Abstract
Rev Bras Ter Intensiva. 2018;30(2):208-218
DOI 10.5935/0103-507X.20180038
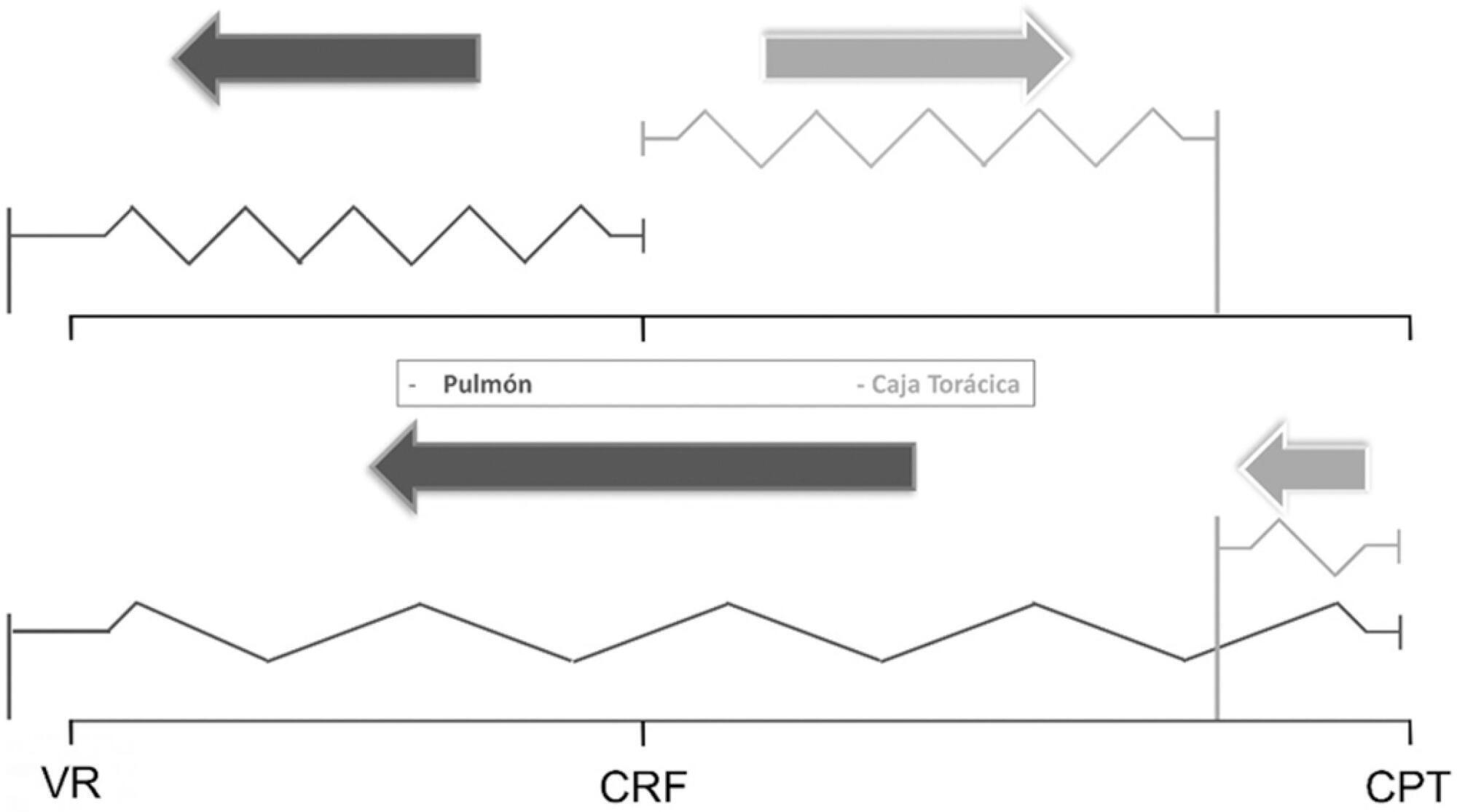
The respiratory system mechanics depend on the characteristics of the lung and chest wall and their interaction. In patients with acute respiratory distress syndrome under mechanical ventilation, the monitoring of airway plateau pressure is fundamental given its prognostic value and its capacity to assess pulmonary stress. However, its validity can be affected by changes in mechanical characteristics of the chest wall, and it provides no data to correctly titrate positive end-expiratory pressure by restoring lung volume. The chest wall effect on respiratory mechanics in acute respiratory distress syndrome has not been completely described, and it has likely been overestimated, which may lead to erroneous decision making. The load imposed by the chest wall is negligible when the respiratory system is insufflated with positive end-expiratory pressure. Under dynamic conditions, moving this structure demands a pressure change whose magnitude is related to its mechanical characteristics, and this load remains constant regardless of the volume from which it is insufflated. Thus, changes in airway pressure reflect changes in the lung mechanical conditions. Advanced monitoring could be reserved for patients with increased intra-abdominal pressure in whom a protective mechanical ventilation strategy cannot be implemented. The estimates of alveolar recruitment based on respiratory system mechanics could reflect differences in chest wall response to insufflation and not actual alveolar recruitment.
