Abstract
Rev Bras Ter Intensiva. 2021;33(2):188-195
DOI 10.5935/0103-507X.20210026
To describe the usual practice of mobility therapy in the adult intensive care unit for patients with and without COVID-19.
Online survey in which physical therapists working in an adult intensive care unit in Argentina participated. Sixteen multiple-choice or single-response questions grouped into three sections were asked. The first section addressed personal, professional and work environment data. The second section presented questions regarding usual care, and the third focused on practices under COVID-19 pandemic conditions.
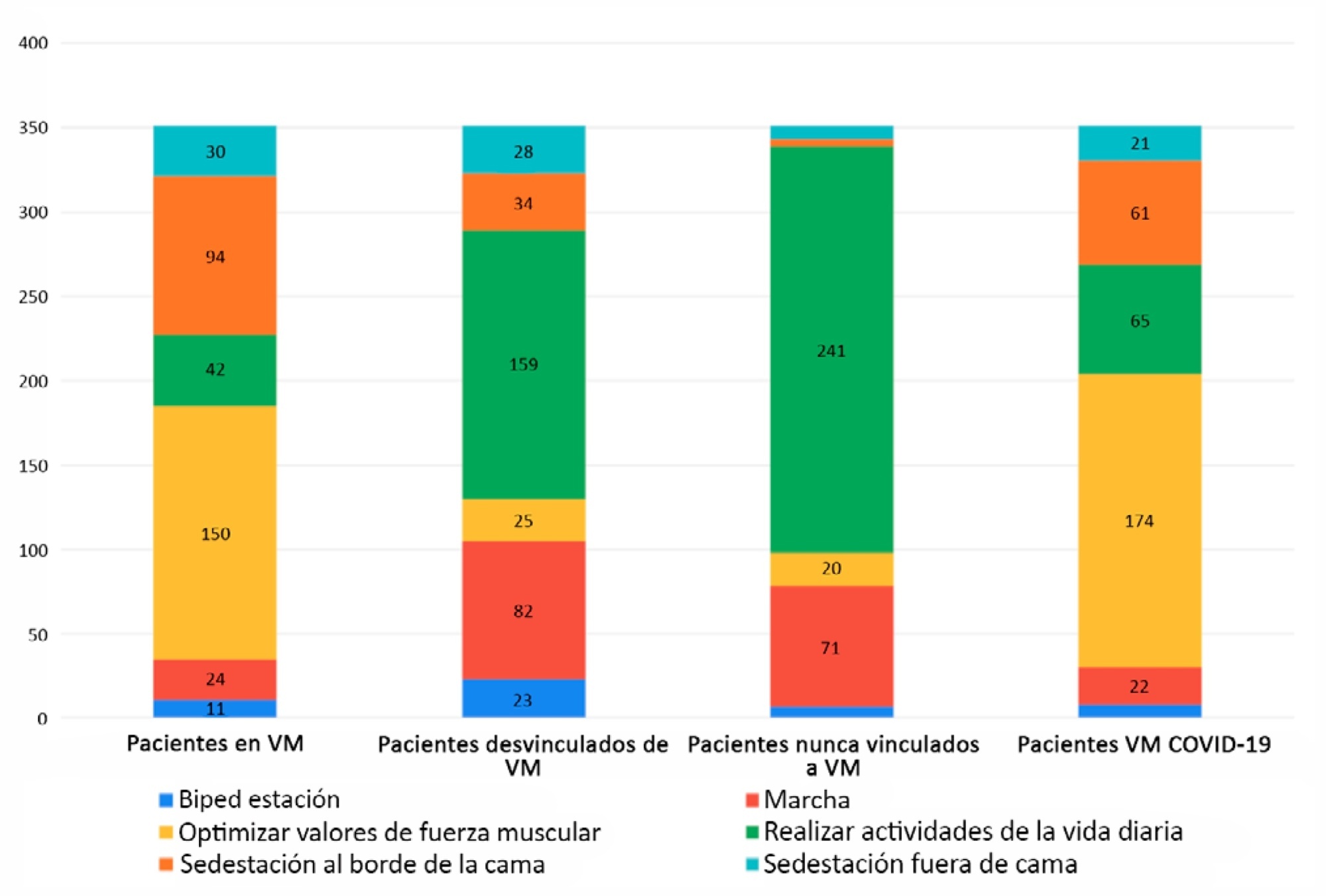
Of 351 physical therapists, 76.1% answer that they were exclusively responsible for patient mobility. The highest motor-based goal varied according to four patient scenarios: Mechanically ventilated patients, patients weaned from mechanical ventilation, patients who had never required mechanical ventilation, and patients with COVID-19 under mechanical ventilation. In the first and last scenarios, the highest goal was to optimize muscle strength, while for the other two, it was to perform activities of daily living. Finally, the greatest limitation in working with patients with COVID-19 was respiratory and/or contact isolation.
