You searched for:"Carolina Fu"
We found (5) results for your search.-
Original Article
Factors associated with functional decline in an intensive care unit: a prospective study on the level of physical activity and clinical factors
Rev Bras Ter Intensiva. 2021;33(4):565-571
Abstract
Original ArticleFactors associated with functional decline in an intensive care unit: a prospective study on the level of physical activity and clinical factors
Rev Bras Ter Intensiva. 2021;33(4):565-571
DOI 10.5935/0103-507X.20210073
Views1See moreABSTRACT
Objective:
To identify the factors associated with functional status decline in intensive care unit patients.
Methods:
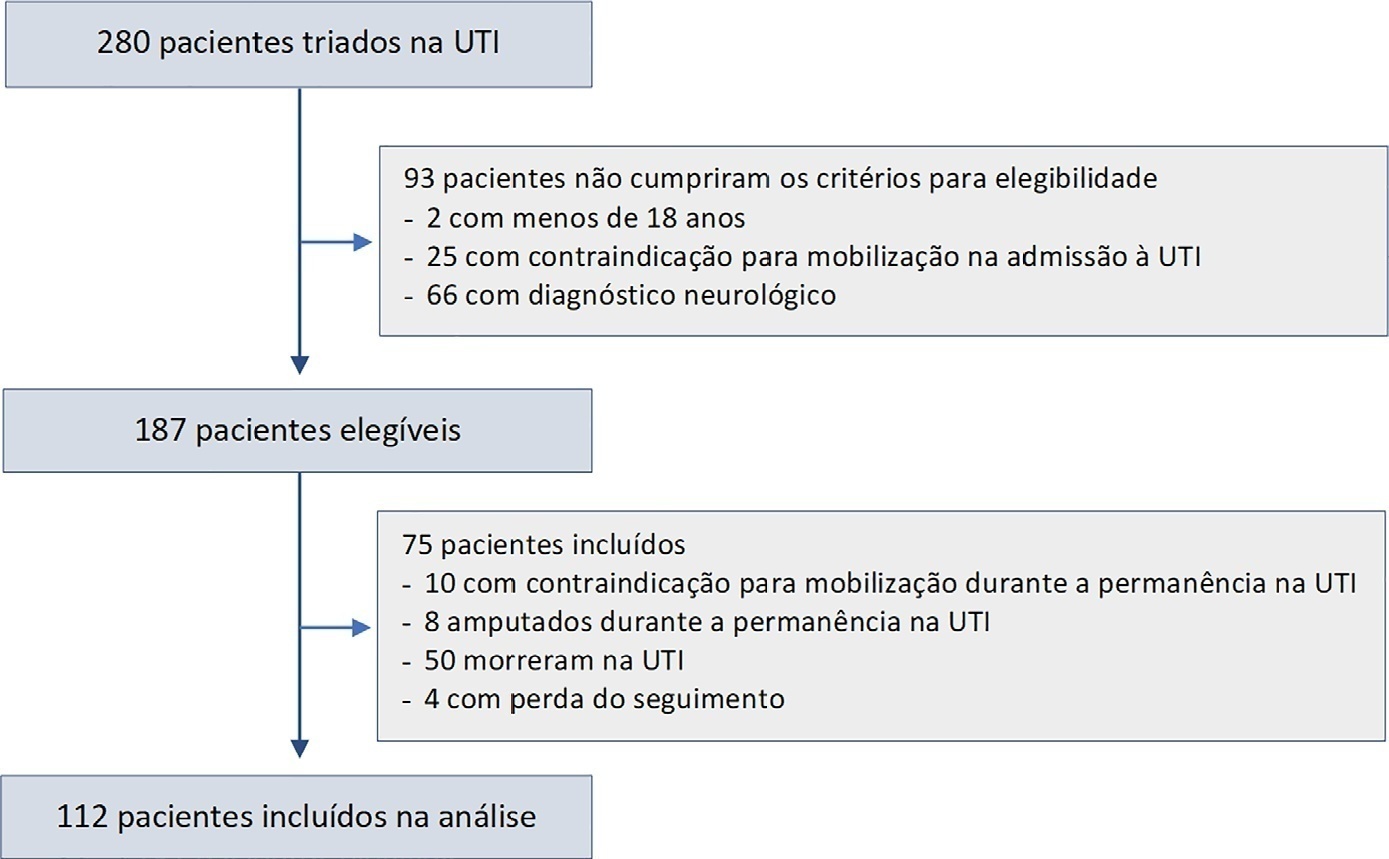
In this prospective study, patients in an intensive care unit aged 18 years or older without neurological disease or contraindications to mobilization were included. The exclusion criteria were patients who spent fewer than 4 days in the intensive care unit or died during the study period. Accelerometry was used to assess the physical activity level of patients. We recorded age, SAPS 3, days on mechanical ventilation, drugs used, comorbidities, and functional status after intensive care unit discharge. After intensive care unit discharge, the patients were assigned to a dependent group or an independent group according to their Barthel index. Logistic regression and the odds ratio were used in the analyses.