Abstract
Rev Bras Ter Intensiva. 2015;27(4):406-411
DOI 10.5935/0103-507X.20150068
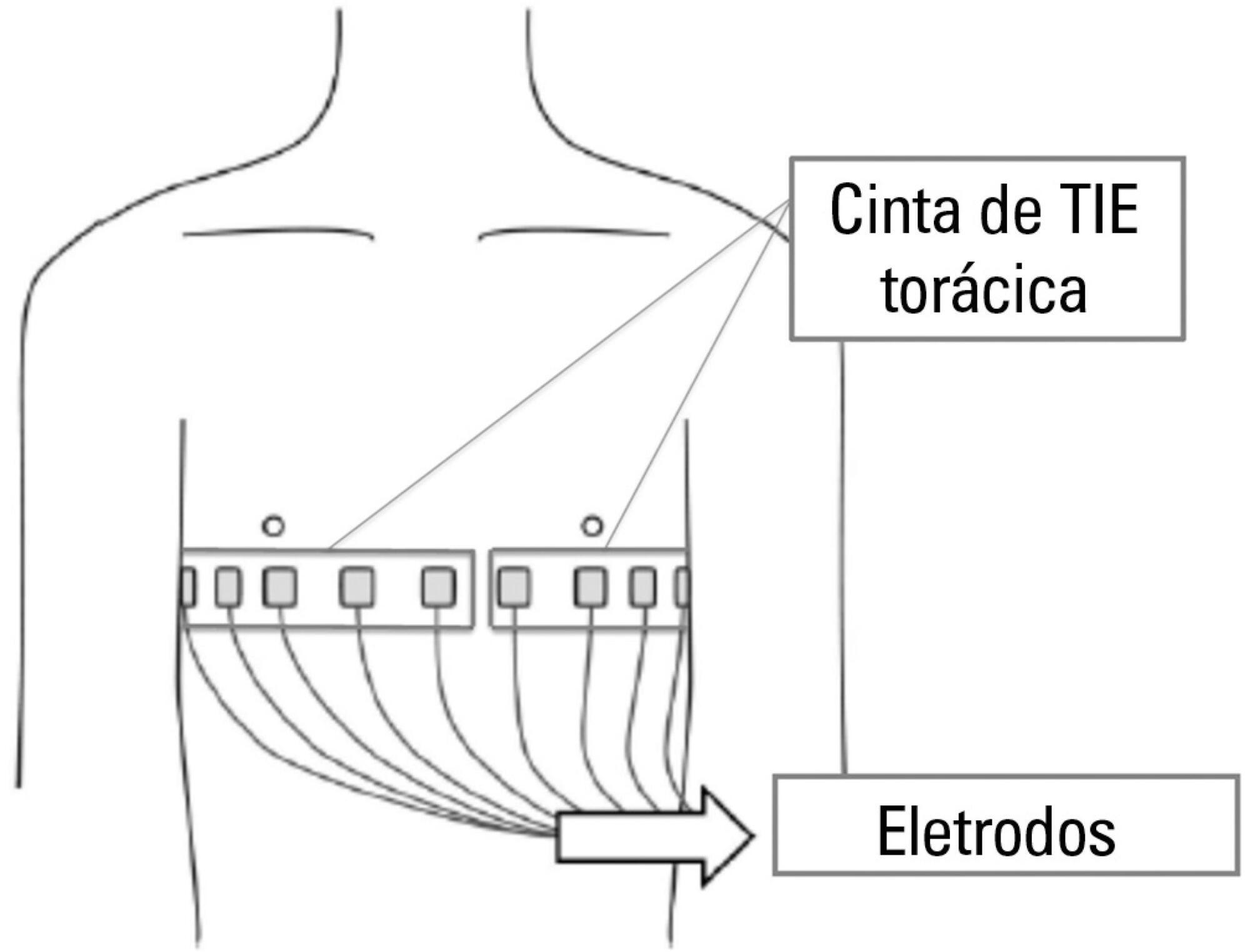
Thoracic electrical impedance tomography is a real-time, noninvasive monitoring tool of the regional pulmonary ventilation distribution. Its bedside use in patients with acute respiratory distress syndrome has the potential to aid in alveolar recruitment maneuvers, which are often necessary in cases of refractory hypoxemia. In this case report, we describe the monitoring results and interpretation of thoracic electrical impedance tomography used during alveolar recruitment maneuvers in a patient with acute respiratory distress syndrome, with transient application of high alveolar pressures and optimal positive end-expiratory pressure titration. Furthermore, we provide a brief literature review regarding the use of alveolar recruitment maneuvers and monitoring using thoracic electrical impedance tomography in patients with acute respiratory distress syndrome.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):155-160
DOI 10.5935/0103-507X.20150027
To evaluate the changes in ventilatory mechanics and hemodynamics that occur in patients dependent on mechanical ventilation who are subjected to a standard respiratory therapy protocol.
