You searched for:"Renata Rego Lins Fumis"
We found (6) results for your search.-
Original Article
Clinical outcomes and lung mechanics characteristics between COVID-19 and non-COVID-19-associated acute respiratory distress syndrome: a propensity score analysis of two major randomized trials
Rev Bras Ter Intensiva. 2022;34(3):335-341
Abstract
Original ArticleClinical outcomes and lung mechanics characteristics between COVID-19 and non-COVID-19-associated acute respiratory distress syndrome: a propensity score analysis of two major randomized trials
Rev Bras Ter Intensiva. 2022;34(3):335-341
DOI 10.5935/0103-507X.20220040-en
Views3ABSTRACT
Objective:
To compare the lung mechanics and outcomes between COVID-19-associated acute respiratory distress syndrome and non-COVID-19-associated acute respiratory distress syndrome.
Methods:
We combined data from two randomized trials in acute respiratory distress syndrome, one including only COVID-19 patients and the other including only patients without COVID-19, to determine whether COVID-19-associated acute respiratory distress syndrome is associated with higher 28-day mortality than non-COVID-19 acute respiratory distress syndrome and to examine the differences in lung mechanics between these two types of acute respiratory distress syndrome.
Results:
A total of 299 patients with COVID-19-associated acute respiratory distress syndrome and 1,010 patients with non-COVID-19-associated acute respiratory distress syndrome were included in the main analysis. The results showed that non-COVID-19 patients used higher positive end-expiratory pressure (12.5cmH2O; SD 3.2 versus 11.7cmH2O SD 2.8; p < 0.001), were ventilated with lower tidal volumes (5.8mL/kg; SD 1.0 versus 6.5mL/kg; SD 1.2; p < 0.001) and had lower static respiratory compliance adjusted for ideal body weight (0.5mL/cmH2O/kg; SD 0.3 versus 0.6mL/cmH2O/kg; SD 0.3; p = 0.01). There was no difference between groups in 28-day mortality (52.3% versus 58.9%; p = 0.52) or mechanical ventilation duration in the first 28 days among survivors (13 [IQR 5 – 22] versus 12 [IQR 6 – 26], p = 0.46).
Conclusion:
This analysis showed that patients with non-COVID-19-associated acute respiratory distress syndrome have different lung mechanics but similar outcomes to COVID-19-associated acute respiratory distress syndrome patients. After propensity score matching, there was no difference in lung mechanics or outcomes between groups.
Keywords:Coronavirus infectionsCOVID-19Critical careCritical care outcomesRespiratory distress syndromeRespiratory mechanicsSee more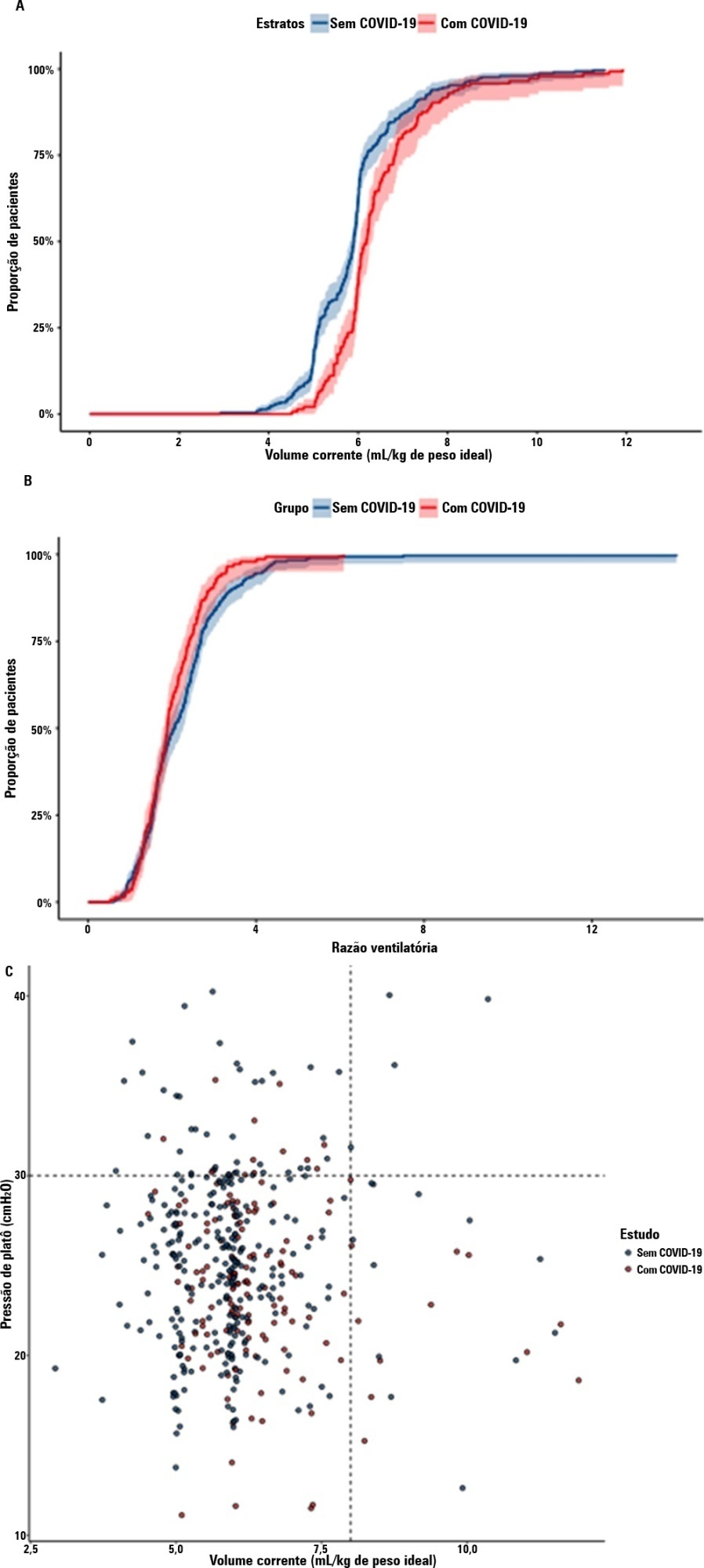