Results:
Sixty-three out of 112 included patients were assigned to the dependent group. The median Charlson comorbidity index was 3 (2 – 4). The mean SAPS 3 score was 53 ± 11. The patients spent 94 ± 4% of the time spent in inactivity and 4.8 ± 3.7% in light activities. The odds ratio showed that age (OR = 1.08; 95%CI 1.04 – 1.13) and time spent in inactivity (OR = 1.38; 95%CI 1.14 – 1.67) were factors associated with functional status decline. Time spent in light activity was associated with a better functional status (OR = 0.73; 95%CI 0.60 – 0.89).
Conclusions:
Age and time spent in inactivity during intensive care unit stay are associated with functional status decline. On the other hand, performing light activities seems to preserve the functional status of patients.
-
Original Articles
Rehabilitation through virtual reality: physical activity of patients admitted to the intensive care unit
Rev Bras Ter Intensiva. 2019;31(4):456-463
Abstract
Original ArticlesRehabilitation through virtual reality: physical activity of patients admitted to the intensive care unit
Rev Bras Ter Intensiva. 2019;31(4):456-463
DOI 10.5935/0103-507X.20190078
Views1See moreABSTRACT
Objective:
To evaluate the level of activity that Nintendo WiiTM can elicit in intensive care unit patients and its associated safety and patient satisfaction.
Methods:
Experimental, single-center study performed at a tertiary care hospital. Patients ≥ 18 years old who were admitted to the intensive care unit, participated in videogames as part of their physical therapy sessions and did not have mobility restrictions were included. Th exclusion criteria were the inability to comprehend instructions and the inability to follow simple commands. We included n = 60 patients and performed 100 sessions. We used the Nintendo WiiTM gaming system in the sessions. An accelerometer measured the level of physical activity of patients while they played videogames. We evaluated the level of activity, the modified Borg scale scores, the adverse events and the responses to a questionnaire on satisfaction with the activity.
Results:
One hundred physical therapy sessions were analyzed. When the patients played the videogame, they reached a light level of activity for 59% of the session duration and a moderate level of activity for 38% of the session duration. No adverse events occurred. A total of 86% of the patients reported that they would like to play the videogame in their future physical therapy sessions.
Conclusion:
Virtual rehabilitation elicited light to moderate levels of activity in intensive care unit patients. This therapy is a safe tool and is likely to be chosen by the patient during physical therapy.

-
Original Articles
Noninvasive positive pressure ventilation after extubation: features and outcomes in clinical practice
Rev Bras Ter Intensiva. 2015;27(3):252-259
Abstract
Original ArticlesNoninvasive positive pressure ventilation after extubation: features and outcomes in clinical practice
Rev Bras Ter Intensiva. 2015;27(3):252-259
DOI 10.5935/0103-507X.20150046
Views0ABSTRACT
Objective:
To describe postextubation noninvasive positive pressure ventilation use in intensive care unit clinical practice and to identify factors associated with noninvasive positive pressure ventilation failure.
