Abstract
Rev Bras Ter Intensiva. 2018;30(1):98-111
DOI 10.5935/0103-507X.20180016
The follow-up of patients who are discharged from intensive care units follows distinct flows in different parts of the world. Outpatient clinics or post-intensive care clinics represent one of the forms of follow-up, with more than 20 years of experience in some countries. Qualitative studies that followed up patients in these outpatient clinics suggest more encouraging results than quantitative studies, demonstrating improvements in intermediate outcomes, such as patient and family satisfaction. More important results, such as mortality and improvement in the quality of life of patients and their families, have not yet been demonstrated. In addition, which patients should be indicated for these outpatient clinics? How long should they be followed up? Can we expect an improvement of clinical outcomes in these followed-up patients? Are outpatient clinics cost-effective? These are only some of the questions that arise from this form of follow-up of the survivors of intensive care units. This article aims to review all aspects relating to the organization and performance of post-intensive care outpatient clinics and to provide an overview of studies that evaluated clinical outcomes related to this practice.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):63-69
DOI 10.5935/0103-507X.20170010
To determine the impact of the day and time of admission and discharge from the intensive care unit on mortality.
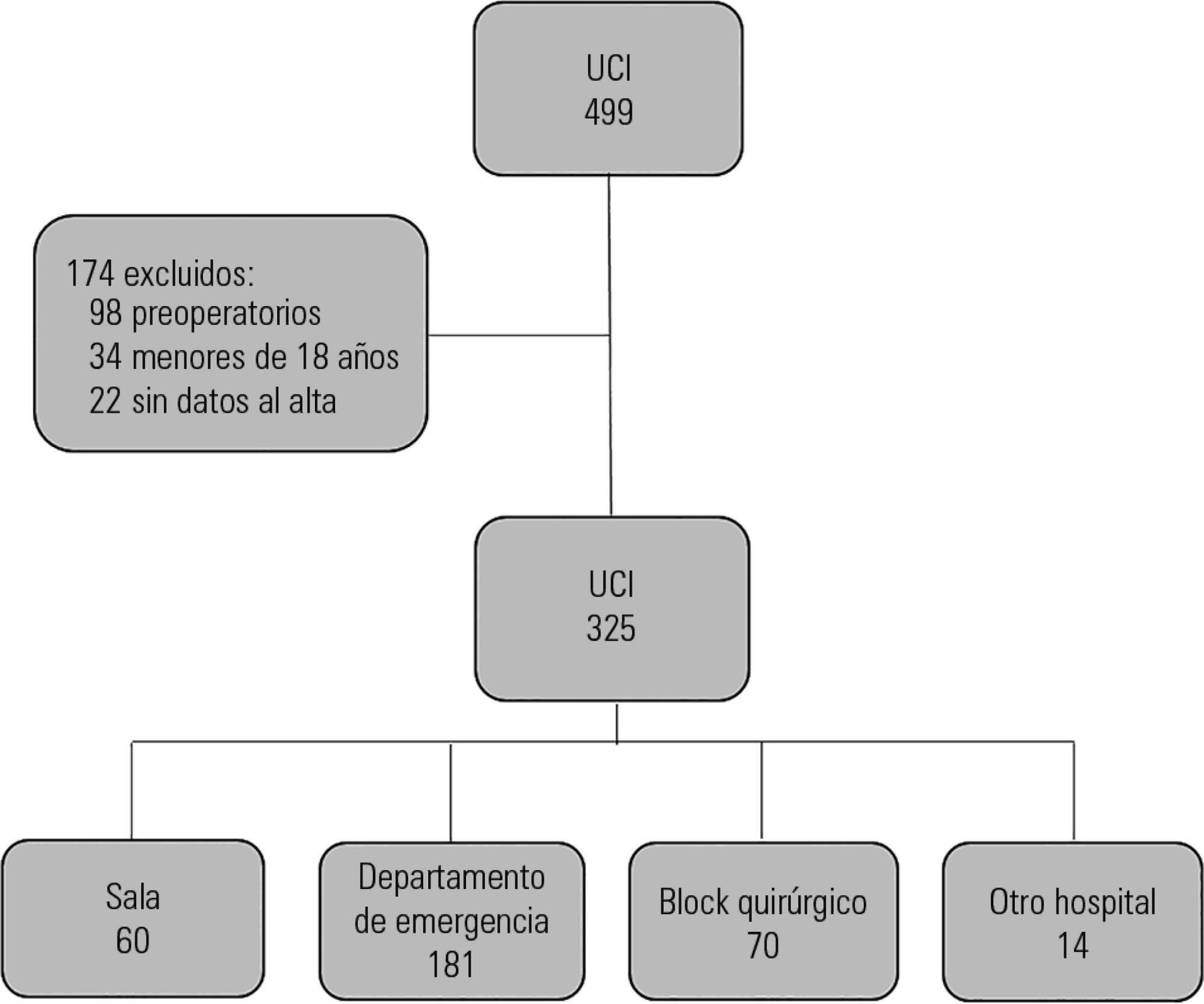
Prospective observational study that included patients admitted to the intensive care unit of the Hospital Maciel in Montevideo between April and November 2014.
