You searched for:"Renata Salatti Ferrari"
We found (3) results for your search.-
Original Article
Functional deficit in children with congenital heart disease undergoing surgical correction after intensive care unit discharge
Rev Bras Ter Intensiva. 2020;32(2):261-267
Abstract
Original ArticleFunctional deficit in children with congenital heart disease undergoing surgical correction after intensive care unit discharge
Rev Bras Ter Intensiva. 2020;32(2):261-267
DOI 10.5935/0103-507X.20200042
Views0See moreAbstract
Objective:
To evaluate the functional status of pediatric patients undergoing congenital heart surgery after discharge from the intensive care unit, and to evaluate the correlations among clinical variables, functional status and surgical risk.
Methods:
Cross-sectional study including patients aged 1 month to less than 18 years undergoing congenital heart surgery between October 2017 and May 2018. Functional outcome was assessed by the Functional Status Scale, surgical risk classification was determined using the Risk Adjustment for Congenital Heart Surgery-1 (RACHS-1), and clinical variables were collected from electronic medical records.
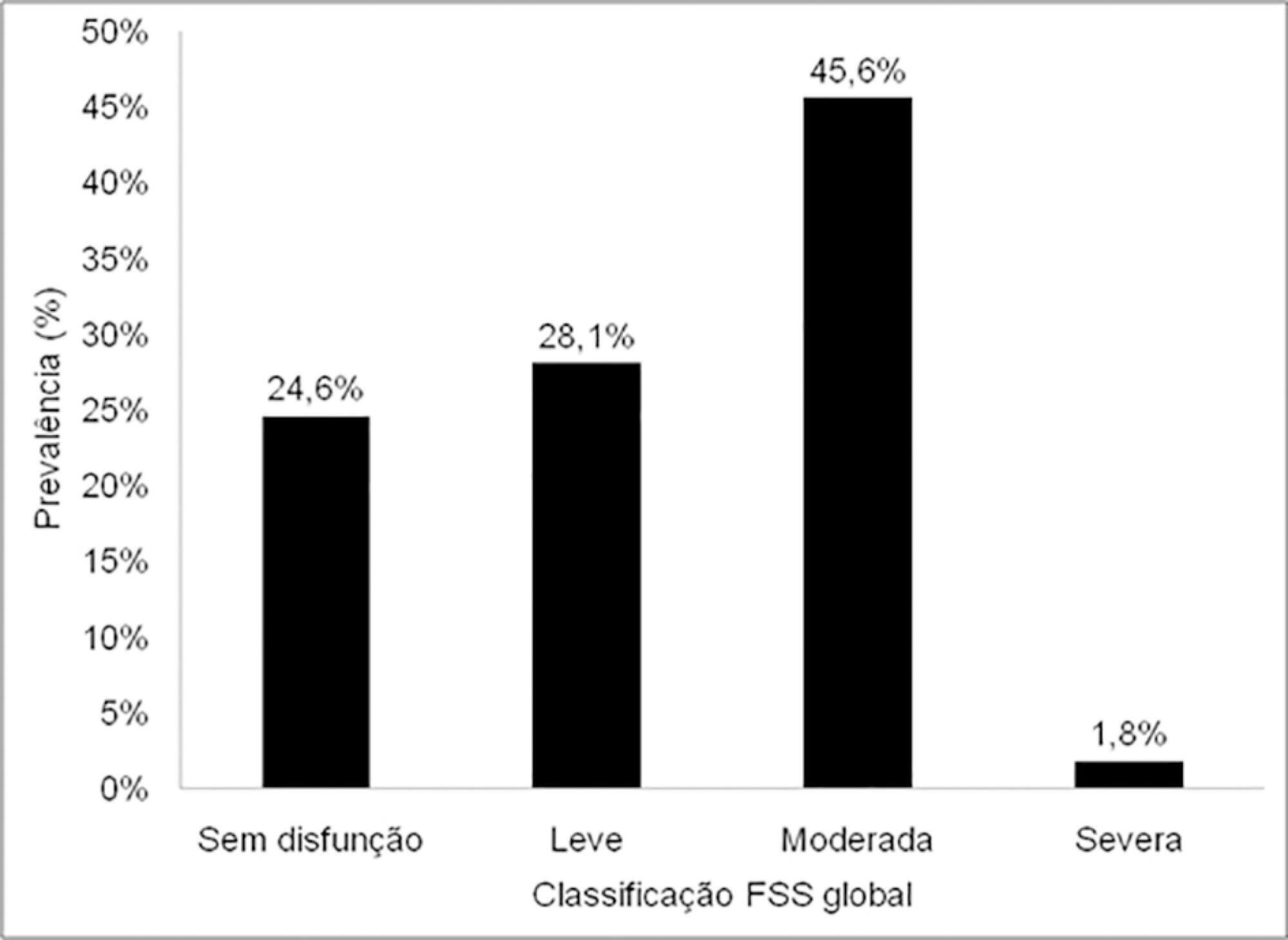
Results:
The sample comprised 57 patients with a median age of 7 months (2 – 17); 54.4% were male, and 75.5% showed dysfunction, which was moderate in 45.6% of the cases. RACHS-1 category > 3 was observed in 47% of the sample, indicating higher surgical risk. There was a correlation between functional deficit and younger age, longer duration of invasive mechanical ventilation and longer intensive care unit stay. Moreover, greater functional deficit was observed among patients classified as RACHS-1 category > 3.
