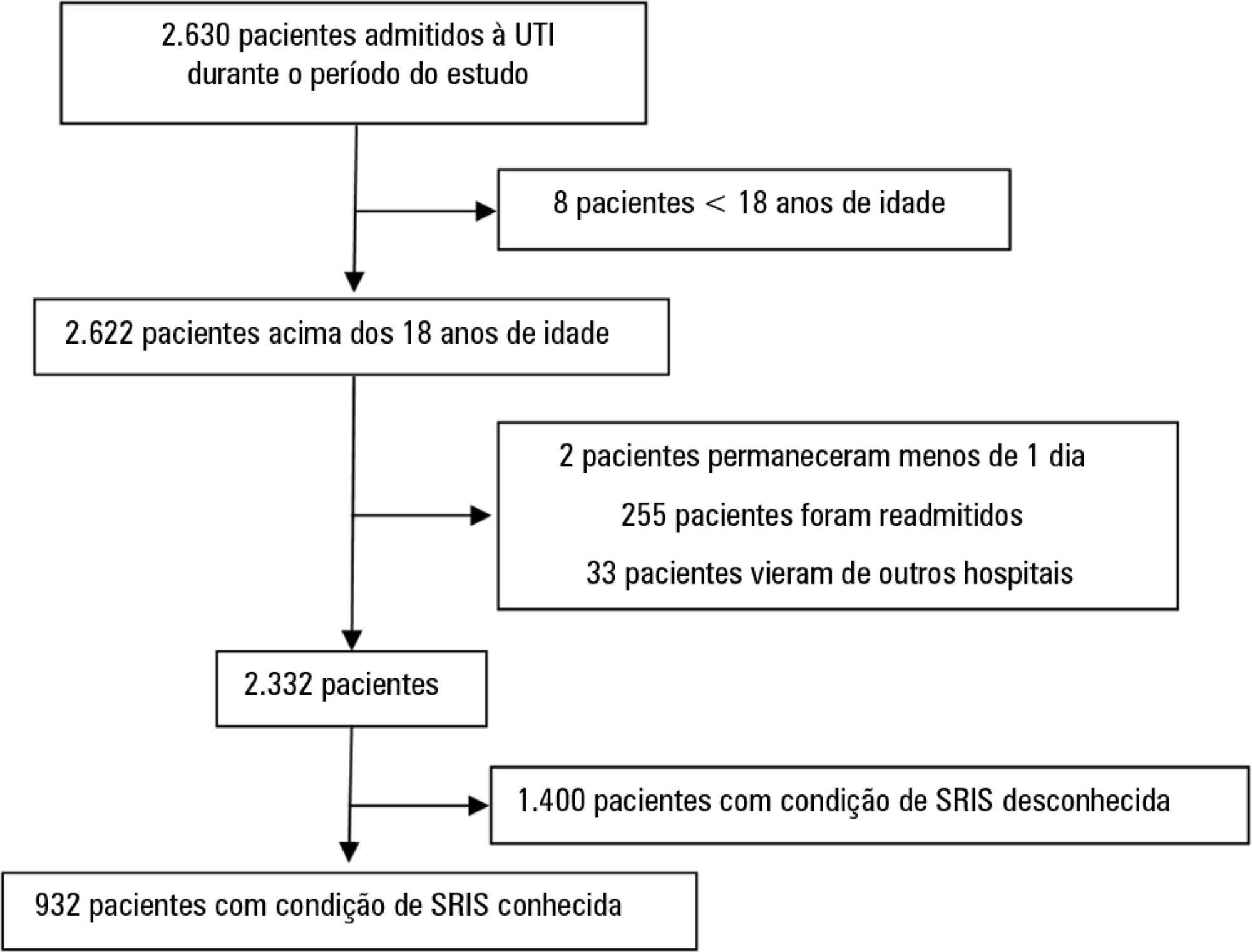
We performed a retrospective cohort study at a private tertiary hospital in São Paulo (SP), Brazil. We extracted information from the adult intensive care unit database (Sistema EpimedTM). We compared the SAPS 3 and the systemic inflammatory response syndrome model as dichotomous (≥ 2 criteria: systemic inflammatory response syndrome -positive versus 0 - 1 criterion: systemic inflammatory response syndrome -negative) and ordinal variables from 0 to 4 (according to the number of systemic inflammatory response syndrome criteria met) in the prediction of hospital mortality at intensive care unit admission. Model discrimination was compared using the area under the receiver operating characteristics (AUROC) curve.
From January to December 2012, we studied 932 patients (60.4% were systemic inflammatory response syndrome -positive). systemic inflammatory response syndrome -positive patients were more critically ill than systemic inflammatory response syndrome -negative patients and had higher hospital mortality (16.9% versus 8.1%, p < 0.001). In the adjusted analysis, being systemic inflammatory response syndrome -positive independently increased the risk of death by 82% (odds ratio 1.82; 95% confidence interval [CI] 1.12 - 2.96, p = 0.016). However, the AUROC curve for the SAPS 3 model was higher (0.81, 95%CI 0.78 - 0.85) compared to the systemic inflammatory response syndrome model with the systemic inflammatory response syndrome criteria as a dichotomous variable (0.60, 95%CI 0.55 - 0.65) and as an ordinal variable (0.62, 95%CI 0.57 - 0.68; p < 0.001) for hospital mortality.