We analyzed 325 patients with an average age of 55 (36 - 71) years and a SAPS II value of 43 (29 - 58) points. No differences were found in the mortality of patients in the intensive care unit when time of admission (35% on the weekend versus 31% on weekdays, p = ns) or the hour of entry (35% at night versus 31% in the daytime, p = ns) were compared. The time of discharge was associated with higher hospital mortality rates (57% for weekend discharges versus 14% for weekday discharges, p = 0.000). The factors independently associated with hospital mortality after discharge from the intensive care unit were age > 50 years (OR 2.4, 95%CI, 1.1 - 5.4) and weekend discharge (OR 7.7, 95%CI, 3.8-15.6).
This study identified the time of discharge from the intensive care unit as a factor that was independently associated with hospital mortality.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):51-56
DOI 10.5935/0103-507X.20150009
To assess the causes and factors associated with the death of patients between intensive care unit discharge and hospital discharge.
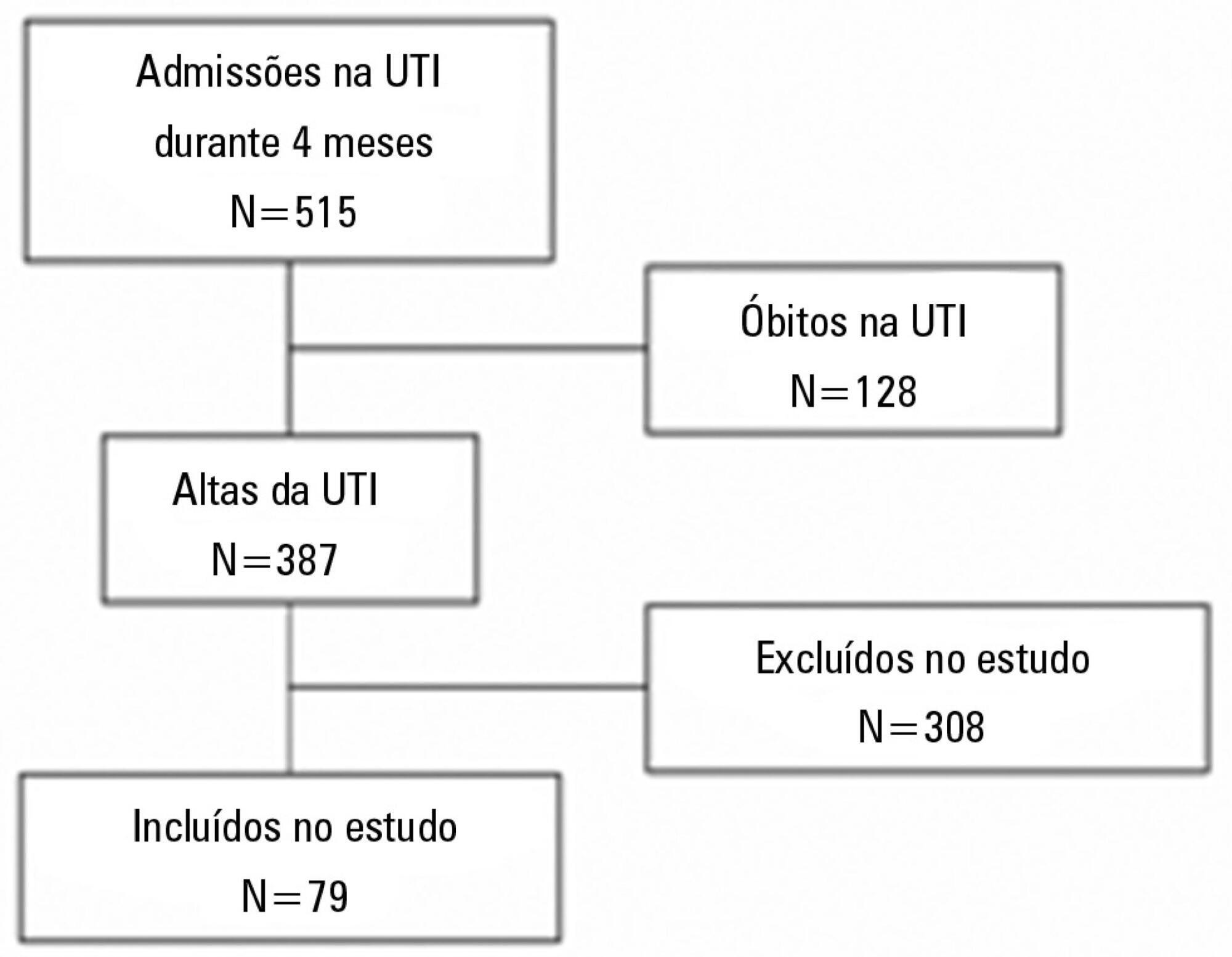
The present is a pilot, retrospective, observational cohort study. The records of all patients admitted to two units of a public/private university hospital from February 1, 2013 to April 30, 2013 were assessed. Demographic and clinical data, risk scores and outcomes were obtained from the Epimed monitoring system and confirmed in the electronic record system of the hospital. The relative risk and respective confidence intervals were calculated.
