Abstract
Rev Bras Ter Intensiva. 2019;31(3):361-367
DOI 10.5935/0103-507X.20190059
To compare the impact of two fast-track strategies regarding the extubation time and removal of invasive mechanical ventilation in adults after cardiac surgery on clinical and hospital outcomes.
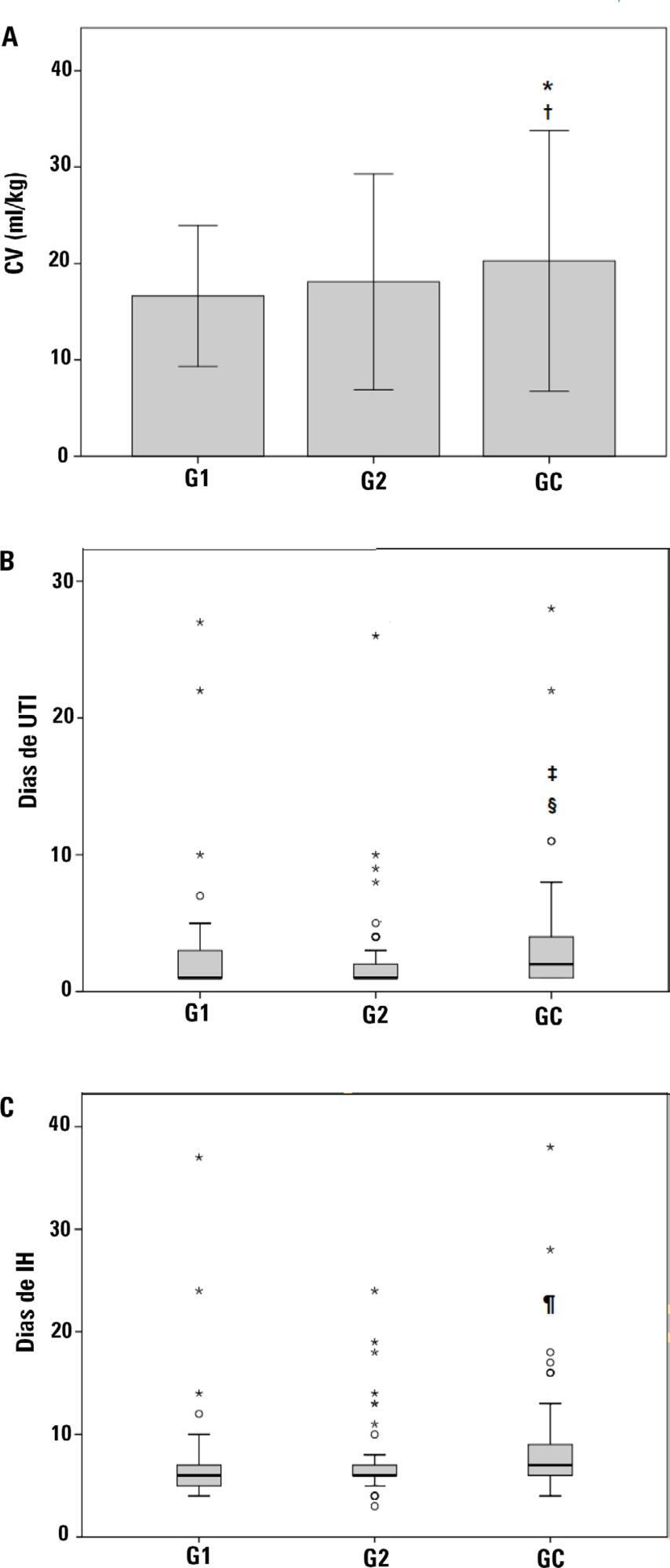
This was a retrospective cohort study with patients undergoing cardiac surgery. Patients were classified according to the extubation time as the Control Group (extubated 6 hours after admission to the intensive care unit, with a maximum mechanical ventilation time of 18 hours), Group 1 (extubated in the operating room after surgery) and Group 2 (extubated within 6 hours after admission to the intensive care unit). The primary outcomes analyzed were vital capacity on the first postoperative day, length of hospital stay, and length of stay in the intensive care unit. The secondary outcomes were reintubation, hospital-acquired pneumonia, sepsis, and death.
For the 223 patients evaluated, the vital capacity was lower in Groups 1 and 2 compared to the Control (p = 0.000 and p = 0.046, respectively). The length of stay in the intensive care unit was significantly lower in Groups 1 and 2 compared to the Control (p = 0.009 and p = 0.000, respectively), whereas the length of hospital stay was lower in Group 1 compared to the Control (p = 0.014). There was an association between extubation in the operating room (Group 1) with reintubation (p = 0.025) and postoperative complications (p = 0.038).