-
Original Article
Satisfaction of family members of critically ill patients admitted to a public hospital intensive care unit and correlated factors
Rev Bras Ter Intensiva. 2019;31(2):147-155
Abstract
Original ArticleSatisfaction of family members of critically ill patients admitted to a public hospital intensive care unit and correlated factors
Rev Bras Ter Intensiva. 2019;31(2):147-155
DOI 10.5935/0103-507X.20190024
Views1See moreABSTRACT
Objective:
To analyze the satisfaction, medical situation understanding and symptoms of anxiety and depression in family members of patients admitted to the intensive care unit.
Methods:
The family members of patients who were hospitalized for ≥ 72 hours were invited to participate in the study, which was performed in a public hospital. Questionnaires were answered to assess the understanding of the diagnosis, treatment and prognosis, and the support received in the intensive care unit. The family needs were also evaluated using a modified version of the Critical Care Family Needs Inventory (CCFNI). The Hospital Anxiety and Depression Scale (HADS) was used to assess the symptoms of anxiety and depression.
Results:
A total of 35 family members were interviewed within the patients’ first week of stay in the intensive care unit. Most patients (57.1%) were male, aged 54 ± 19 years. Sepsis was the main reason for admission to the intensive care unit (40%); the median of the Simplified Acute Physiology Score (SAPS) 3 was 68 (48 – 77), and 51.4% of the patients died in the intensive care unit. The majority of the family members were female (74.3%) and were sons or daughters of patients (54.3%), with a mean age of 43.2 ± 14 years. Overall, 77.1% of the family members were satisfied with the intensive care unit. A total of 37.1% of the family members did not understand the prognosis. Receiving clear and complete information in the intensive care unit and the doctor being accessible were factors that were significantly correlated with the overall family satisfaction. The prevalence of symptoms of anxiety (60%) and depression (54.3%) in the family members was high.
Conclusion:
The emotional distress of family members is high during a patient’s hospitalization in the intensive care unit, although satisfaction is also high. Clear and complete information provided by the intensivist and the support received in the intensive care unit are significantly correlated with the satisfaction of family members in a public hospital.
