Abstract
Rev Bras Ter Intensiva. 2021;33(1):138-145
DOI 10.5935/0103-507X.20210015
To double the percentage of time within the 100 - 180mg/dL blood glucose range in the first three months following a phased implementation of a formal education program, and then, of an insulin therapy protocol, without entailing an increased incidence of hypoglycemia.
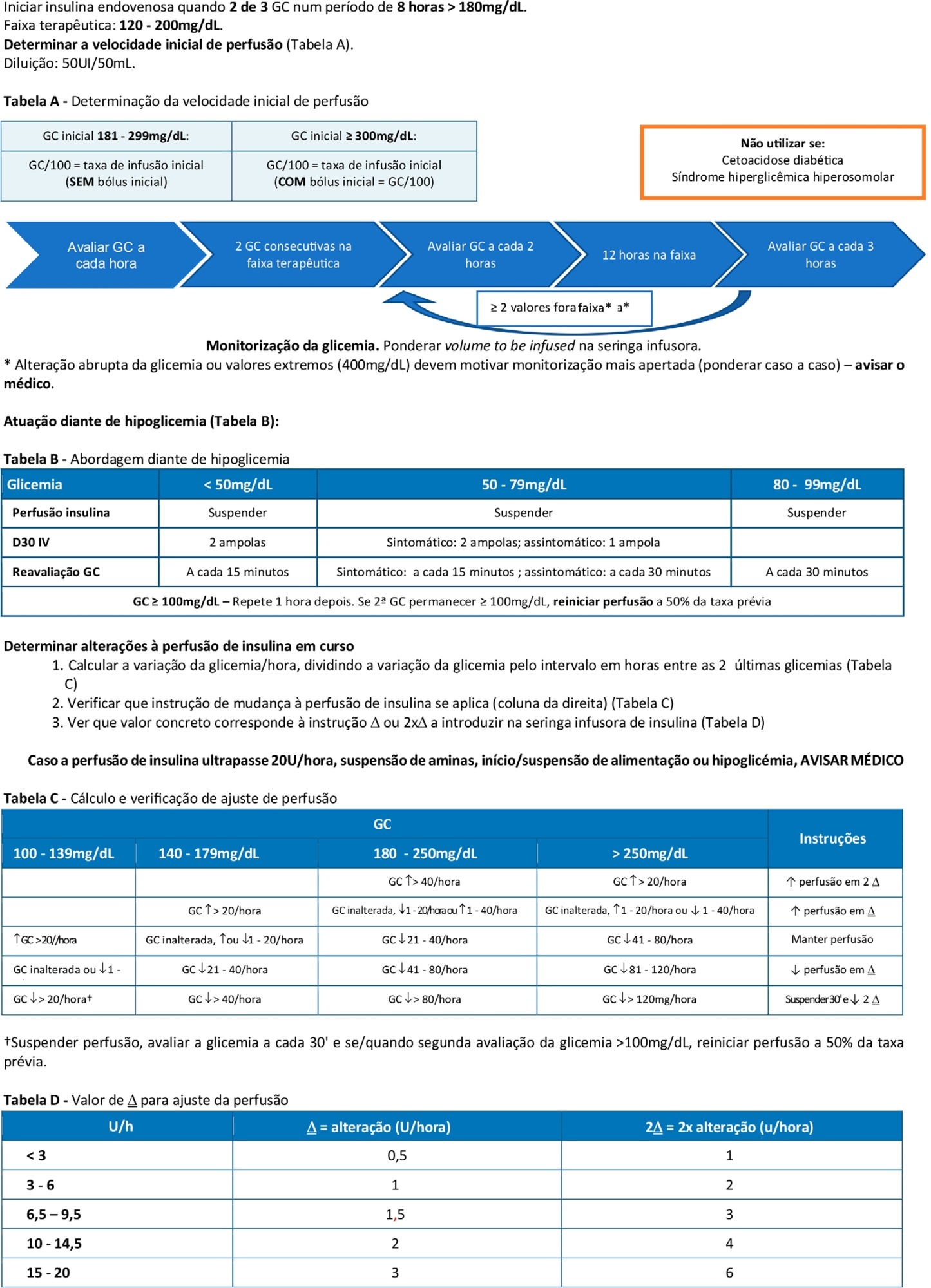
The pre-intervention glycemic control was assessed retrospectively. Next, were carried out the implementation of a formal education program, distribution of manual algorithms for intravenous insulin therapy - optimized by the users, based on the modified Yale protocol - and informal training of the nursing staff. The use of electronic blood glucose control systems was supported, and the results were recorded prospectively.
The first phase of the program (formal education) lead to improvement of the time within the euglycemic interval (28% to 37%). In the second phase, euglycemia was achieved 66% of the time, and the incidence of hypoglycemia was decreased. The percentage of patients on intravenous insulin infusion at 48 hours from admission increased from 6% to 35%.
The phased implementation of a formal education program, fostering the use of electronic insulin therapy protocols and dynamic manuals, received good adherence and has shown to be safe and effective for blood glucose control in critically ill patients, with a concomitant decrease in hypoglycemia.