Patients undergoing fast-track management with extubation within 6 hours had shorter stays in the intensive care unit without increasing postoperative complications and death. Patients extubated in the operating room had a shorter hospital stay and a shorter stay in the intensive care unit but showed an increase in the frequency of reintubation and postoperative complications.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):79-85
DOI 10.5935/0103-507X.20190012
We aimed to determine the incidence, risk factors, and outcomes of unplanned extubation among adult patients.
We conducted a prospective cohort study of adult intubated patients admitted to the charity wards of a government tertiary teaching hospital in the Philippines. Patients managed in both intensive care and nonintensive care settings were included. Patients were followed-up until discharge or until seven days postextubation.
The outcomes of the 191 included patients were planned extubation (35%), unplanned extubation (19%), death (39%), and discharge against advice (7%). Competing risk regression showed that male sex (Crude OR: 2.25, 95%CI: 1.10 - 4.63) and age (Crude OR 0.976, 95%CI: 0.957 - 0.996) were significant baseline factors. The night shift (Crude OR: 24.6, 95%CI: 2.87 - 211) was also consistently associated with more unplanned extubations. Among postextubation outcomes, reintubation (unplanned extubation: 61.1% versus planned extubation: 25.4%), acute respiratory failure (unplanned extubation: 38.9% versus planned extubation: 17.5%), and cardiovascular events (unplanned extubation: 8.33% versus planned extubation: 1.49%) occurred significantly more often among the unplanned extubation patients. Admission in an intensive care unit was not associated with a lower risk of unplanned extubation (Crude OR 1.15, 95%CI: 0.594 - 2.21).
Many intubated patients had unplanned extubation. Patients admitted in nonintensive care unit settings did not have significantly higher odds of unplanned extubation.
Abstract
Rev Bras Ter Intensiva. 2018;30(3):294-300
DOI 10.5935/0103-507X.20180046
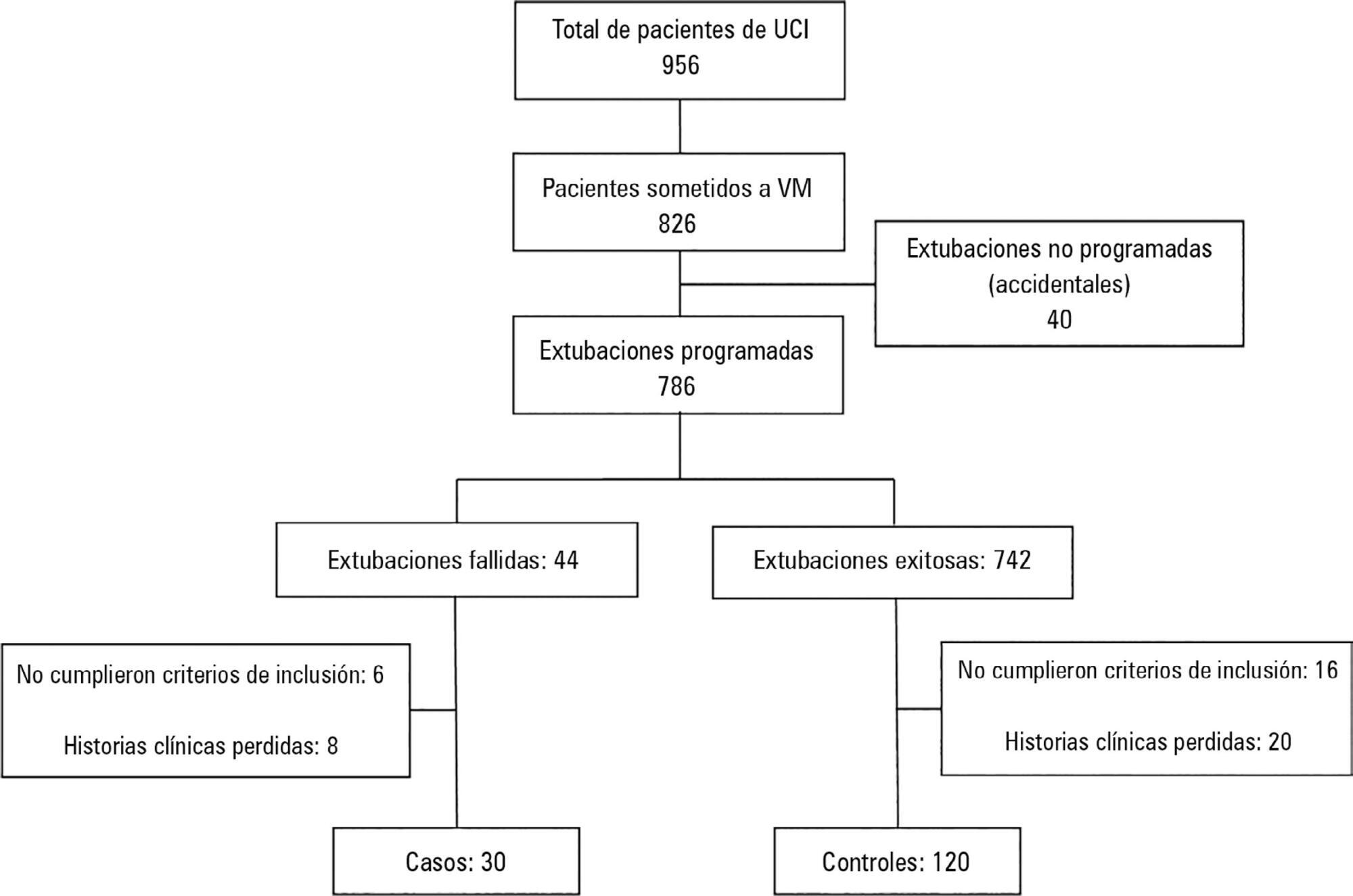
To determine the risk factors for extubation failure in the intensive care unit.