This experimental and prospective study was performed in two intensive care units, in which patients dependent on mechanical ventilation for more than 48 hours were consecutively enrolled and subjected to an established respiratory physiotherapy protocol. Ventilatory variables (dynamic lung compliance, respiratory system resistance, tidal volume, peak inspiratory pressure, respiratory rate, and oxygen saturation) and hemodynamic variables (heart rate) were measured one hour before (T-1), immediately after (T0) and one hour after (T+1) applying the respiratory physiotherapy protocol.
During the period of data collection, 104 patients were included in the study. Regarding the ventilatory variables, an increase in dynamic lung compliance (T-1 = 52.3 ± 16.1mL/cmH2O versus T0 = 65.1 ± 19.1mL/cmH2O; p < 0.001), tidal volume (T-1 = 550 ± 134mL versus T0 = 698 ± 155mL; p < 0.001), and peripheral oxygen saturation (T-1 = 96.5 ± 2.29% versus T0 = 98.2 ± 1.62%; p < 0.001) were observed, in addition to a reduction of respiratory system resistance (T-1 = 14.2 ± 4.63cmH2O/L/s versus T0 = 11.0 ± 3.43cmH2O/L/s; p < 0.001), after applying the respiratory physiotherapy protocol. All changes were present in the assessment performed one hour (T+1) after the application of the respiratory physiotherapy protocol. Regarding the hemodynamic variables, an immediate increase in the heart rate after application of the protocol was observed, but that increase was not maintained (T-1 = 88.9 ± 18.7 bpm versus T0 = 93.7 ± 19.2bpm versus T+1 = 88.5 ± 17.1bpm; p < 0.001).
Respiratory therapy leads to immediate changes in the lung mechanics and hemodynamics of mechanical ventilation-dependent patients, and ventilatory changes are likely to remain for at least one hour.
Abstract
Rev Bras Ter Intensiva. 2015;27(4):347-352
DOI 10.5935/0103-507X.20150059
The positioning of a patient in bed may directly affect their respiratory mechanics. The objective of this study was to evaluate the respiratory mechanics of mechanically ventilated patients positioned with different head angles hospitalized in an intensive care unit.