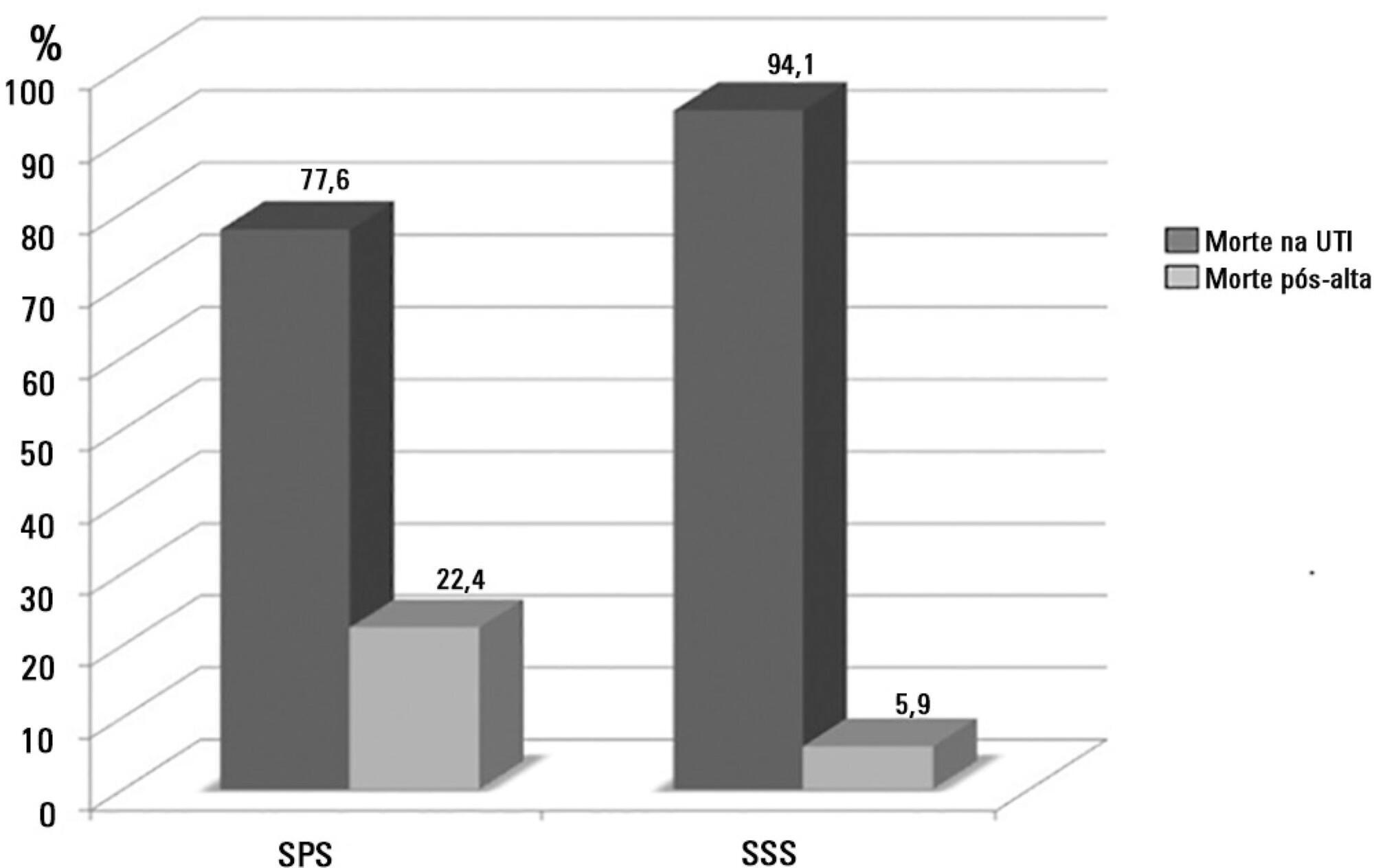
A total of 581 patients were evaluated. The mortality rate in the intensive care unit was 20.8% and in the hospital was 24.9%. Septic shock was the cause of death in 58.3% of patients who died after being discharged from the intensive care unit. Of the patients from the public health system, 73 (77.6%) died in the intensive care unit and 21 (22.4%) died in the hospital after being discharged from the unit. Of the patients from the Supplementary Health System, 48 (94.1%) died in the intensive care unit and 3 (5.9%) died in the hospital after being discharged from the unit (relative risk, 3.87%; 95% confidence interval, 1.21 - 12.36; p < 0.05). The post-discharge mortality rate was significantly higher in patients with intensive care unit hospitalization time longer than 6 days.