The present case-control study was conducted in an intensive care unit. Failed extubations were used as cases, while successful extubations were used as controls. Extubation failure was defined as reintubation being required within the first 48 hours of extubation.
Out of a total of 956 patients who were admitted to the intensive care unit, 826 were subjected to mechanical ventilation (86%). There were 30 failed extubations and 120 successful extubations. The proportion of failed extubations was 5.32%. The risk factors found for failed extubations were a prolonged length of mechanical ventilation of greater than 7 days (OR = 3.84, 95%CI = 1.01 - 14.56, p = 0.04), time in the intensive care unit (OR = 1.04, 95%CI = 1.00 - 1.09, p = 0.03) and the use of sedatives for longer than 5 days (OR = 4.81, 95%CI = 1.28 - 18.02; p = 0.02).
Pediatric patients on mechanical ventilation were at greater risk of failed extubation if they spent more time in the intensive care unit and if they were subjected to prolonged mechanical ventilation (longer than 7 days) or greater amounts of sedative use.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):252-259
DOI 10.5935/0103-507X.20150046
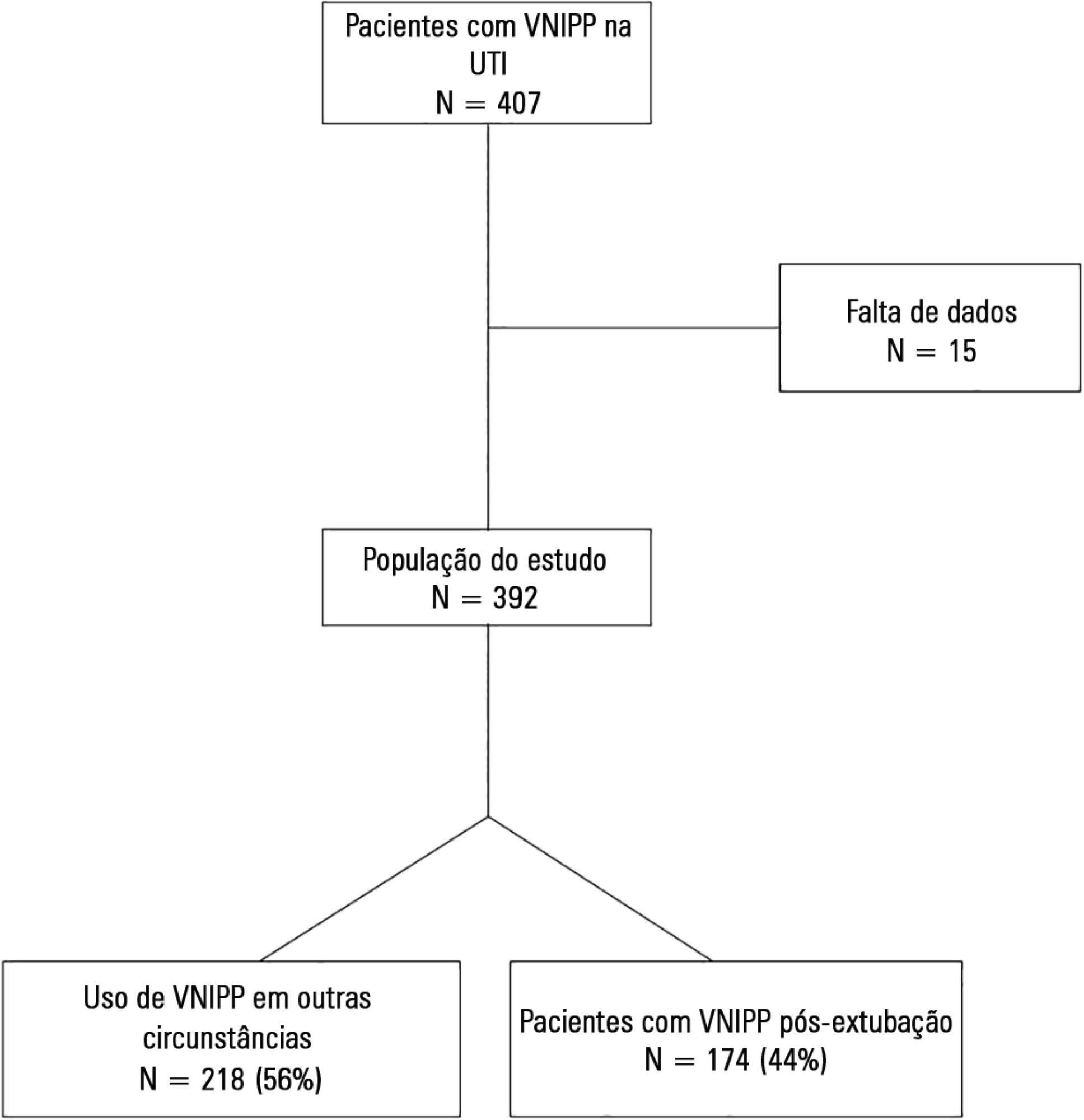
To describe postextubation noninvasive positive pressure ventilation use in intensive care unit clinical practice and to identify factors associated with noninvasive positive pressure ventilation failure.
This prospective cohort study included patients aged ≥ 18 years consecutively admitted to the intensive care unit who required noninvasive positive pressure ventilation within 48 hours of extubation. The primary outcome was noninvasive positive pressure ventilation failure.
We included 174 patients in the study. The overall noninvasive positive pressure ventilation use rate was 15%. Among the patients who used noninvasive positive pressure ventilation, 44% used it after extubation. The failure rate of noninvasive positive pressure ventilation was 34%. The overall mean ± SD age was 56 ± 18 years, and 55% of participants were male. Demographics; baseline pH, PaCO2 and HCO3; and type of equipment used were similar between groups. All of the noninvasive positive pressure ventilation final parameters were higher in the noninvasive positive pressure ventilation failure group [inspiratory positive airway pressure: 15.0 versus 13.7cmH2O (p = 0.015), expiratory positive airway pressure: 10.0 versus 8.9cmH2O (p = 0.027), and FiO2: 41 versus 33% (p = 0.014)]. The mean intensive care unit length of stay was longer (24 versus 13 