Methods:
This prospective cohort study included patients aged ≥ 18 years consecutively admitted to the intensive care unit who required noninvasive positive pressure ventilation within 48 hours of extubation. The primary outcome was noninvasive positive pressure ventilation failure.
Results:
We included 174 patients in the study. The overall noninvasive positive pressure ventilation use rate was 15%. Among the patients who used noninvasive positive pressure ventilation, 44% used it after extubation. The failure rate of noninvasive positive pressure ventilation was 34%. The overall mean ± SD age was 56 ± 18 years, and 55% of participants were male. Demographics; baseline pH, PaCO2 and HCO3; and type of equipment used were similar between groups. All of the noninvasive positive pressure ventilation final parameters were higher in the noninvasive positive pressure ventilation failure group [inspiratory positive airway pressure: 15.0 versus 13.7cmH2O (p = 0.015), expiratory positive airway pressure: 10.0 versus 8.9cmH2O (p = 0.027), and FiO2: 41 versus 33% (p = 0.014)]. The mean intensive care unit length of stay was longer (24 versus 13 days), p < 0.001, and the intensive care unit mortality rate was higher (55 versus 10%), p < 0.001 in the noninvasive positive pressure ventilation failure group. After fitting, the logistic regression model allowed us to state that patients with inspiratory positive airway pressure ≥ 13.5cmH2O on the last day of noninvasive positive pressure ventilation support are three times more likely to experience noninvasive positive pressure ventilation failure compared with individuals with inspiratory positive airway pressure < 13.5 (OR = 3.02, 95%CI = 1.01 - 10.52, p value = 0.040).
Conclusion:
The noninvasive positive pressure ventilation failure group had a longer intensive care unit length of stay and a higher mortality rate. Logistic regression analysis identified that patients with inspiratory positive airway pressure ≥ 13.5cmH2O on the last day of noninvasive positive pressure ventilation support are three times more likely to experience noninvasive positive pressure ventilation failure.
Keywords:Airway extubationIntensive care unitsPositive-pressure respiration/methodsRespiration, artificialTreatment outcomesVentilator weaningSee more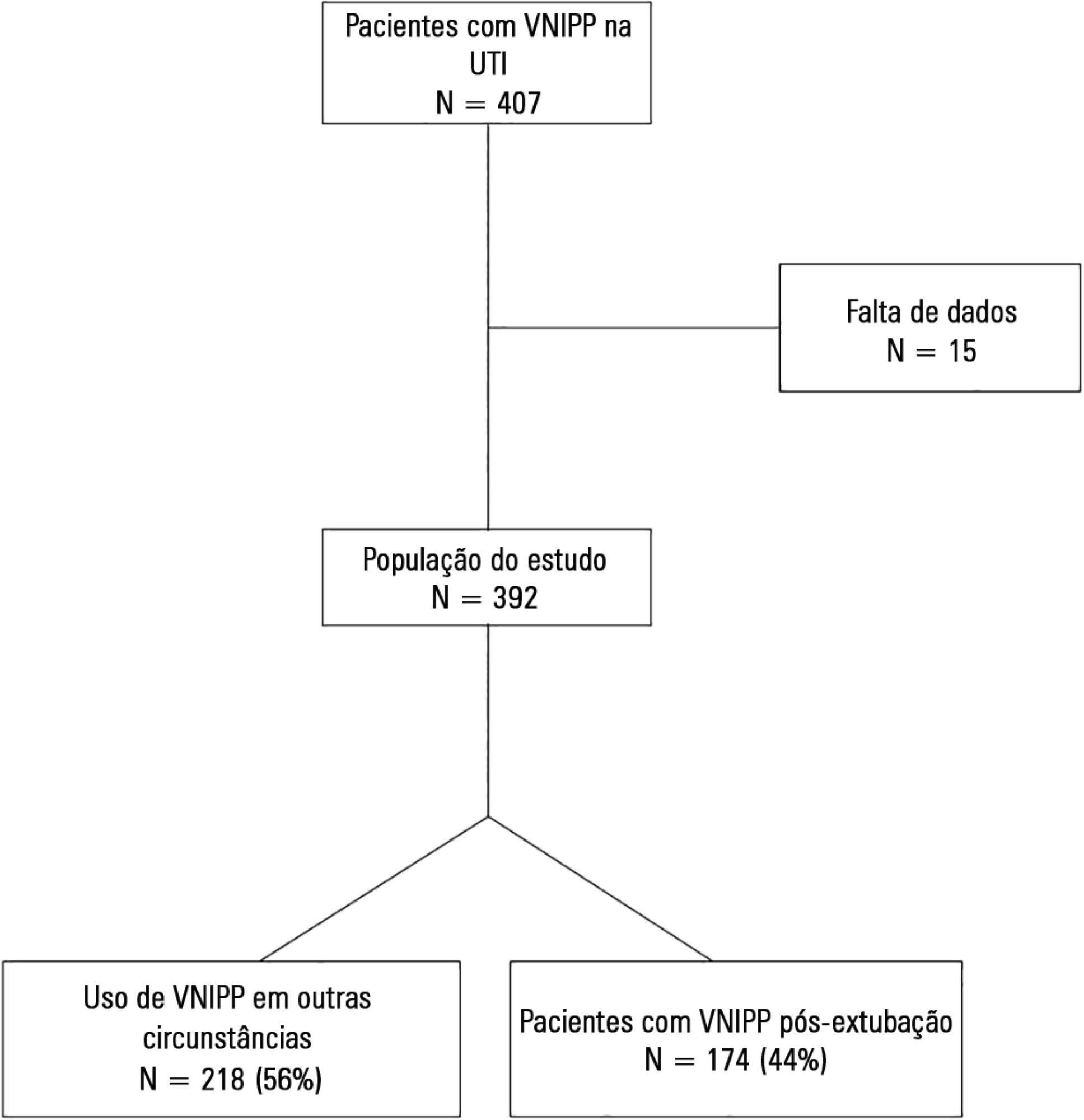