Physical therapists in Argentina reported being responsible for the mobility of patients in the intensive care unit. The highest motor-based therapeutic goals for four classic scenarios in the closed area were limited by the need for mechanical ventilation. The greatest limitation when mobilizing patients with COVID-19 was respiratory and contact isolation.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):248-257
DOI 10.5935/0103-507X.20190038
To describe the existing early mobilization protocols in pediatric intensive care units.
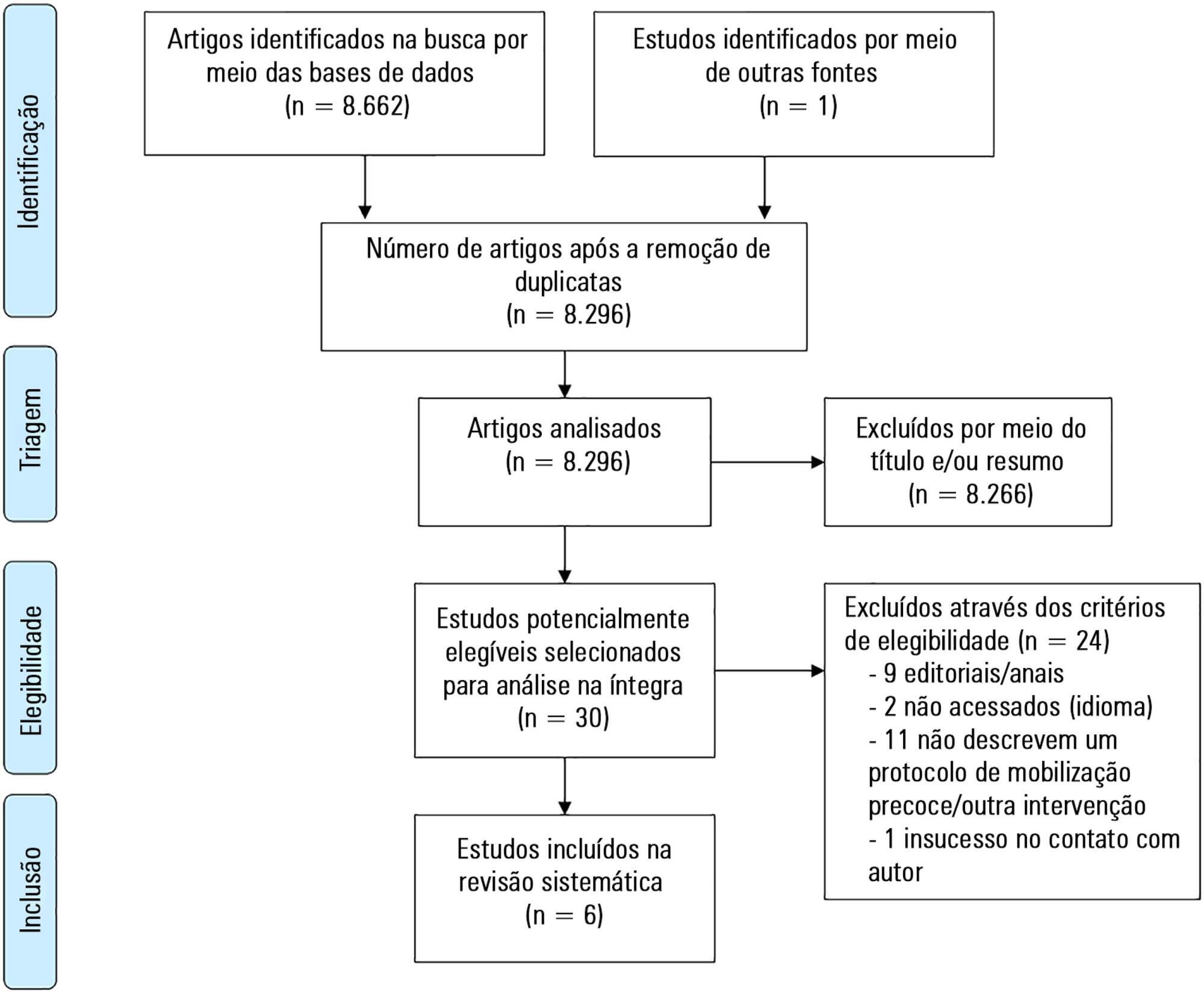
A systematic literature review was performed using the databases MEDLINE®, Embase, SciELO, LILACS and PeDRO, without restrictions of date and language. Observational and randomized and nonrandomized clinical trials that described an early mobilization program in patients aged between 29 days and 18 years admitted to the pediatric intensive care unit were included. The methodological quality of the studies was evaluated using the Newcastle-Ottawa Scale, Methodological Index for Non-Randomized Studies and the Cochrane Collaboration.
A total of 8,663 studies were identified, of which 6 were included in this review. Three studies described the implementation of an early mobilization program, including activities such as progressive passive mobilization, positioning, and discussion of mobilization goals with the team, in addition to contraindications and interruption criteria. Cycle ergometer and virtual reality games were also used as resources for mobilization. Four studies considered the importance of the participation of the multidisciplinary team in the implementation of early mobilization protocols.
In general, early mobilization protocols are based on individualized interventions, depending on the child's development. In addition, the use of a cycle ergometer may be feasible and safe in this population. The implementation of institutional and multidisciplinary protocols may contribute to the use of early mobilization in pediatric intensive care units; however, studies demonstrating the efficacy of such intervention are needed.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):39-43
