You searched for:"Carolina Kosour"
We found (4) results for your search.-
Original Article
Atrial natriuretic factor: is it responsible for hyponatremia and natriuresis in neurosurgery?
Rev Bras Ter Intensiva. 2016;28(2):154-160
Abstract
Original ArticleAtrial natriuretic factor: is it responsible for hyponatremia and natriuresis in neurosurgery?
Rev Bras Ter Intensiva. 2016;28(2):154-160
DOI 10.5935/0103-507X.20160030
Views0See moreABSTRACT
Objective:
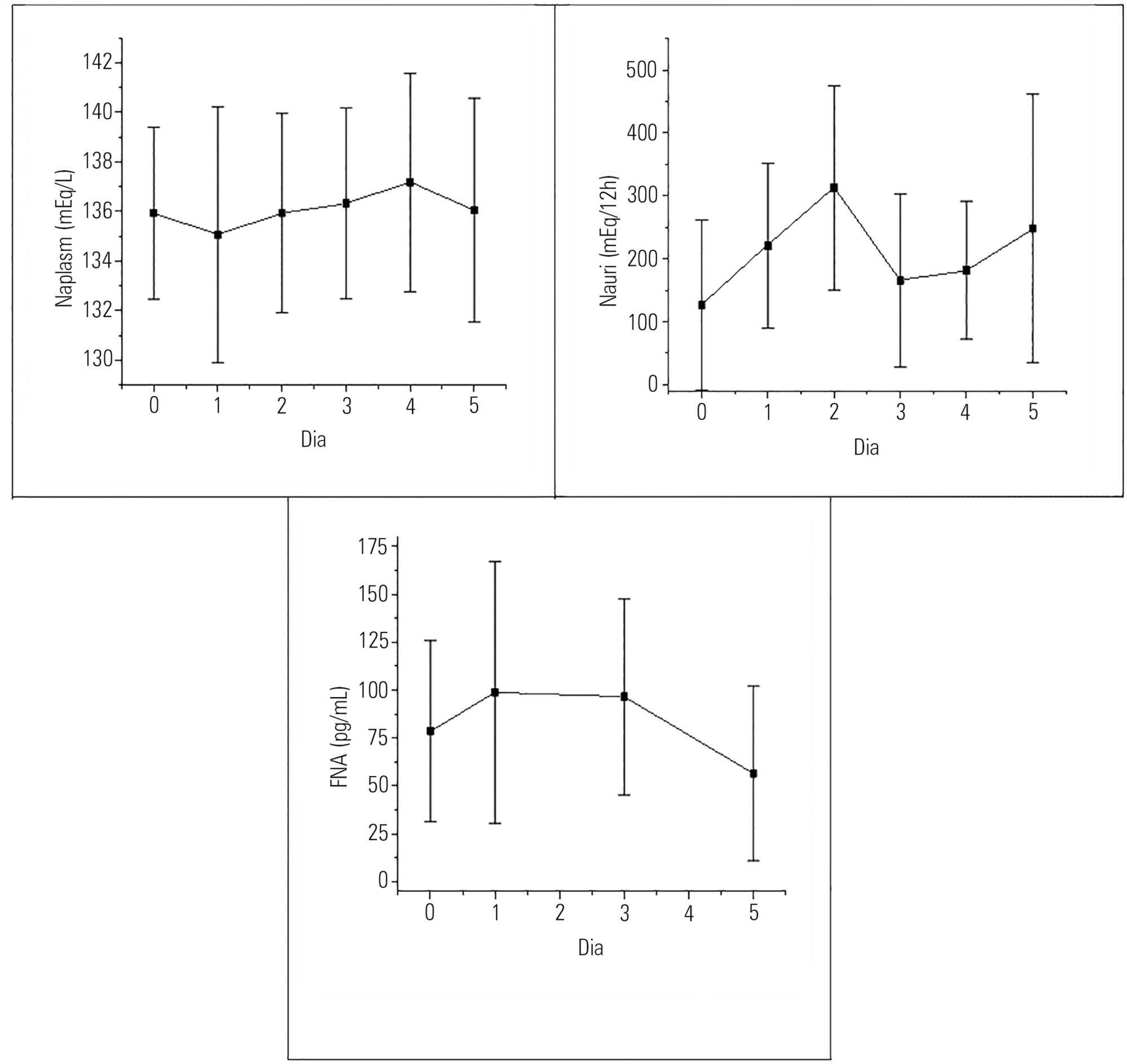
To evaluate the presence of hyponatremia and natriuresis and their association with atrial natriuretic factor in neurosurgery patients.