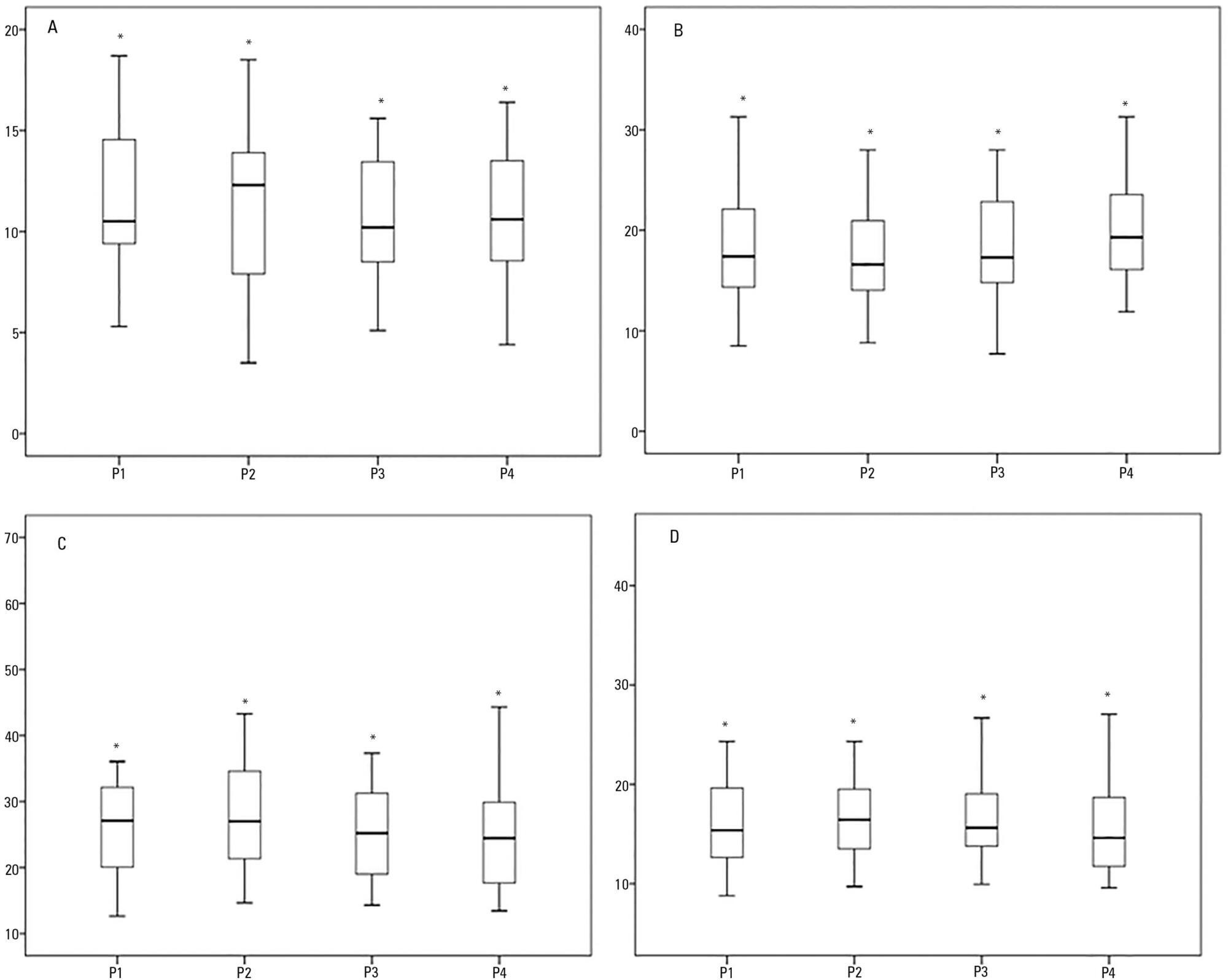
This was a prospective physiological study in which static and dynamic compliance, resistive airway pressure, and peripheral oxygen saturation were measured with the head at four different positions (0° = P1, 30° = P2, 45° = P3, and 60° = P4). Repeated-measures analysis of variance (ANOVA) with a Bonferroni post-test and Friedman analysis were used to compare the values obtained at the different positions.
A comparison of the 35 evaluated patients revealed that the resistive airway pressure values in the 0° position were higher than those obtained when patients were positioned at greater angles. The elastic pressure analysis revealed that the 60° position produced the highest value relative to the other positions. Regarding static compliance, a reduction in values was observed from the 0° position to the 60° position. The dynamic compliance analysis revealed that the 30° angle produced the greatest value compared to the other positions. The peripheral oxygen saturation showed little variation, with the highest value obtained at the 0° position.
The highest dynamic compliance value was observed at the 30° position, and the highest oxygenation value was observed at the 0° position.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):163-168
DOI 10.5935/0103-507X.20140024
To compare the effectiveness of the alveolar recruitment maneuver and the breath stacking technique with respect to lung mechanics and gas exchange in patients with acute lung injury.