Conclusion:
The prevalence of functional deficit was high among children and adolescents with congenital heart disease after cardiac surgery. Higher surgical risk, longer duration of invasive mechanical ventilation, longer intensive care unit stay and younger age were correlated with worse functional status.
-
Review Article
Early mobilization protocols for critically ill pediatric patients: systematic review
Rev Bras Ter Intensiva. 2019;31(2):248-257
Abstract
Review ArticleEarly mobilization protocols for critically ill pediatric patients: systematic review
Rev Bras Ter Intensiva. 2019;31(2):248-257
DOI 10.5935/0103-507X.20190038
Views0See moreABSTRACT
Objective:
To describe the existing early mobilization protocols in pediatric intensive care units.
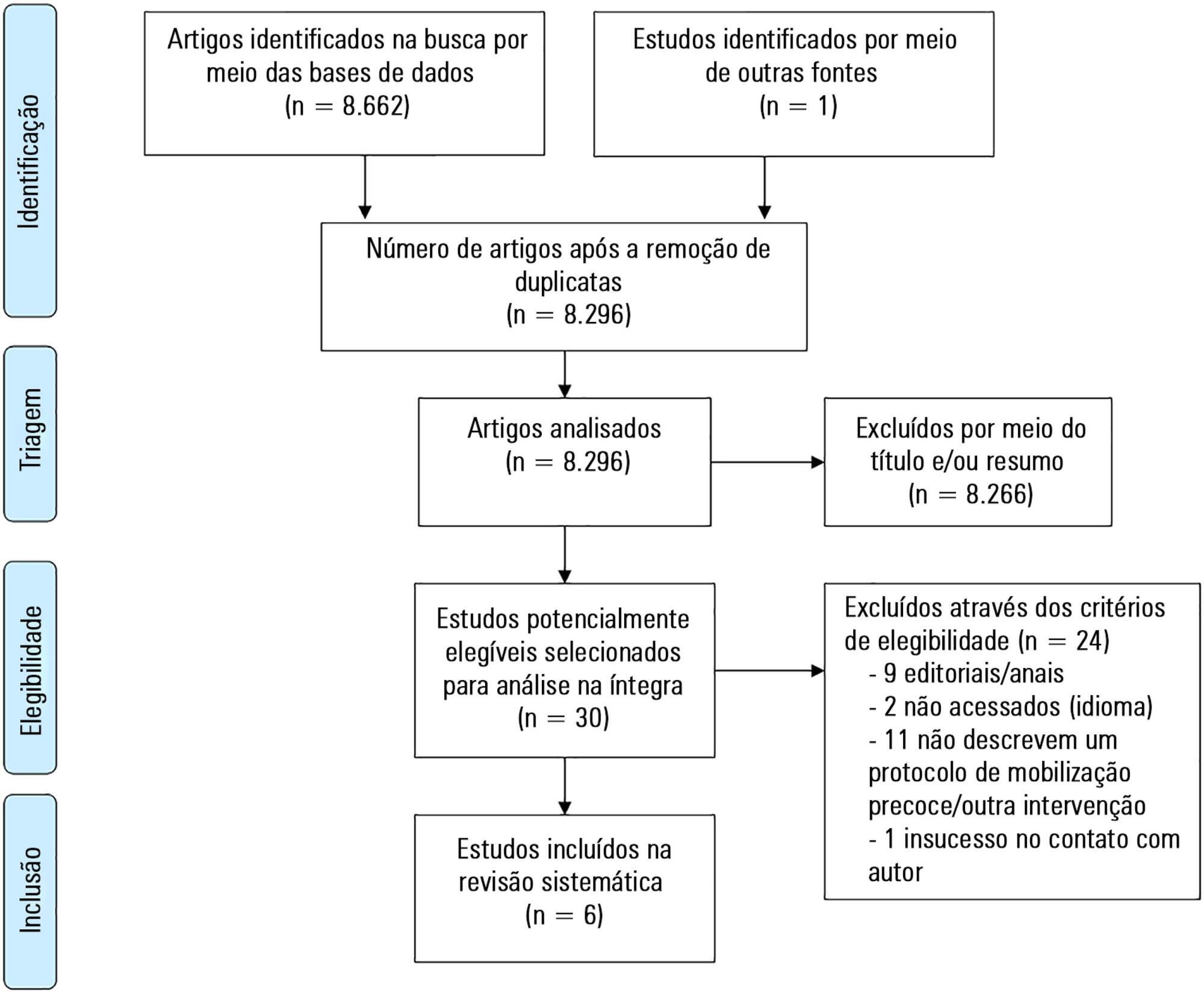
Methods:
A systematic literature review was performed using the databases MEDLINE®, Embase, SciELO, LILACS and PeDRO, without restrictions of date and language. Observational and randomized and nonrandomized clinical trials that described an early mobilization program in patients aged between 29 days and 18 years admitted to the pediatric intensive care unit were included. The methodological quality of the studies was evaluated using the Newcastle-Ottawa Scale, Methodological Index for Non-Randomized Studies and the Cochrane Collaboration.
Results:
A total of 8,663 studies were identified, of which 6 were included in this review. Three studies described the implementation of an early mobilization program, including activities such as progressive passive mobilization, positioning, and discussion of mobilization goals with the team, in addition to contraindications and interruption criteria. Cycle ergometer and virtual reality games were also used as resources for mobilization. Four studies considered the importance of the participation of the multidisciplinary team in the implementation of early mobilization protocols.
Conclusion:
In general, early mobilization protocols are based on individualized interventions, depending on the child’s development. In addition, the use of a cycle ergometer may be feasible and safe in this population. The implementation of institutional and multidisciplinary protocols may contribute to the use of early mobilization in pediatric intensive care units; however, studies demonstrating the efficacy of such intervention are needed.
-
Original Articles