-
Original Article
Sex and spouse conditions influence symptoms of anxiety, depression, and posttraumatic stress disorder in both patients admitted to intensive care units and their spouses
Rev Bras Ter Intensiva. 2018;30(1):35-41
Abstract
Original ArticleSex and spouse conditions influence symptoms of anxiety, depression, and posttraumatic stress disorder in both patients admitted to intensive care units and their spouses
Rev Bras Ter Intensiva. 2018;30(1):35-41
DOI 10.5935/0103-507X.20180004
Views1See moreABSTRACT
Objectives:
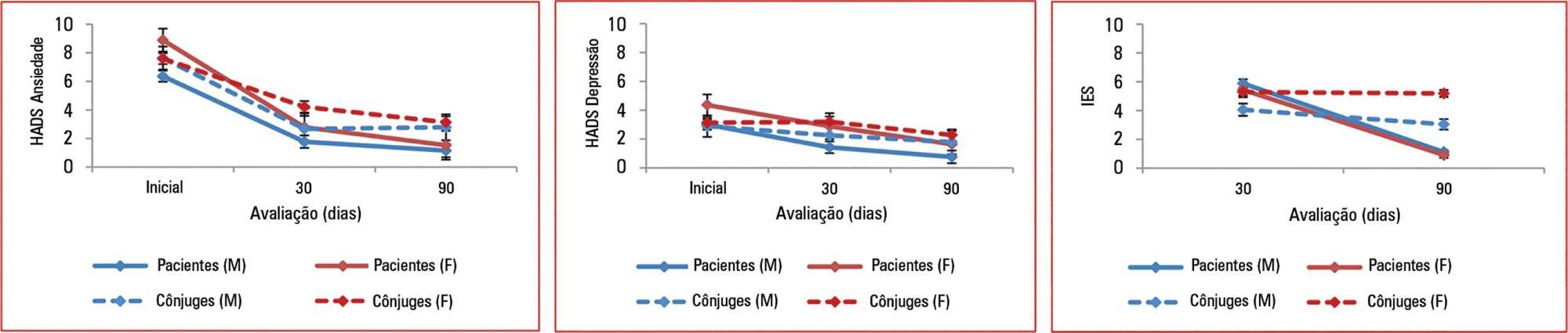
To assess the effect of sex and spouse condition on symptoms of anxiety, depression and posttraumatic stress symptoms in patients and their spouses.
Methods:
A prospective study conducted in a 22-bed adult mixed intensive care unit in a tertiary hospital in São Paulo, Brazil. Patients and their spouses were enrolled 2 days after intensive care unit admission. They were interviewed while in the intensive care unit using the Hospital Anxiety and Depression Scale. At 30 and 90 days after intensive care unit discharge, they completed the Impact of Event Scale and Hospital Anxiety and Depression Scale by phone.
Results:
From March 2011 to March 2013, we analyzed 118 patients and their spouses. We observed that female sex was associated with higher scores than male sex was in terms of the anxiety Hospital Anxiety and Depression Scale – subscale (p = 0.032) and depression (p = 0.034). There was no association between sex and posttraumatic stress disorder symptoms. However, spouses had higher Impact of Event Scale points compared with patients (p = 0.001).
Conclusions:
Female sex was associated with anxiety and depression, and spouses were more vulnerable to post-traumatic stress symptoms than the patients were. Increasing age and a later time of assessment were also associated with lower scores on the Impact of Event Scale.
-
Original Articles
Limitation to Advanced Life Support in patients admitted to intensive care unit with integrated palliative care
Rev Bras Ter Intensiva. 2016;28(3):294-300
Abstract
Original ArticlesLimitation to Advanced Life Support in patients admitted to intensive care unit with integrated palliative care
Rev Bras Ter Intensiva. 2016;28(3):294-300
DOI 10.5935/0103-507X.20160042
Views1See moreABSTRACT
Objective:
To estimate the incidence of limitations to Advanced Life Support in critically ill patients admitted to an intensive care unit with integrated palliative care.