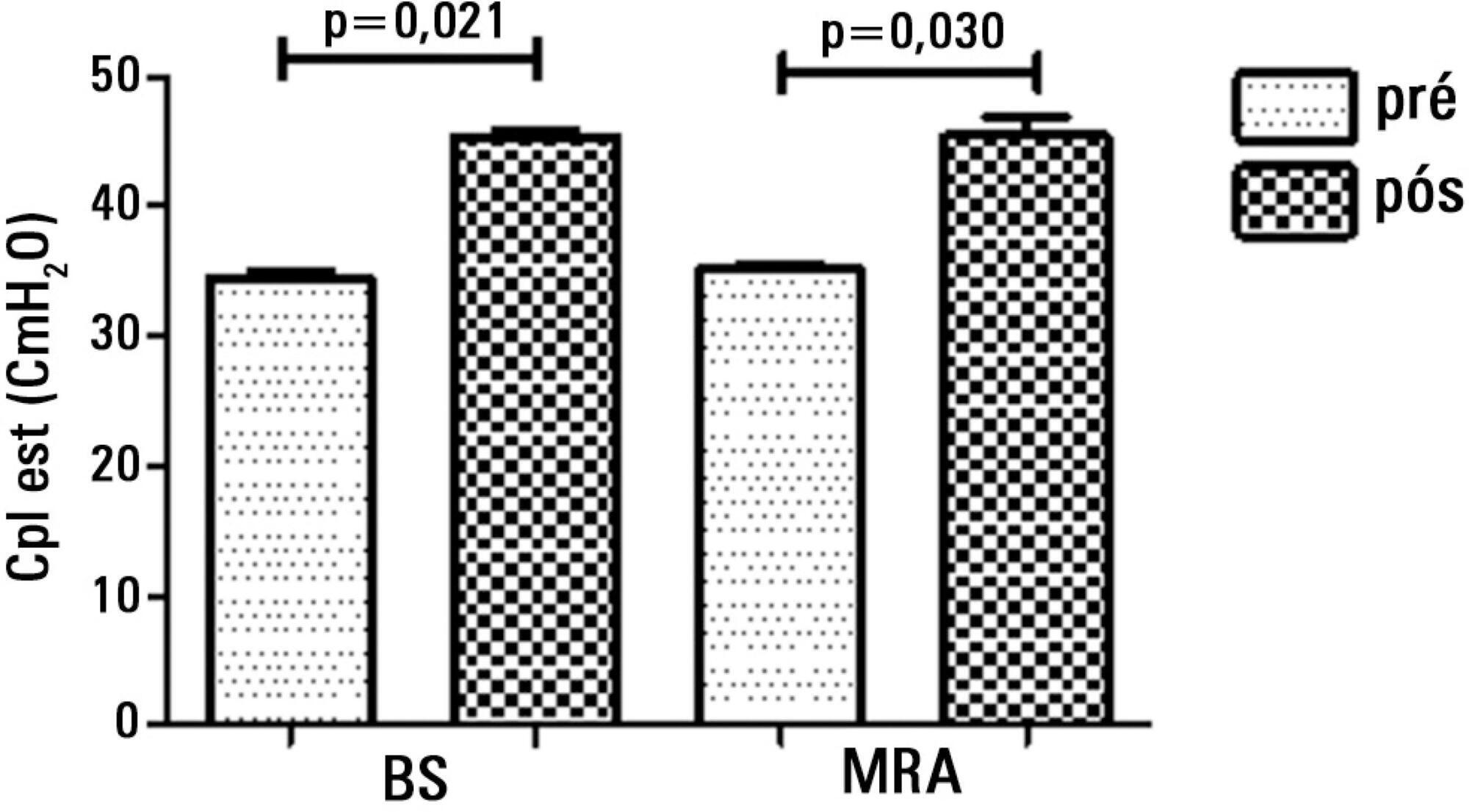
Thirty patients were distributed into two groups: Group 1 - breath stacking; and Group 2 - alveolar recruitment maneuver. After undergoing conventional physical therapy, all patients received both treatments with an interval of 1 day between them. In the first group, the breath stacking technique was used initially, and subsequently, the alveolar recruitment maneuver was applied. Group 2 patients were initially subjected to alveolar recruitment, followed by the breath stacking technique. Measurements of lung compliance and airway resistance were evaluated before and after the use of both techniques. Gas analyses were collected before and after the techniques were used to evaluate oxygenation and gas exchange.
Both groups had a significant increase in static compliance after breath stacking (p=0.021) and alveolar recruitment (p=0.03), but with no significant differences between the groups (p=0.95). The dynamic compliance did not increase for the breath stacking (p=0.22) and alveolar recruitment (p=0.074) groups, with no significant difference between the groups (p=0.11). The airway resistance did not decrease for either groups, i.e., breath stacking (p=0.91) and alveolar recruitment (p=0.82), with no significant difference between the groups (p=0.39). The partial pressure of oxygen increased significantly after breath stacking (p=0.013) and alveolar recruitment (p=0.04), but there was no significant difference between the groups (p=0.073). The alveolar-arterial O2 difference decreased for both groups after the breath stacking (p=0.025) and alveolar recruitment (p=0.03) interventions, and there was no significant difference between the groups (p=0.81).