Functional evaluation of pediatric patients after discharge from the intensive care unit using the Functional Status Scale
Rev Bras Ter Intensiva. 2017;29(4):460-465
Abstract
Original ArticlesFunctional evaluation of pediatric patients after discharge from the intensive care unit using the Functional Status Scale
Rev Bras Ter Intensiva. 2017;29(4):460-465
DOI 10.5935/0103-507X.20170066
Views0See moreABSTRACT
Objective:
To evaluate the functional status of pediatric patients after discharge from the pediatric intensive care unit using the Functional Status Scale and to compare the time of invasive mechanical ventilation, length of stay in the pediatric intensive care unit, and Pediatric Index of Mortality 2 results among individuals with different degrees of functional impairment.
Methods:
A cross-sectional study was conducted on patients who were discharged from a pediatric intensive care unit. The functional evaluation by the Functional Status Scale was performed on the first day after discharge from the unit, and the Pediatric Index of Mortality 2 was used to predict the mortality rate at the time of admission to the pediatric intensive care unit.
Results:
The sample consisted of 50 individuals, 60% of which were male, with a median age of 19 [6 – 61] months. The overall score of the Functional Status Scale was 11.5 [7 – 15], and the highest scores were observed in the “motor function” 3 [1 – 4] and “feeding” 4 [1 – 4] domains. Compared to patients who were not readmitted to the pediatric intensive care unit, patients who were readmitted presented a worse overall score (p = 0.01), worse scores in the “motor function” (p = 0.01), “feeding” (p = 0.02), and “respiratory” (p = 0.036) domains, and a higher mortality rate according to the Pediatric Index of Mortality 2 (p = 0.025).
Conclusion:
Evaluation of the functional status using the Functional Status Scale indicated moderate impairment in patients after discharge from the pediatric intensive care unit, mainly in the “motor function” and “feeding” domains; patients who were readmitted to the pediatric intensive care unit demonstrated worse overall functional, motor function, feeding and respiratory scores. Individuals with greater functional impairment had longer times of invasive mechanical ventilation and hospitalization in the pediatric intensive care unit.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