Although systemic inflammatory response syndrome is associated with hospital mortality, the systemic inflammatory response syndrome criteria show low accuracy in the prediction of mortality compared with the SAPS 3.
Abstract
Rev Bras Ter Intensiva. 2011;23(4):426-433
DOI 10.1590/S0103-507X2011000400006
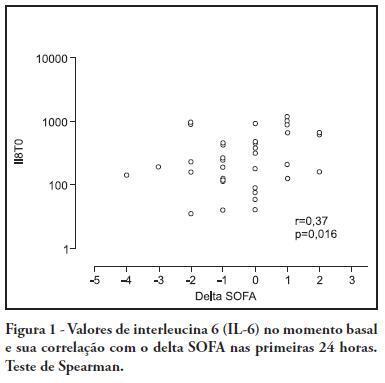
OBJECTIVE: To investigate the correlation of organ dysfunction and its progression with inflammatory response during the early phases of septic shock by assessing baseline cytokine concentrations. METHODS: This study included patients over 18 years old with septic shock within the first 48 hours after the onset of organ dysfunction. Interleukin 6 (IL-6), interleukin 8 (IL-8), interleukin 10 (IL-10) and C-reactive protein levels were assessed at inclusion and after 24 hours, and the differences between these values were calculated. The progression of organ dysfunction was assessed using the Sequential Organ Failure Assessment (SOFA) score upon admission and 24 hours later for a delta-SOFA determination and were categorized as either worsened or improved. The results were expressed as means + standard deviation or median (25-75% percentiles). Values with descriptive p values of 0.05 or less were considered significant. RESULTS: Overall, we included 41 patients with median SOFA scores of 8.0 (6.5-10.0) upon admission (T0) and 8.0 (6.0-10.0) 24 hours later (T1). Worsened, improved or unchanged SOFA scores were observed in 11 (Group 1), 17 (Group 2) and 13 (Group 3) patients, respectively. For Group 1, the baseline IL-6, IL-8 and IL-10 values were higher, and a significant increase of IL-8 levels was found after 24 hours. The change in the SOFA score after 24 hours was significantly, although weakly, correlated with baseline IL-6 and IL-8 concentrations. CONCLUSIONS: Higher baseline IL-6, IL-8 and IL-10 levels are associated with unfavorable organ dysfunction outcomes. Increased IL-8 levels within the first 24 hours are correlated with a worsening dysfunction.
Abstract
Rev Bras Ter Intensiva. 2010;22(3):280-290
DOI 10.1590/S0103-507X2010000300011
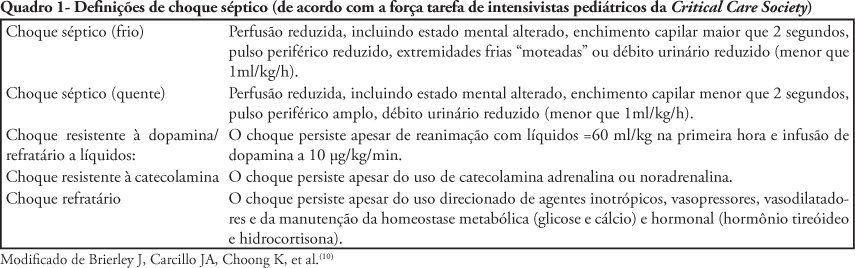
The nonspecific presentation of neonatal sepsis and systemic inflammatory response syndrome preceding septic shock delay the early diagnosis of septic shock and increase its mortality rate. Early diagnosis involves suspecting septic shock in every newborn with tachycardia, respiratory distress, difficult feeding, altered tonus and skin coloration, tachypnea and reduced perfusion, specially in case of maternal peripartum infection, chorioamnionitis or long-term membranes rupture. This article aims to review current knowledge on neonatal period peculiarities, fetal circulation dynamics, and the pregnancy age variable. Newborn septic shock is not just a small adult shock. In the newborn, the septic shock is predominantly cold and characterized by reduced cardiac output and increased systemic vascular resistance (vasoconstriction). Time is fundamental for septic shock reversion. The indexed-databases literature review provides subside for the newborn management.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):128-134