days), p < 0.001, and the intensive care unit mortality rate was higher (55 versus 10%), p < 0.001 in the noninvasive positive pressure ventilation failure group. After fitting, the logistic regression model allowed us to state that patients with inspiratory positive airway pressure ≥ 13.5cmH2O on the last day of noninvasive positive pressure ventilation support are three times more likely to experience noninvasive positive pressure ventilation failure compared with individuals with inspiratory positive airway pressure < 13.5 (OR = 3.02, 95%CI = 1.01 - 10.52, p value = 0.040).
The noninvasive positive pressure ventilation failure group had a longer intensive care unit length of stay and a higher mortality rate. Logistic regression analysis identified that patients with inspiratory positive airway pressure ≥ 13.5cmH2O on the last day of noninvasive positive pressure ventilation support are three times more likely to experience noninvasive positive pressure ventilation failure.
Abstract
Rev Bras Ter Intensiva. 2012;24(3):230-235
DOI 10.1590/S0103-507X2012000300005
OBJECTIVE: This study established the incidence and primary causes of unplanned extubation in newborns in the neonatal intensive care units of the Hospital Sofia Feldman, Belo Horizonte (Minas Gerais). METHODS: This retrospective study was conducted between July 1, 2009 and April 30, 2010. Unplanned extubations and their primary causes were assessed using an adverse events form. The following variables were assessed: gender, corrected age, present weight, duration of mechanical ventilation time, and motives/causes of the event on the day of the unplanned extubation event. RESULTS: Fifty-four unplanned extubations occurred, which corresponded to an incidence of 1.0 event/100 days of mechanical ventilation. This rate was higher among newborns with a corrected age of 30 to 36 weeks and weight < 1,000 g. The primary causes of unplanned extubations included patient agitation, inappropriate handling of patients during the performance of procedures, and inappropriate fixation and positioning of the endotracheal tube. CONCLUSION: The incidence of unplanned extubation in the investigated neonatal intensive care units was low during the study period compared to previously reported data. Nevertheless, the assessment of the quality of procedures, the continuous follow-up of newborns, and the monitoring of the causes of extubation are required to further reduce this incidence.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (115) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)