DOI 10.1590/S0103-507X2013000100008
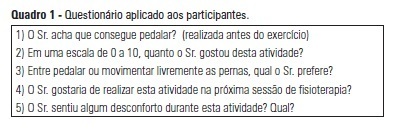
OBJECTIVE: The objective of this study was to use a cycle ergometer to assess cardiorespiratory changes during active exercise and to verify patients' satisfaction with this type of activity. METHODS: A single intervention involving active lower limb exercise was performed with a cycle ergometer (without load) for 5 minutes. The following variables were measured before, during and immediately after exercise: heart rate, blood pressure, respiratory rate, peripheral oxygen saturation and the Borg dyspnea scale score. Following the exercise, the patients answered a questionnaire to evaluate their satisfaction with this type of activity. RESULTS: A total of 38 patients (65% male) with a mean age of 48 ± 16 years old participated in the study. Enrolled patients presented a sequential organ failure assessment (SOFA) score of 2 (0 - 5 scale). During the exercise, 16% of the patients used ventilation support and 55% of them were breathing at room air. A comparison of the initial and final values of the variables indicated increases in the heart rate (92±17 beats/min vs. 95±18 beats/min; p<0.05), the respiratory rate (19 ± 8 breaths/min vs. 23±8 breaths/min; p<0.05) and the Borg dyspnea scale score (1.3±1.8 vs. 2.8±2.2; p<0.05). In addition, 85% of the patients reported enjoying the activity. Only 25% of the patients reported some discomfort, and 100% of the patients wanted to repeat this type of activity in future treatments. CONCLUSION: During the cycle ergometer exercises, minor cardiorespiratory changes were observed in the patients. The evaluated patients reported high satisfaction with this type of activity.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)