Methods:
This retrospective cohort study included patients in the palliative care program of the intensive care unit of Hospital Paulistano over 18 years of age from May 1, 2011, to January 31, 2014. The limitations to Advanced Life Support that were analyzed included do-not-resuscitate orders, mechanical ventilation, dialysis and vasoactive drugs. Central tendency measures were calculated for quantitative variables. The chi-squared test was used to compare the characteristics of patients with or without limits to Advanced Life Support, and the Wilcoxon test was used to compare length of stay after Advanced Life Support. Confidence intervals reflecting p ≤ 0.05 were considered for statistical significance.
Results:
A total of 3,487 patients were admitted to the intensive care unit, of whom 342 were included in the palliative care program. It was observed that after entering the palliative care program, it took a median of 2 (1 – 4) days for death to occur in the intensive care unit and 4 (2 – 11) days for hospital death to occur. Many of the limitations to Advanced Life Support (42.7%) took place on the first day of hospitalization. Cardiopulmonary resuscitation (96.8%) and ventilatory support (73.6%) were the most adopted limitations.
Conclusion:
The contribution of palliative care integrated into the intensive care unit was important for the practice of orthothanasia, i.e., the non-extension of the life of a critically ill patient by artificial means.
-
Original Articles
Is the ICU staff satisfied with the computerized physician order entry? A cross-sectional survey study
Rev Bras Ter Intensiva. 2014;26(1):1-6
Abstract
Original ArticlesIs the ICU staff satisfied with the computerized physician order entry? A cross-sectional survey study
Rev Bras Ter Intensiva. 2014;26(1):1-6
DOI 10.5935/0103-507X.20140001
Views1Objective:
To evaluate the satisfaction of the intensive care unit staff with a computerized physician order entry and to compare the concept of the computerized physician order entry relevance among intensive care unit healthcare workers.
Methods:
We performed a cross-sectional survey to assess the satisfaction of the intensive care unit staff with the computerized physician order entry in a 30-bed medical/surgical adult intensive care unit using a self-administered questionnaire. The questions used for grading satisfaction levels were answered according to a numerical scale that ranged from 1 point (low satisfaction) to 10 points (high satisfaction).
Results:
The majority of the respondents (n=250) were female (66%) between the ages of 30 and 35 years of age (69%). The overall satisfaction with the computerized physician order entry scored 5.74±2.14 points. The satisfaction was lower among physicians (n=42) than among nurses, nurse technicians, respiratory therapists, clinical pharmacists and diet specialists (4.62±1.79 versus 5.97±2.14, p<0.001); satisfaction decreased with age (p<0.001). Physicians scored lower concerning the potential of the computerized physician order entry for improving patient safety (5.45±2.20 versus 8.09±2.21, p<0.001) and the ease of using the computerized physician order entry (3.83±1.88 versus 6.44±2.31, p<0.001). The characteristics independently associated with satisfaction were the system's user-friendliness, accuracy, capacity to provide clear information, and fast response time.
Conclusion:
Six months after its implementation, healthcare workers were satisfied, albeit not entirely, with the computerized physician order entry. The overall users’ satisfaction with computerized physician order entry was lower among physicians compared to other healthcare professionals. The factors associated with satisfaction included the belief that digitalization decreased the workload and contributed to the intensive care unit quality with a user-friendly and accurate system and that digitalization provided concise information within a reasonable time frame.