Abstract
Rev Bras Ter Intensiva. 2018;30(4):471-478
DOI 10.5935/0103-507X.20180068
To analyze the association between glycemia levels upon pediatric intensive care unit admission and mortality in patients hospitalized.
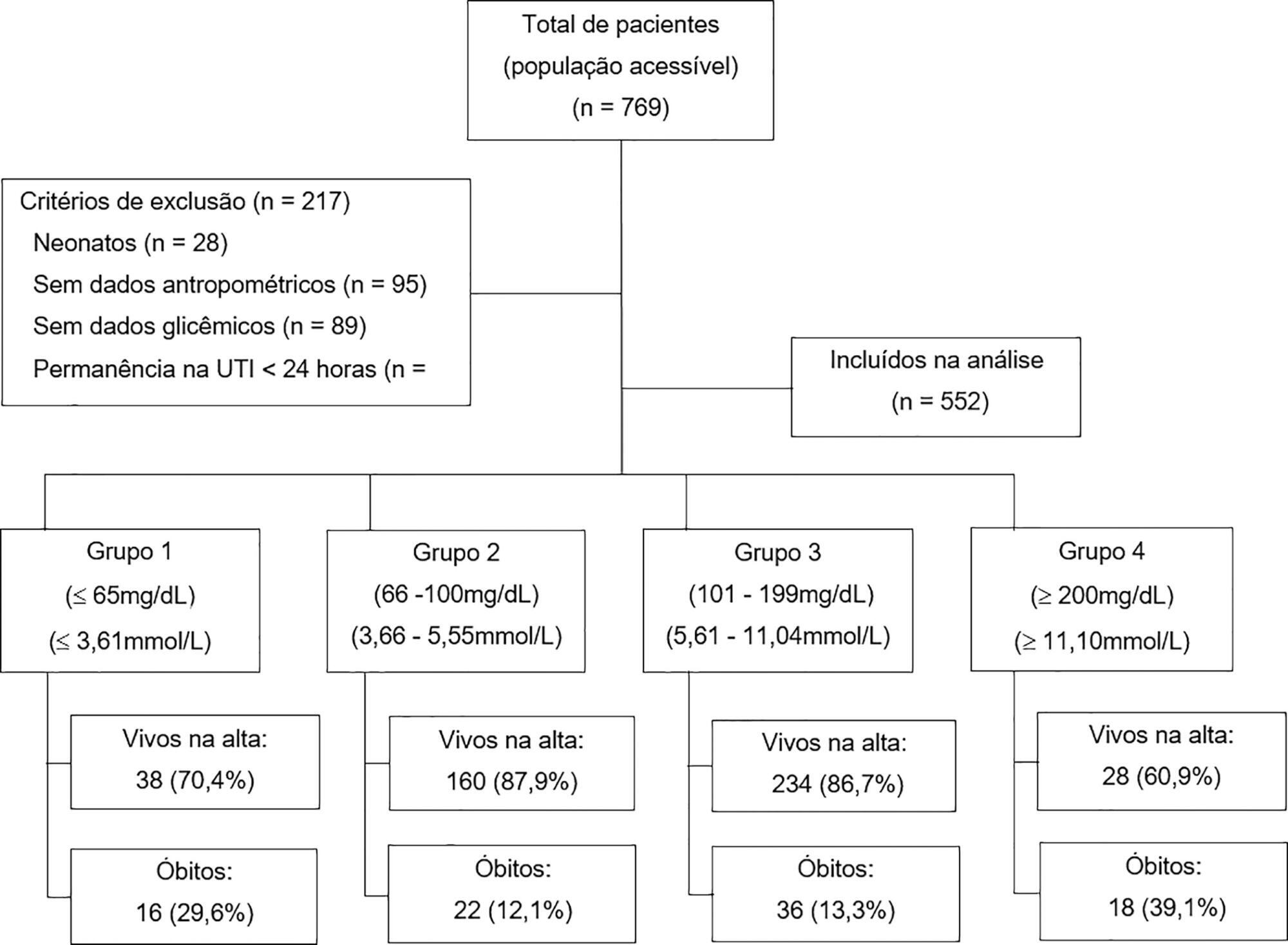
A retrospective cohort of pediatric intensive care unit patients admitted to the Instituto Nacional de Salud del Niño between 2012 and 2013. A Poisson regression model with robust variance was used to quantify the association. Diagnostic test performance evaluation was used to describe the sensitivity, specificity, positive predictive value, negative predictive value and likelihood ratios for each range of glycemia.
In total, 552 patients were included (median age 23 months, age range 5 months to 79.8 months). The mean glycemia level upon admission was 121.3mg/dL (6.73mmol/L). Ninety-two (16.6%) patients died during hospitalization. In multivariable analyses, significant associations were found between glycemia < 65mg/dL (3.61mmol/L) (RR: 2.01, 95%CI 1.14 - 3.53), glycemia > 200mg/dL (> 11.1mmol/L) (RR: 2.91, 95%CI 1.71 - 4.55), malnutrition (RR: 1.53, 95%CI 1.04 - 2.25), mechanical ventilation (RR: 3.71, 95%CI 1.17 - 11.76) and mortality at discharge. There was low sensitivity (between 17.39% and 39.13%) and high specificity (between 49.13% and 91.74%) for different glucose cut-off levels.