The main cause of death of patients who were discharged from the intensive care unit and died in the ward before hospital discharge was septic shock. Coverage by the public healthcare system and longer hospitalization time in the intensive care unit were factors associated with death after discharge from the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):32-38
DOI 10.1590/S0103-507X2013000100007
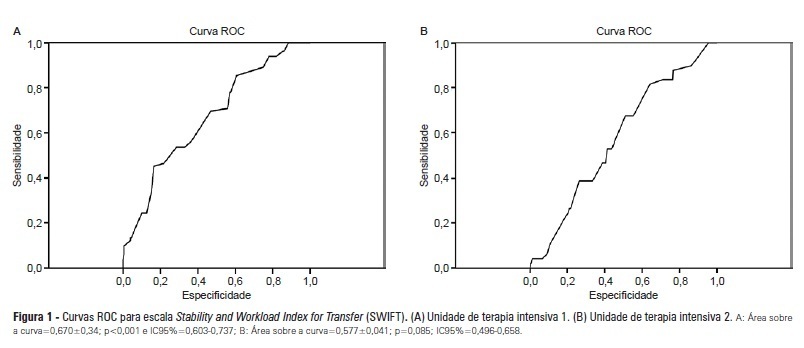
OBJECTIVES: Identify patients at risk for intensive care unit readmission, the reasons for and rates of readmission, and mortality after their stay in the intensive care unit; describe the sensitivity and specificity of the Stability and Workload Index for Transfer scale as a criterion for discharge from the intensive care unit. METHODS: Adult, critical patients from intensive care units from two public hospitals in Porto Alegre, Brazil, comprised the sample. The patients' clinical and demographic characteristics were collected within 24 hours of admission. They were monitored until their final outcome on the intensive care unit (death or discharge) to apply the Stability and Workload Index for Transfer. The deaths during the first intensive care unit admission were disregarded, and we continued monitoring the other patients using the hospitals' electronic systems to identify the discharges, deaths, and readmissions. RESULTS: Readmission rates were 13.7% in intensive care unit 1 (medical-surgical, ICU1) and 9.3% in intensive care unit 2 (trauma and neurosurgery, ICU2). The death rate following discharge was 12.5% from ICU1 and 4.2% from ICU2. There was a statistically significant difference in Stability and Workload Index for Transfer (p<0.05) regarding the ICU1 patients' outcome, which was not found in the ICU2 patients. In ICU1, 46.5% (N=20) of patients were readmitted very early (within 48 hours of discharge). Mortality was high among those readmitted: 69.7% in ICU1 and 48.5% in ICU2. CONCLUSIONS: The Stability and Workload Index for Transfer scale showed greater efficacy in identifying patients more prone to readmission and death following discharge from a medical-surgical intensive care unit. The patients' intensive care unit readmission during the same hospitalization resulted in increased morbidity, mortality, length of stay, and total costs.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):218-224
DOI 10.5935/0103-507X.20130038
To assess the functional and psychological features of patients immediately after discharge from the intensive care unit.
Prospective cohort study. Questionnaires and scales assessing the degree of dependence and functional capacity (modified Barthel and Karnofsky scales) and psychological problems (Hospital Anxiety and Depression Scale), in addition to the Epworth Sleepiness Scale, were administered during interviews conducted over the first week after intensive care unit discharge, to all survivors who had been admitted to this service from August to November 2012 and had remained longer than 72 hours.
The degree of dependence as measured by the modified Barthel scale increased after intensive care unit discharge compared with the data before admission (57±30 versus 47±36; p<0.001) in all 79 participants. This impairment was homogeneous among all the categories in the modified Barthel scale (p<0.001) in the 64 participants who were independent or partially dependent (Karnofsky score ≥40) before admission. The impairment affected the categories of personal hygiene (p=0.01) and stair climbing (p=0.04) only in the 15 participants who were highly dependent (Karnofsky score <40) before admission. Assessment of the psychological changes identified mood disorders (anxiety and/or depression) in 31% of the sample, whereas sleep disorders occurred in 43.3%.
Patients who remained in an intensive care unit for 72 hours or longer exhibited a reduced functional capacity and an increased degree of dependence during the first week after intensive care unit discharge. In addition, the incidence of depressive symptoms, anxiety, and sleep disorders was high among that population.