Keywords:Attitude of health personnelHealth care surveysJob satisfactionMedical order entry systemPhysician practice patternsSee more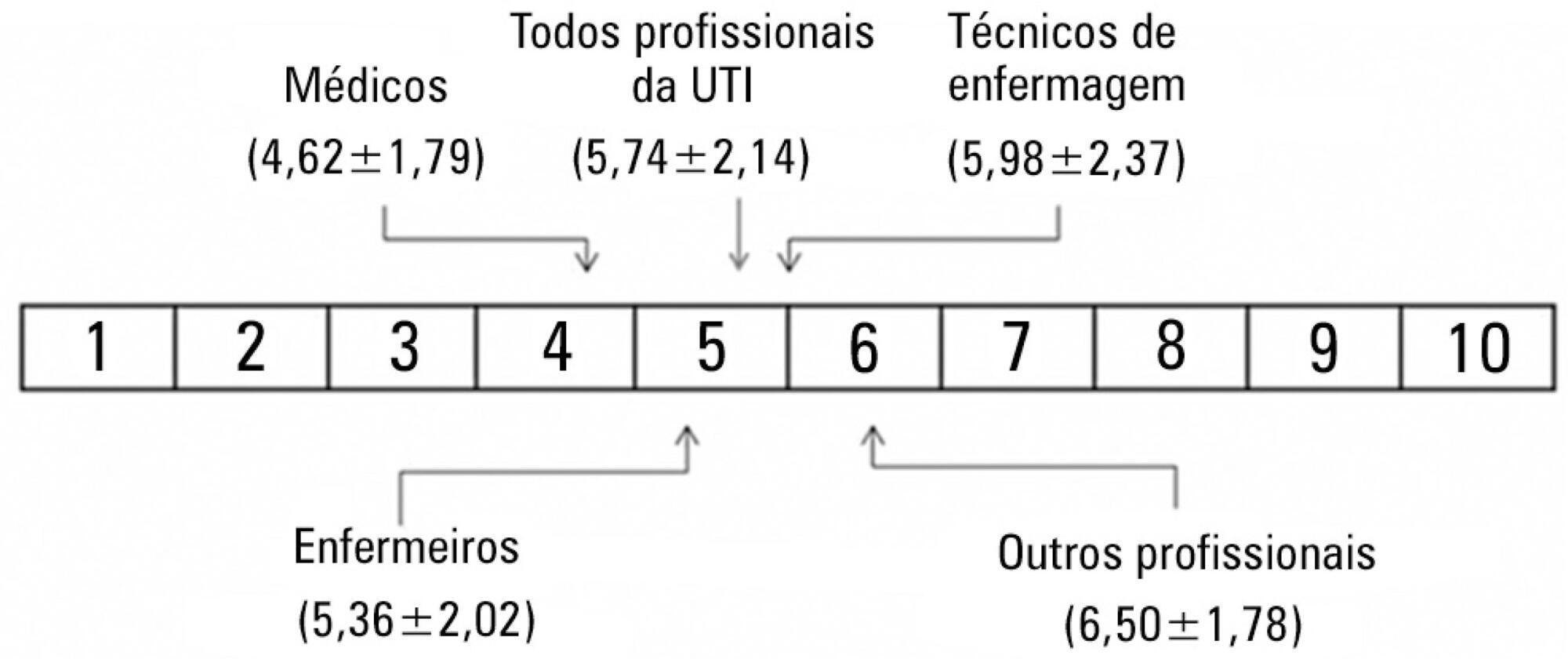
-
Original Articles
Intensive care unit visitation policies in Brazil: a multicenter survey
Rev Bras Ter Intensiva. 2014;26(4):339-346
Abstract
Original ArticlesIntensive care unit visitation policies in Brazil: a multicenter survey
Rev Bras Ter Intensiva. 2014;26(4):339-346
DOI 10.5935/0103-507X.20140052
Views0Objective:
This study aimed to determine which visitation policy was the most predominant in Brazilian intensive care units and what amenities were provided to visitors.
Methods:
Eight hundred invitations were sent to the e-mail addresses of intensivist physicians and nurses who were listed in the research groups of the Brazilian Association of Intensive Care Network and the Brazilian Research in Intensive Care Network. The e-mail contained a link to a 33-item questionnaire about the profile of their intensive care unit.
Results:
One hundred sixty-two questionnaires from intensive care units located in all regions of the country, but predominantly in the Southeast and South (58% and 16%), were included in the study. Only 2.6% of the intensive care units reported having liberal visitation policies, while 45.1% of the intensive care units allowed 2 visitation periods and 69.1% allowed 31-60 minutes of visitation per period. In special situations, such as end-of-life cases, 98.7% of them allowed flexible visitation. About half of them (50.8%) did not offer any bedside amenities for visitors. Only 46.9% of the intensive care units had a family meeting room, and 37% did not have a waiting room.
Conclusion:
Restrictive visitation policies are predominant in Brazilian intensive care units, with most of them allowing just two periods of visitation per day. There is also a lack of amenities for visitors.