DOI 10.1590/S0103-507X2008000200003
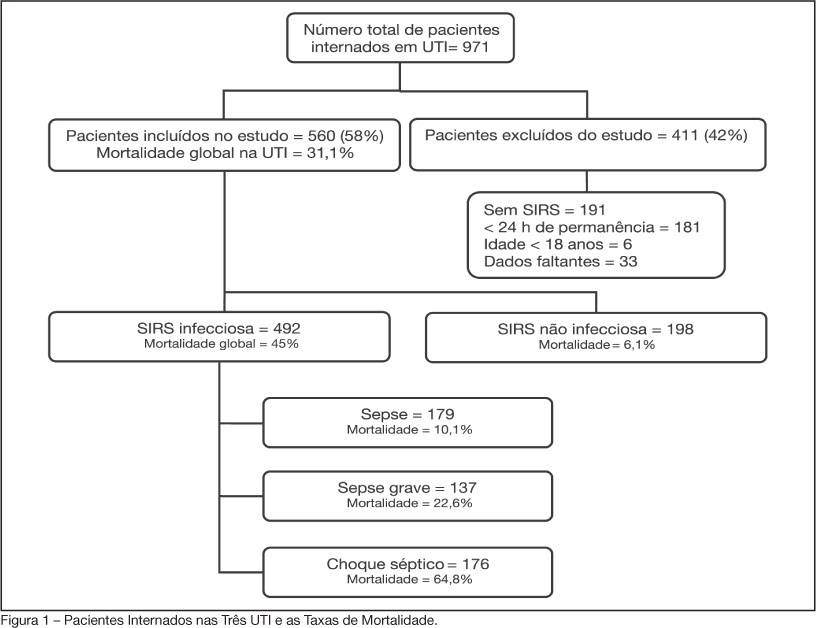
BACKGROUND AND OBJECTIVES: Sepsis is the main cause of death in patients treated in intensive care units (ICU). The aim of this study was to evaluate etiology, prognostic factors and mortality of septic patients treated in ICU of Passo Fundo, Brazil. METHODS: Out of 971 consecutive patients prospectively evaluated from August 2005 to February 2006, 560 were selected due to presence of systemic inflammatory response syndrome (SIRS) and followed for 28 days or until discharge or death. Patients were categorized according with the etiology of SIRS and further classified as having SIRS, sepsis, severe sepsis and septic shock. Prognosis was assessed by means of Apache II and SOFA. Mortality was compared in different etiologies of sepsis, APACHE II and SOFA scores, parameters. RESULTS: Of the 971 patients admitted to the ICU, 560 developed SIRS (58%). The most frequent cause of internation was neurological disease (28.9%), the most frequent site of infection was the respiratory tract (71.6%), and the most prevalent pathogens were gram-negative bacilli (53.2%). Mean APACHE II score was 18 ± 9, and mean SOFA score was 5 ± 4. Median ICU stay was 6 (3-11) days and overall mortality rate was 31.1%: 6.1% for non-infectious SIRS, 10.1% for sepsis, 22.6% for severe sepsis, and 64.8% for septic shock. CONCLUSIONS: Sepsis is an important health problem that leads to an extremely high mortality rate in the ICU of Passo Fundo, Brazil.
Abstract
Rev Bras Ter Intensiva. 2007;19(2):210-215
DOI 10.1590/S0103-507X2007000200012
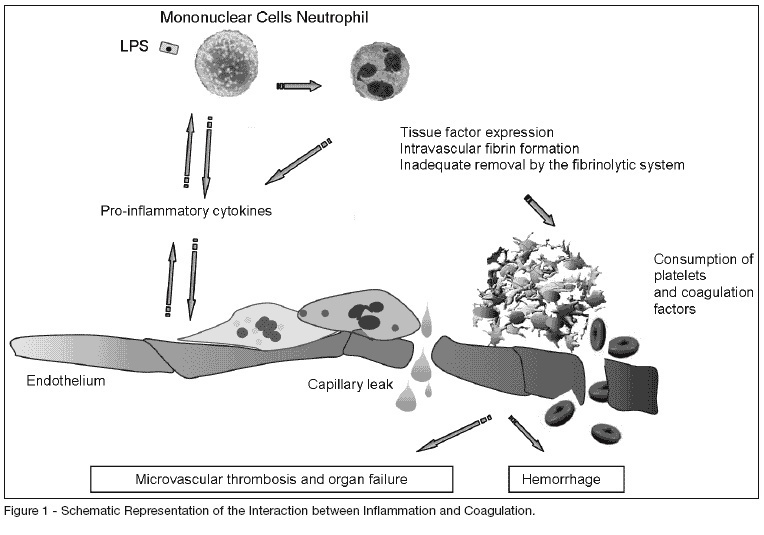
BACKGROUND AND OBJECTIVES: Sepsis is the expression of a complex network of mediators. Multiple organ dysfunction and septic shock indeed remain a major cause of death among ICU patients worldwide. Prompt recognition of both the diagnosis and the complicated evolution are essential, hence the importance of using biological markers. The main pro-inflammatory and anti-inflammatory cytokines as well as hundreds of others cellular markers, circulating bioactive molecules or coagulation products are potential biological markers that could help to characterize the presence of infection and sepsis. We aimed to review the main biological markers that could be used nowadays or possibly in the future, either in clinical or research fields. CONTENTS: A selective review of biologic markers of sepsis focusing on markers of the coagulation cascade, C-reactive protein and procalcitonin. CONCLUSIONS: Most of the available biological markers is still not a practical method to be used at the bed-side and is currently restricted to research works. Nowadays the determination of CRP or PCT serum levels can be of great help in the critically ill patient care along with the conventional parameters.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (115) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)