Methods:
The study included 30 patients who had been submitted to intracranial tumor resection and cerebral aneurism clipping. Both plasma and urinary sodium and plasma atrial natriuretic factor were measured during the preoperative and postoperative time periods.
Results:
Hyponatremia was present in 63.33% of the patients, particularly on the first postoperative day. Natriuresis was present in 93.33% of the patients, particularly on the second postoperative day. Plasma atrial natriuretic factor was increased in 92.60% of the patients in at least one of the postoperative days; however, there was no statistically significant association between the atrial natriuretic factor and plasma sodium and between the atrial natriuretic factor and urinary sodium.
Conclusion:
Hyponatremia and natriuresis were present in most patients after neurosurgery; however, the atrial natriuretic factor cannot be considered to be directly responsible for these alterations in neurosurgery patients. Other natriuretic factors are likely to be involved.
-
Original Articles – Clinical Research
Use of non-invasive ventilation in acute pulmonary edema and chronic obstructive pulmonary disease exacerbation in emergency medicine: predictors of failure
Rev Bras Ter Intensiva. 2012;24(3):278-283
Abstract
Original Articles – Clinical ResearchUse of non-invasive ventilation in acute pulmonary edema and chronic obstructive pulmonary disease exacerbation in emergency medicine: predictors of failure
Rev Bras Ter Intensiva. 2012;24(3):278-283
DOI 10.1590/S0103-507X2012000300012
Views0OBJECTIVE: This study analyzed acute respiratory failure caused by acute pulmonary edema, as well as chronic obstructive pulmonary disease exacerbation, that was treated with non-invasive mechanical ventilation to identify the factors that are associated with the success or failure non-invasive mechanical ventilation in urgent and emergency service. METHODS: This study was a prospective, descriptive and analytical study. We included patients of both genders aged >18 years who used non-invasive mechanical ventilation due to acute respiratory failure that was secondary to acute pulmonary edema or chronic obstructive pulmonary disease exacerbation. Patients with acute respiratory failure that was secondary to pathologies other than acute pulmonary edema and chronic obstructive pulmonary disease or who presented with contraindications for the technique were excluded. Expiratory pressures between 5 and 8 cmH2O and inspiratory pressures between 10 and 12 cmH2O were used. Supplemental oxygen maintained peripheral oxygen saturation at >90%. The primary outcome was endotracheal intubation. RESULTS: A total of 152 patients were included. The median non-invasive mechanical ventilation time was 6 hours (range 1 – 32 hours) for chronic obstructive pulmonary disease patients (n=60) and 5 hours (range 2 – 32 hours) for acute pulmonary edema patients (n=92). Most (75.7%) patients progressed successfully. However, reduced APACHE II scores and lower peripheral oxygen saturation were observed. These results were statistically significant in patients who progressed to intubation (p<0.001). BiPAP (Bi-level Positive Airway Pressure portable ventilator), as continuous positive airway pressure use increased the probability of endotracheal intubation 2.3 times (p=0.032). Patients with acute pulmonary edema and elevated GCS scores also increased the probability of success. CONCLUSION: Respiratory frequency >25 rpm, higher APACHE II scores, BiPAP use and chronic obstructive pulmonary disease diagnosis were associated with endotracheal intubation. Higher GCS and SpO2 values were associated with NIV success. Non-invasive mechanical ventilation can be used in emergency services in acute respiratory failure cases caused by acute pulmonary edema and chronic obstructive pulmonary disease exacerbation, but patients with variables related to a higher percentage of endotracheal intubation should be specially monitored.