Keywords:Intensive care units/standardsPatient-centered-care/standardsProfessional-family relationsProfessional-patient relationsQuestionnairesVisitors to patientsSee more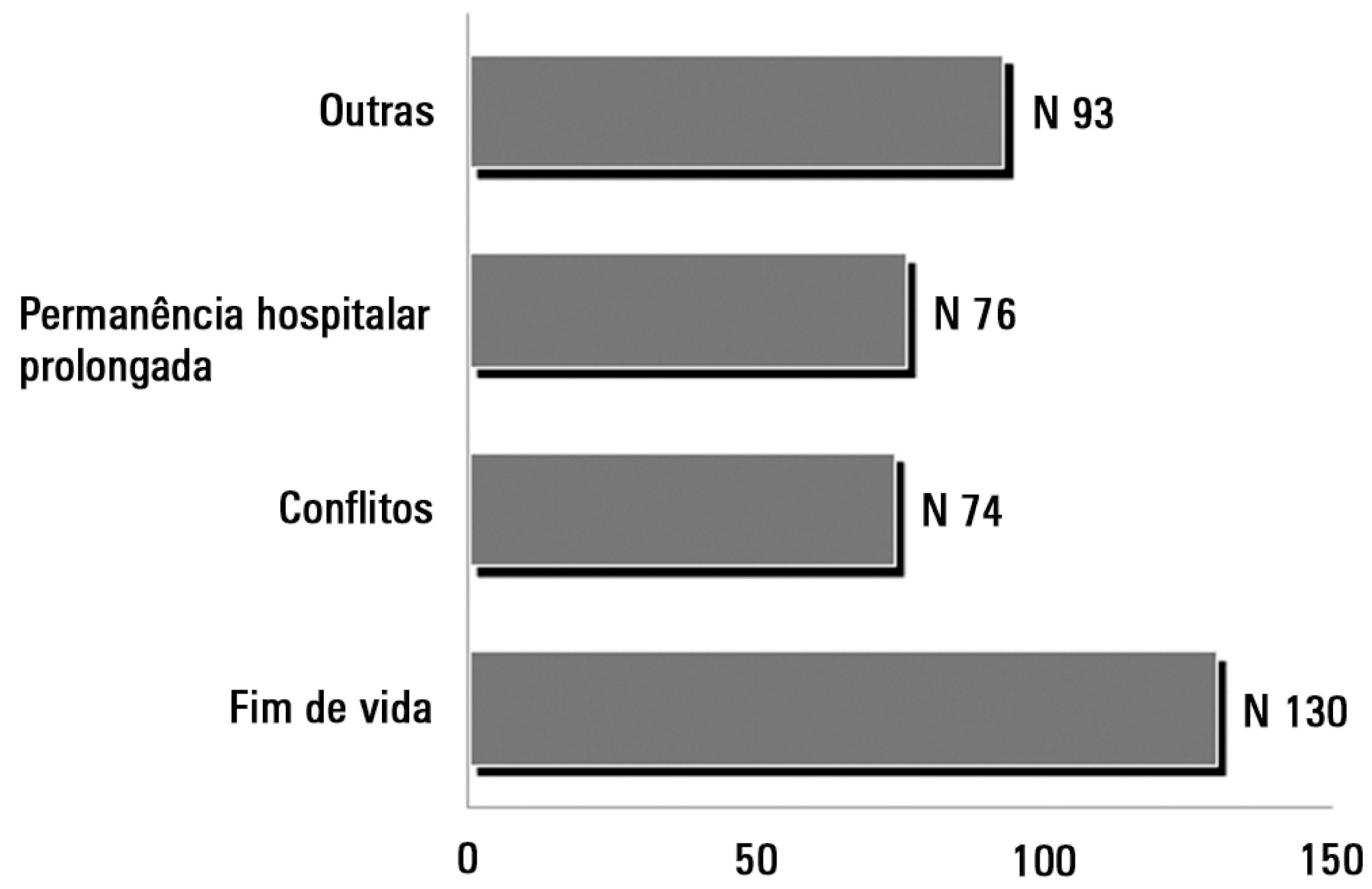
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