-
Original Articles – Clinical Research
Characterization of the use of a cycle ergometer to assist in the physical therapy treatment of critically ill patients
Rev Bras Ter Intensiva. 2013;25(1):39-43
Abstract
Original Articles – Clinical ResearchCharacterization of the use of a cycle ergometer to assist in the physical therapy treatment of critically ill patients
Rev Bras Ter Intensiva. 2013;25(1):39-43
DOI 10.1590/S0103-507X2013000100008
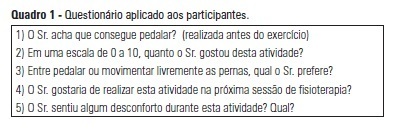
Views0See moreOBJECTIVE: The objective of this study was to use a cycle ergometer to assess cardiorespiratory changes during active exercise and to verify patients’ satisfaction with this type of activity. METHODS: A single intervention involving active lower limb exercise was performed with a cycle ergometer (without load) for 5 minutes. The following variables were measured before, during and immediately after exercise: heart rate, blood pressure, respiratory rate, peripheral oxygen saturation and the Borg dyspnea scale score. Following the exercise, the patients answered a questionnaire to evaluate their satisfaction with this type of activity. RESULTS: A total of 38 patients (65% male) with a mean age of 48 ± 16 years old participated in the study. Enrolled patients presented a sequential organ failure assessment (SOFA) score of 2 (0 – 5 scale). During the exercise, 16% of the patients used ventilation support and 55% of them were breathing at room air. A comparison of the initial and final values of the variables indicated increases in the heart rate (92±17 beats/min vs. 95±18 beats/min; p<0.05), the respiratory rate (19 ± 8 breaths/min vs. 23±8 breaths/min; p<0.05) and the Borg dyspnea scale score (1.3±1.8 vs. 2.8±2.2; p<0.05). In addition, 85% of the patients reported enjoying the activity. Only 25% of the patients reported some discomfort, and 100% of the patients wanted to repeat this type of activity in future treatments. CONCLUSION: During the cycle ergometer exercises, minor cardiorespiratory changes were observed in the patients. The evaluated patients reported high satisfaction with this type of activity.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