Keywords:Continuous positive airway pressureEmergencyPulmonary disease, chronic obstructivePulmonary edemaRespiratory insufficiencySee more -
Original Articles – Clinical Research
The effects of orthostatism in adult intensive care unit patients
Rev Bras Ter Intensiva. 2012;24(1):64-70
Abstract
Original Articles – Clinical ResearchThe effects of orthostatism in adult intensive care unit patients
Rev Bras Ter Intensiva. 2012;24(1):64-70
DOI 10.1590/S0103-507X2012000100010
Views0See moreOBJECTIVE: To assess the consciousness level, pulmonary and hemodynamic effects of orthostatic position in intensive care patients. METHODS: This study was conducted from April 2008 to July 2009 in the Adult Intensive Care Unit, Hospital das Clínicas, Universidade Estadual de Campinas, São Paulo, Brazil. Fifteen patients were included who were mechanically ventilated for more than seven days and had the following characteristics: tracheotomized; receiving intermittent nebulization; maximal inspiratory pressure of less than -25 cm H2O; Tobin score less than 105; preserved respiratory drive; not sedated; partial arterial oxygen pressure greater than 70 mm Hg; oxygen saturation greater than 90%; and hemodynamically stable. With inclinations of 0º, 30º and 50º, the following parameters were recorded: consciousness level; blinking reflex; thoracoabdominal cirtometry; vital capacity; tidal volume; minute volume; respiratory muscle strength; and vital signs. RESULTS: No neurological level changes were observed. Respiratory rate and minute volume (V E) decreased at 30% and later increased at 50%; however, these changes were not statistically significant. Abdominal cirtometry and maximal expiratory pressure increased, but again, the changes were not statistically significant. Regarding maximal inspiratory pressure and vital capacity, statistically significant increases were seen in the comparison between the 50º and 0º inclinations. However, tidal volume increased with time in the comparisons between 30º and 0º and between 50º and 0º. Mean blood pressure increased only for the comparison of 50º versus 0º. Heart rate increased with time for the comparisons between 30º and 0º, between 50º and 0º and between 50º and 30º. CONCLUSION: Passive orthostatism resulted in improved tidal volume and vital capacity, maximal inspiratory pressure and increased heart rate and mean blood pressure in critically ill patients.
-
The influence of noise levels on the perception of stress in heart disease patients
Rev Bras Ter Intensiva. 2011;23(1):62-67
Abstract
The influence of noise levels on the perception of stress in heart disease patients
Rev Bras Ter Intensiva. 2011;23(1):62-67
DOI 10.1590/S0103-507X2011000100011
Views0OBJECTIVES: To identify the main causes of stress in patients staying in a coronary unit and to assess the influence of noise levels on their perception of stress. METHODS: This was a prospective, descriptive and quantitative study conducted between June and November 2009 in the Coronary Unit of the Hospital de Clínicas da Universidade Estadual de Campinas. The Intensive Care Unit Environmental Stressor Scale was used on the first, second and third days of hospitalization to identify stressors. The noise level was measured on the first and second nights using an Instrutherm DEC-460 decibel meter. RESULTS: Overall, 32 clinical heart disease patients were included. The median Intensive Care Unit Environmental Stressor Scale scores were 67.5, 60.5 and 59.5 for the first, second and third days, respectively. The differences were not statistically significant. The highest noise level (a median of 58.7 dB) was detected on the second night at 9:00 pm; the lowest level (51.5 dB) was measured on the first night at 12:00 am. In a multiple linear regression model, the first-night noise level had a 33% correlation with the second-day stress scale score, and for the second night, the correlation with the third-day stress scale score was 32.8% (p = 0.001). CONCLUSION: Patients admitted into a coronary unit have an increased perception of stress. Higher noise levels are also responsible for the perception of stress in these patients.
Keywords:Critical careHeart diseasesHumanization of assistanceIntensive care unitsPatient satisfactionSound contaminationSee more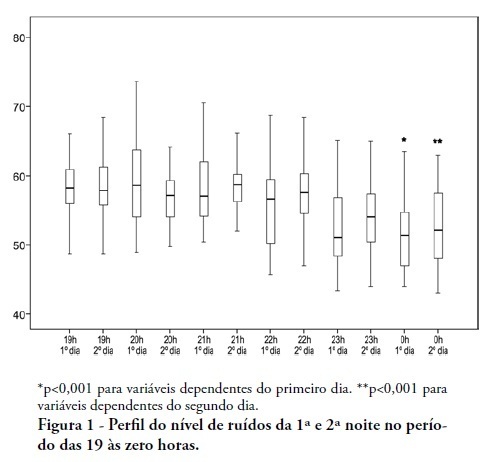
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