There was an increased risk of death at discharge in patients who developed hypoglycemia and hyperglycemia upon admission to the pediatric intensive care unit. Certain glucose ranges (> 200mg/dL (> 11.1mmol/L) and < 65mg/dL (3.61mmol/L)) have high specificity as predictors of death at discharge.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):364-372
DOI 10.5935/0103-507X.20170054
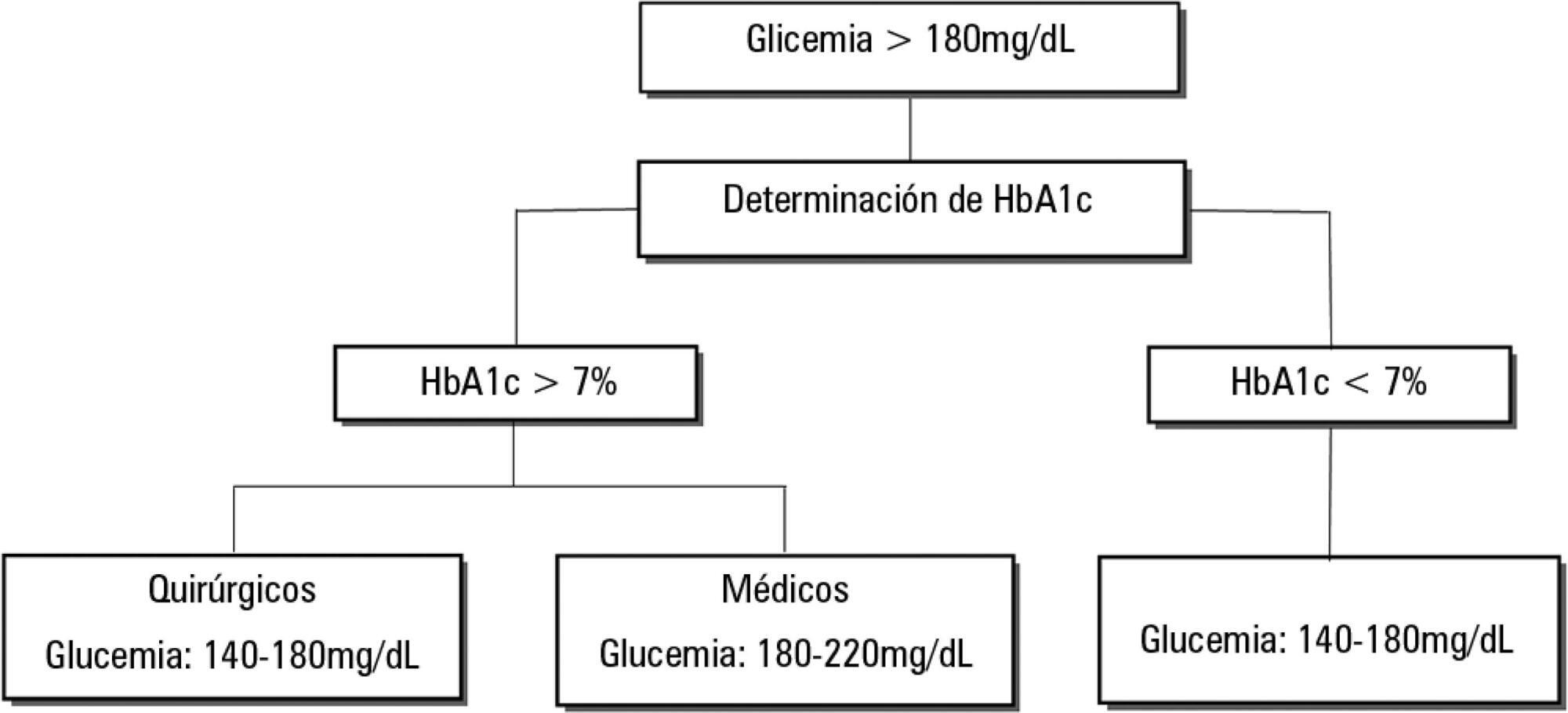
Dysglycemia in critically ill patients (hyperglycemia, hypoglycemia, glycemic variability and time in range) is a biomarker of disease severity and is associated with higher mortality. However, this impact appears to be weakened in patients with previous diabetes mellitus, particularly in those with poor premorbid glycemic control; this phenomenon has been called "diabetes paradox". This phenomenon determines that glycated hemoglobin (HbA1c) values should be considered in choosing glycemic control protocols on admission to an intensive care unit and that patients' target blood glucose ranges should be adjusted according to their HbA1c values. Therefore, HbA1c emerges as a simple tool that allows information that has therapeutic utility and prognostic value to be obtained in the intensive care unit.