Our data suggest that the breath stacking and alveolar recruitment techniques are effective in improving the lung mechanics and gas exchange in patients with acute lung injury.
Abstract
Rev Bras Ter Intensiva. 2013;25(4):312-318
DOI 10.5935/0103-507X.20130053
The development of abdominal surgery represents an alternative therapy for the morbidly obese; however, patients undergoing this surgical procedure often experience postoperative pulmonary complications. The use of alveolar recruitment maneuvers and/or perioperative ventilatory strategies is a possible alternative to reduce these complications, focusing on the reduction of postoperative pulmonary complications. In this review, the benefits of perioperative ventilatory strategies and the implementation of alveolar recruitment maneuvers in obese patients undergoing abdominal surgery are described.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):453-460
DOI 10.1590/S0103-507X2009000400017
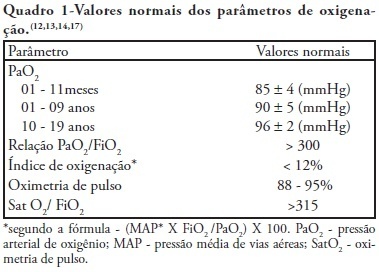
Recent changes were introduced in acute hypoxemic respiratory failure children ventilation methods. There are evidences that less aggressive ventilation strategies can improve severe pulmonary injury survival. Experimental trials evidenced a relationship between inappropriate ventilatory measures and delayed acute pulmonary injury improvement, or even worsening. From this, a protective ventilatory measure arises in combination with alveolar recruitment maneuver. This association is believed in clinical practice to determine importantly reduced morbidity and mortality as well as reduced mechanic ventilation-induced injuries. It is indicated for acute lung injury patients, generally from pneumonia or sepsis, with severe hypoxemia. Its main contraindications are homodynamic instability, pneumothorax and intracranial hypertension. Experimental trials showed beneficial maneuver effects on both oxygenation and alveolar collapse. Adult studies showed improved pulmonary function with hypoxemia reversion. In children, the maneuver lead to significant inspired oxygen fraction and alveolar collapse reductions, less oxygen dependency, improved pulmonary complacency, and reduced bronchopulmonary dysplasia. However, studies in children are limited. Additional investigation is warranted on this matter, and its clinical application evidence. A literature review was conducted based on textbooks and MEDLINE, Pubmed, Cochrane library, SciELO, and Ovid databases, from 1998 to 2009, both in Portuguese and English. Publications on alveolar recruitment maneuver both in adults and children, review articles, experimental and clinical trials were included using the key words: protective ventilatory strategy, alveolar recruitment maneuver, pediatrics and mechanic ventilation.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):292-298
DOI 10.1590/S0103-507X2009000300009
BACKGROUND AND OBJECTIVES: An inspired oxygen fraction (FiO2) of 40% is often used for weaning patients, but lower FiO2 values are also recommended, if arterial oxygen pressure (PaO2)/ FiO2 >150-200 mmHg. This study aimed to compare respiratory variables and vital data values recorded during use of sufficient FiO2 (ideal) to maintain peripheral oxygen saturation at 92% with values recorded during use of FiO2 established at 40% (baseline) in weaning patients. METHODS: Prospective cross-over study. Respiratory variables (respiratory frequency, tidal volume, occlusion pressure, inspiratory time/total time ratio) and vital data (blood pressure and heart rate) were collected sequentially at 30 and 60 minutes with baseline FiO2, followed by ideal FiO2. These were compared to a generalized linear model for repeated measurements. Comparisons between baseline and ideal FiO2 values, and arterial blood gases were evaluated by the Student's t or Wilcoxon tests. RESULTS: In 30 adult patients the median of ideal FiO2 was 25% (IQ25%-75% 23-28). This was significantly lower than baseline FiO2 (40%) (p< 0.001). No significant difference was found in the PaO2/ FiO2 ratio between baseline FiO2 (269±53) and ideal FiO2 (268±47). Tidal volume was significantly lower during use of ideal FiO2 (p=0.003) and blood pressure was significantly higher during use of baseline FiO2 (p=0.041), but there was no clinical significance. The remaining variables were not affected by reduction in FiO2. The ideal FiO2 did not influence remaining variables. CONCLUSIONS: These results suggest that FiO2 levels sufficient to ensure a SpO2>92% did not alter breathing patterns or trigger clinical changes in weaning patients.